Employee medical self-care programs reduce spending: SHRM speaker
Originally posted June 23, 2014 by Sheena Harrison on www.businessinsurance.com.
ORLANDO, Fla. — Medical self-care programs that teach employees which symptoms can be treated at home and which need medical attention can help reduce unnecessary medical spending for workers and employers, said Don R. Powell, president and CEO of the American Institute for Preventive Medicine in Farmington Hills, Michigan.
Mr. Powell gave a presentation Monday about the characteristics of best-in-class wellness programs during the Society for Human Resource Management's Annual Conference & Exposition in Orlando, Florida.
He said about 25% of physician visits each year are unnecessary, equaling about $227 million in excess medical costs for workers and employers, and 55% of emergency room visits are unnecessary, resulting in $65.6 million in extra costs to treat medical problems that are not urgent.
Employers should provide printed employee resource guides and websites that employees can use to evaluate whether their medical symptoms can be treated at home, whether they should visit a doctor and what questions to ask when they visit a physician, Mr. Powell said. Such guides typically include an easy-to-use flow chart that employees can follow to determine whether they need immediate medical care.
In addition to resource guides, Mr. Powell said some companies offer a nurse advice hotline to employees to discuss whether their symptoms need medical care.
Usage and ROI
Mr. Powell noted that printed self-care resource guides, which cost about $5 to $8 per copy, are more likely to be used by employees of all ages than websites or nurse hotlines when considering the urgency of a medical problem. However, he said, offering a variety of delivery methods — as well as communicating the program’s availability through newsletters, emails and posters — can make employees more likely to use self-care programs.
Companies see anywhere from a 3-1 to a 15-1 return on investment for every dollar spent on medical self-care programs, Mr. Powell said.
“You're cutting into those unnecessary doctor and ER visits,” he said. “If you're a self-funded company ... that's $199 per visit to $350 per ER visit right back into your pocket, so you stand to gain the most. Not to say a company that’s fully insured doesn't stand to gain, because it allows employees not to miss work when they’re at the doctor or ER unnecessarily and because people really appreciate a medical self-care program.”
Other factors in successful wellness programs include having corporate leaders and employee peers involved in such initiatives, making it easy for workers to participate in wellness initiatives and health coaching to program participants, Mr. Powell said.
American Workers More Physically than Financially Fit
Originally posted April 22, 2014 by Lisa Barron on https://www.benefitspro.com
American employees see themselves as more physically fit (57 percent) than financially fit (28 percent), according to new research from the Principal Financial Well-Being Index: American workers.
The vast majority (84 percent), however, also believe that maintaining physical fitness is an investment in their financial future.
Still, nearly half of workers (46 percent) are stressed about their current financial situation. Fifty-one percent of Gen Y workers are stressed about finances compared to 35 percent of baby boomers. And those working with a financial advisor were less likely (33 percent) to be stressed about their financial future.
"American workers recognize the long-term financial benefits of staying healthy, but financial stress is often a constant pressure that can have a significant impact on their physical health," said Luke Vandermillen, vice president at the Principal Financial Group.
"With spring in full swing, now is a good time for Americans to apply their good fitness habits to their financial lives as well. Mark some time on the calendar for financial spring cleaning."
More than half (52 percent) say they have monitored their spending levels in the past year. Thirty-nine percent created a budget to keep finances in check, up from 28 percent two years ago.
Fifty-seven percent have an emergency fund in place, with those working with a financial profession about 1.5 times more likely to have one.
"It's encouraging to see American workers planning for unforeseen hurdles by giving themselves a financial checkup and setting aside money in an emergency fund," said Vandermillen.
"Despite a few missteps, like using the fund on monthly bills, these positive behaviors show individuals are making strides and taking personal responsibility to improve their short and long-term financial well-being."
The Principal Financial Well-Being Index: American Workers was conducted online among 1,123 employees at small and mid-sized businesses from Feb. 4-12.
76 Percent of Workforce is Tired Most Weekdays
Originally posted April 15, 2014 on www.ifebp.org.
The Virgin Pulse Institute, an evidence-based organization that puts research to work to help employees and companies thrive, today announced the results of a study designed to better understand employees' sleep disturbances and offer actionable insight to both employers and their workforce. The research outlines why employers supporting sleep programs increase employee productivity, and how these programs help employees feel more appreciated and supported.
Leveraging an online sleep program from vielife, the Virgin Pulse Institute conducted a sleep study in November 2013 with approximately 1,140 employees, all Virgin Pulse members, from three U.S.-based companies. Researchers found that:76 percent of employees felt tired most days of the week40 percent of employees doze off during the day once per month30 percent of employees were unhappy or very unhappy with the quality or quantity of their sleep15 percent doze off during the day at least once per week to once per day.
Dr. Jennifer Turgiss, a co-author of the study and director of the Virgin Pulse Institute, said, "Showing up to work sleep deprived can be the equivalent of showing up to work intoxicated. Employees who don't sleep well have poorer concentration, poorer decision-making abilities, are significantly less able to cope with stressful situations, and are more likely to make unhealthy choices. The effects of poor sleep impair people's focus and motivation, preventing them from reaching their full potential. In attempts to encourage employees to live healthier, often employers - with the help of their health insurers or wellness vendors -focus on simply improving diet and exercise, but this approach ignores one critically important habit: sleep. With its direct link to dangerous health conditions and steep productivity losses, a well-rested workforce is critical to a company's success."
The Effect of Sleep Problems
The Centers for Disease Control and Prevention has called lack of sleep "an epidemic," linking it to motor vehicle crashes, industrial disasters and other occupational errors. Many other studies have found employees who sleep fewer than six hours per day are nearly 30 percent more likely to be overweight and have a whole host of health problems like hypertension, diabetes, depression and cancer. These people also take a tremendous cognitive hit on a daily basis - finding it difficult to concentrate at work or complete tasks, resulting in significantly lower productivity. Sleep disturbances cause fatigue-related productivity losses estimated at $1,967 per employee annually, according to a study published in the journal Sleep.
What Causes Sleep Problems?
The Virgin Pulse Institute study found four key themes keeping employees awake at night: worry/stress, mental activity, physical discomfort and environmental disruptors. Many factors within these categories kept participants awake, including:Temperature too high or too low (85.2%)Their partner (71.9%)Unwanted noise (68.6%)Light - too bright (52.8%)Mattress (40%)Young children (35.9%)Medical condition that disturbs sleep (10.2%)
Sleep deprivation was found to have impacts across four key areas: physical well-being; cognitive abilities and productivity; mood; and stress management. Lack of sleep leaves employees less focused on the job and unable to perform at their peak, and leaves them experiencing a decreased feeling of overall well-being, according to the Institute study.
Participants noted that lack of sleep impacted their energy and motivation to participate in physical activities and eat healthy foods. They experienced difficulty concentrating at work or remembering tasks, and felt more irritable at work and home. Sleeplessness also made it harder to manage stress, further impacting their difficulties sleeping. “I come in here in the morning and it's kind of hard to get motivated. I'll be yawning and carrying on and kind of drag for an hour or so before I'm really probably engaged and back doing real performance type of work I would say. So it will be easy for me to just kind of lag around, drink some coffee, walk around, talk to people, or sit at my desk and read Internet news rather than actually work," said one participant."[I would] blow up at the wrong thing or you blow up at the wrong kid or something. And you just go, oh, man. I should have been able to handle that one," said another participant. “And the other thing that I noticed when I go through the period where I have more lack of sleep, I feel more scatterbrained, like I have all of these things to do. And normally, I'm very organized and prioritize and will at least write a list, and everything goes out the window and I start forgetting to do things or bring this in the morning or things like that. And that really bothers me. I hate it when I drop a ball because I forgot something," said another participant. “I think there is a slow-down, in terms of getting tasks done, just because, again, your attention span isn't fully there. You might not be as with it," said another participant. “I probably have got a shorter fuse, a little grumpier," said a participant.
"Our study made one thing clear: lack of sleep is crippling America's workforce. Employers can't turn a blind eye. Whether they offer an online sleep program, encourage employees to use vacation days, or provide other tools, employers must address sleep issues in order to create a thriving workforce and business," said Turgiss. "Not only will employees be more rested, but they'll feel more supported by their employers, helping them perform better and become better able to engage in work and in life."
Employers’ Corporate Wellness Incentives Climb to New Heights
Originally posted February 20, 2014 by Michael Giardina on https://ebn.benefitnews.com
With a reported 15% increase in wellness incentive spending within their health care plans, corporate employers have their sights set on improving their workforce’s overall health in 2014 through wellness programs for both employees and their significant others, according to a new survey from Fidelity Investments and the National Business Group on Health.
The fifth annual study finds that corporate employers expect to spend an average of $594 per employee on wellness-based incentives, an increase from 2013’s $521 average. For smaller employers with less than 5,000 employees, the employee average reached $595, a $151 increase from levels reported in 2013.
Approximately 95% of employers plan to offer some sort of health improvement program, highlighting that benefit plan sponsors have labeled wellness programs as an integral part of their benefits program in this post-Affordable Care Act world. Also, 74% note that they offer incentives for employee participation, which is a 12% dip from last year.
“While the use and measurement of corporate wellness programs continue to evolve, it has become clear that many employers understand the value of – and are committed to – wellness-based incentives in their company health plan,” says Robert Kennedy, health and welfare practice leader with Fidelity’s benefits consulting business.
The most popular programs include lifestyle management courses that focus on physical activity, weight and stress management. Disease and care management programs – which look to manage chronic health conditions – were also favored.
Doling out for spouses/HSAs
From the 2014 survey, Fidelity and NBGH found that nearly four out of 10 employers disclosed that their plan will include options for spouses or domestic partners. Last year, results highlighted that 54% set out plans to expand wellness-based incentives to include dependents and roughly half said they were including spouses and dependents in wellness communications.
Average payouts for spouse and domestic partners are expected to reach $530 in 2014. Employers with more than 20,000 employees expect to spend an average of $611 on this group.
Other incentives such as heath savings accounts and flexible spending accounts were expected to incentivize more employees use. Roughly 34% list that they plant to contribute to these accounts in order to bolster disease or care management engagement and 30% hope these deposits will add to weight management programs participation.
“Based on the feedback from this year’s survey respondents, it’s obvious that wellness programs not only play a key role in many corporate health care plans today, but they’ll continue to be an integral part of corporate benefit programs in the future,” says Helen Darling, the retiring president and CEO of NBGH.
Stress continues to boil up in American adults: APA study
Originally posted February 12, 2014 by Michael Giardina on https://ebn.benefitnews.com
Are Americans accepting ways to cope with ever skyrocketing stress levels that can make them more productive to employers? New research finds that traditional pressures continue to rise and more needs to be done to relieve this strain.
The American Psychological Association’s annual survey, released Tuesday, finds that stress continues to plague American adults. According to its Stress in America report, 42% say that stress levels have increased and 36% state that these levels have remained constant over the past five-years.
On average, despite reporting that a healthy stress level is 3.6 on a 10-point scale, survey respondents state their stress level is 5.1. APA says that only 10% of these adults actually make time for stress management activities.
Dr. David Ballard, who heads up APA’s Center for Organizational Excellence, explains that in stress “there is a sizeable gap of what people think is healthy and what they are experiencing.”
Ballard notes stresses related to money, work and the economy seem to support this year’s growth among the 2,000 adults who participated in the nationwide study. While “not unusual,” Ballard says the industry needs to act.
“[Employers] have a workforce…trying to be productive and engaged [but] who is overwhelmed,” Ballard says. “To have more than two-thirds of their workforce say that work is a major source of stress for them, it’s clearly something that employers and employees alike need to deal with.”
Individual stress interventions such as relaxation trainings, meditation, exercise or yoga classes and teaching time management skills are just some options for employers.
“The organizations that do take steps to address work stress typically are focusing on individual-level intervention….but this individual level approach by itself typically won’t be enough to prevent the stress from occurring in the first place and keeping it from being a problem,” Ballard continues. “The key is adding…organizational level things that can be done because when you look at what work stress really is, it’s a mismatch between the demands that employees are facing to the resources that they have available to cope with those demands.”
Previously, in February 2013, APA found that 31% of Americans who categorize themselves as suffering from high stress never discuss stress management with their health care provider. Moreover, 32% of Americans say they believe it is very or extremely important to talk with their health care providers about stress management, but only 17% report that these conversations are happening often or always.
In this year’s study, APA lists that stress impacts both sleep and exercise habits. Ballard says that employers can get ahead of the curve by first instituting hiring practices that find individuals who are a “good fit for the job and the organization.” He adds that additional training and development can help to handle conflicts that arise from positions, ambiguity of work tasks and the handling of high workloads.
Also, employers should assess social and work environment issues that can address team compatibility and workplace organization from both the social and physical dynamic, he says.
“When organizations understand that the health of their workforce and the performance and success of the company are linked together, then they’ll take steps that are both for the wellbeing of the worker and for the organization’s performance,” Ballard explains. “This isn’t just about doing the right thing and taking care of your workers, that is all true and it’s important, but it’s also smart business.”
Making HSAs and wellness work together
Originally posted January 13, 2014 by Rose Rosa on https://ebn.benefitnews.com
Maximizing the positive impact of a wellness program is a goal of many employers. Much of the discussion around wellness focuses on how to increase employee participation. Doing so remains a challenge for many employers, but there are some innovative approaches employers are exploring.
One concept we’re seeing is tying wellness to health savings accounts. With a HSA, employees can use tax-free dollars to pay for qualified out-of-pocket healthcare expenses, typically including items such as eyeglasses or prescription medications. Now, some employers are expanding use of HSAs to drive wellness participation.
Combining wellness and HSAs is a long-term strategy. However, there can be some immediate benefit for the employer, which typically begins by going from a traditional fully insured plan to a high-deductible plan with a HSA, thereby saving the employer some money right out of the gate.
Here’s how tying a HSA to wellness can work: The employer funds or partially funds a HSA, which is the “carrot” to get employees interested in the account. Over time, some employers introduce the so-called “stick” to maximize participation by requiring employees to meet certain health-related criteria.
Here’s one possible approach:
• In the first year, the employer contributes to the employees’ HSA account (typically, a 50% contribution).
• To receive the 50% contribution in year two, employees are required to complete a health risk assessment.
• In year three, the employer will increase the requirements, perhaps including completion of another HRA, plus biometric testing.
By increasing the conditions that must be met, it creates a natural progression that helps employees become more aware of their health and to do something about any issues identified by the screening. It also demonstrates to employees what they need to do to control their personal health care costs; those who make progress get discounts on their plan, so they become more responsible for their own health and ultimately their own savings. As employees control their costs, they help control the employer’s costs as well.
In the end, it’s a win-win scenario; the combination of HSAs and wellness programs can provide value to both employees and employers. It’s also an effective way to guide beneficial behavior since employees who follow the program are more likely to take steps to become (or stay) healthy. Using this type of program can also be a good opportunity to tie in other health initiatives, such as smoking cessation. One approach is to apply a smokers’ surcharge on the employee contributions (the stick) while also offering smoking cessation programs to help the employee quit smoking (the carrot to avoid the stick).
To make this combined strategy work, education is a vital. HSAs are most effective if employees understand how the program works, so it’s the employer’s duty to teach them. With this approach, employees have greater risk and higher deductibles, but they also have greater control and choice, coupled with an incentive to be healthy. Essentially, this spurs the employee to become a more educated consumer of health care services.
But it’s up to the employer to make the first move.
Survey: Employees still under-informed on ACA, wellness
Originally posted November 8, 2013 by Tristan Lejeune on ebn.benefitnews.com
Only 15.1% of workers at large employers say they are “knowledgeable” or “very knowledgeable” about health care reform and the Affordable Care Act’s public exchanges, and nearly one in five can’t say for sure if their company has a wellness program or not, according a recent survey. The poll’s results, released this month, speak to a population that has confidence in the communication efforts of their benefits administrators, and that points out some serious shortfalls in that communication.
The survey, which spoke with 400 employees at companies with north of 2,000 each, found that only 29.5% could correctly identify times when they can make changes to their health plans, like open enrollment, according to the Jellyvison Labs. Jellyvision, which created ALEX, a virtual employee benefits counselor, says all but one of the employers involved in the survey offer health insurance, but employees still demonstrate large education gaps on their own benefits.
More than 90% of surveyed workers say it’s at least “somewhat important” to understand ACA and its implications, but less than a fifth actually consider themselves knowledgeable. The good news is employee confidence in their employers’ ability to communicate the necessary information is high: nearly 80% think their companies can properly bring them up to speed, and more than one in three rate their confidence levels on this point at eight or higher on a 10-point scale.
Some 77.6% of those polled agree that it is at least “somewhat important” for their organizations to offer a wellness program, but almost one-fifth don’t know with any certainty whether or not their company does so.
“One of the most important things we learned from this data,” says Josh Fosburg, vice president of business development for the Jellyvision Lab, “is employees aren’t getting everything they need to know about their employers’ wellness programs and other benefits. For instance, nearly half of employees in our survey think they have to pay something in order to take advantage of the wellness programming that will help them manage their weight, stay on top of their prescribed medications, or cease smoking. That’s bananas.”
Jellyvision says employers need to “up their communications game” in order to help employees take advantage of everything included in their benefits offerings.
Doctors urged to treat obesity like any other ailment; New guidelines say do whatever it takes to get the pounds off
Originally posted November 13, 2013 by Nanci Hellmich on www6.lexisnexis.com
There's no ideal diet that's right for everyone, but that shouldn't stop the nation's doctors from helping their heavy patients battle weight issues as aggressively as things like blood pressure, according to new obesity treatment guidelines released Tuesday.
The guidelines, from three leading health groups, say that doctors need to help obese patients figure out the best plan, whether it's a vegetarian diet, low-sodium plan, commercial weight-loss program or a low-carb diet.
Still, the most effective behavior-change weight-loss programs include two to three in-person meetings a month for at least six months, and most people should consume at least 500 fewer calories a day to lose weight, the recommendations say.
The guidelines are designed to help health care providers aggressively tackle the obesity epidemic. "The overall objective is quite a tall order: to get primary care practitioners to own weight management as they own hypertension management," says obesity researcher Donna Ryan, co-chairwoman of the committee writing these guidelines for the Obesity Society, American Heart Association and American College of Cardiology.
The recommendations are part of a set of heart disease prevention guidelines released Tuesday.
Nearly 155 million U.S. adults are overweight or obese, which is roughly 35 pounds over a healthy weight. Extra pounds put people at a higher risk of heart disease, stroke, many types of cancer, type 2 diabetes and a host of other health problems.
Health care providers should encourage obese and overweight patients who need to drop pounds for health reasons to lose at least 5% to 10% of their weight by following a moderately reduced-calorie diet suited to their food tastes and health status, while being physically active and learning behavioral strategies.
"The gold standard is an intervention delivered by trained interventionists (not just registered dietitians or doctors) for at least 14 sessions in the first six months and then continue therapy for a year," says Ryan, a professor emeritus at the Pennington Biomedical Research Center in Baton Rouge. If this kind of intensive therapy is not available, then other types of treatment, such as commercial weight-loss programs or telephone and Web-based programs, are good "second choices," she says.
Medicare began covering behavioral counseling for obese patients last year, and under the Affordable Care Act, most private insurance companies are expected to cover behavioral counseling and other obesity treatments by next year.
"There is no ideal diet for weight loss, and there is no superiority between the many diets we looked at," Ryan says. "We examined about 17 different weight-loss diets."
Pat O'Neil, director of the Weight Management Center at Medical University of South Carolina, says, "The diet you follow is the one that's going to work for you. That's good information for the public to have."
The report advises health care providers to calculate body mass index (a number that takes into account height and weight) at annual visits or more frequently, and use it to identify adults who may be at a higher risk of heart disease and stroke. Evidence shows that the greater the BMI, the higher the risk of coronary heart disease, stroke, type 2 diabetes and death from any cause, the report says. "BMI is a quick and easy first step," Ryan says.
The guidelines are being published simultaneously in Circulation, a journal of the American Heart Association; the Journal of the American College of Cardiology; and Obesity: Journal of the Obesity Society.
6 wellness tips for flu prevention
Originally posted on benefitnews.com
The flu costs businesses approximately $10.4 billion in direct costs for hospitalizations and out-patient visits for adults, according to the Centers for Disease Control and Prevention. In addition to encouraging workers to get immunized, employers can further minimize employee sick days and slow the spread of illness by communicating best practices in wellness and nutrition. Share these six preventive tips from Dr. Bruce Underwood, a certified nutrition and preventive care specialist with Healthy Futures, Inc., to keep workers and their families healthy this season.
No matter whether an individual decides to get immunized for influenza, primary prevention should be their priority for avoiding illness. Dr. Underwood explains that a good basis for our immune system is to get a good night’s sleep, generally between six to eight hours every night.
The surgeon general recommends all adults walk at least 10,000 steps or about 4 miles every day. If we over-exercise, then our immune system is weakened for a few days, explains Underwood. However, if we don't exercise at all our immune system is also weak.
As the following three slides prove, we need vitamins, minerals, amino acids, and fatty acids for our bodies to work well. Overall, Underwood recommends eating a wide variety of foods in amounts that allow you to maintain an ideal body weight.
One of the most important vitamins for immune health is vitamin C. The upper safe limit for Vitamin C is 2,000 mg for adults, according to the National Institute of Health. Underwood and other experts recommend 1,000 mg of the vitamin as a good daily dose. Dietary sources of the vitamin come mainly from fruits and vegetables, but can also be found in certain cuts of meat, especially liver. Studies have shown that our bodies expend Vitamin C to mitigate toxins such as cigarette smoke and pollution. The antioxidant has also helps relieve the physical and psychological effects of stress on people.
5. Zinc
The mineral Zinc is also necessary in stressful situations. By ingesting 10 to 40 milligrams of Zinc each day, individuals can also help build up their immune system. Underwood advises people to keep their daily dosage under 100 mg per day, however, as too much of the metal might cause fever, coughing, stomach pain, fatigue, and many other problems. Meats, seafood, dairy products, nuts, legumes, and whole grains offer relatively high levels of zinc.
U.S. Obesity Rate Climbing in 2013
Originally posted November 1, 2013 by Lindsey Sharpe on https://www.gallup.com
WASHINGTON, D.C. -- The adult obesity rate so far in 2013 is 27.2%, up from 26.2% in 2012, and is on pace to surpass all annual average obesity rates since Gallup-Healthways began tracking in 2008.
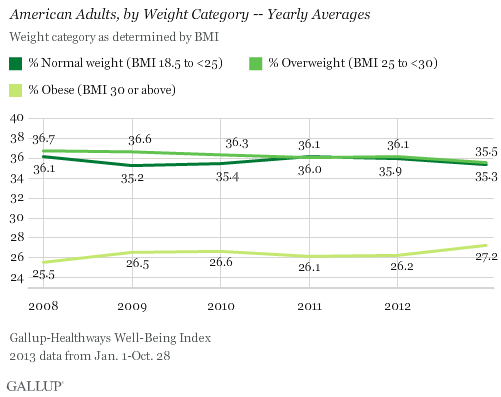
The one-percentage-point uptick in the obesity rate so far in 2013 is statistically significant and is the largest year-over-year increase since 2009. The higher rate thus far in 2013 reverses the lower levels recorded in 2011 and 2012, and is much higher than the 25.5% who were obese in 2008.
The increase in obesity rate is accompanied by a slight decline in the percentage of Americans classified as normal weight or as overweight but not obese. The percentage of normal weight adults fell to 35.3% from 35.9% in 2012, while the percentage of adults who are overweight declined to 35.5% from 36.1% in 2012. An additional 1.9% of Americans are classified as underweight in 2013 so far.
Since 2011, U.S. adults have been about as likely to be classified as overweight as normal weight. Prior to that, Americans were most commonly classified as overweight.
Gallup and Healthways began tracking Americans' weight in 2008. The 2013 data are based on more than 141,000 interviews conducted from Jan. 1 through Oct. 28 as part of the Gallup-Healthways Well-Being Index. Gallup uses respondents' self-reported height and weight to calculate body mass index (BMI) scores. Individual BMI values of 30 or above are classified as "obese," 25 to 29.9 are "overweight," 18.5 to 24.9 are "normal weight," and 18.4 or less are "underweight."
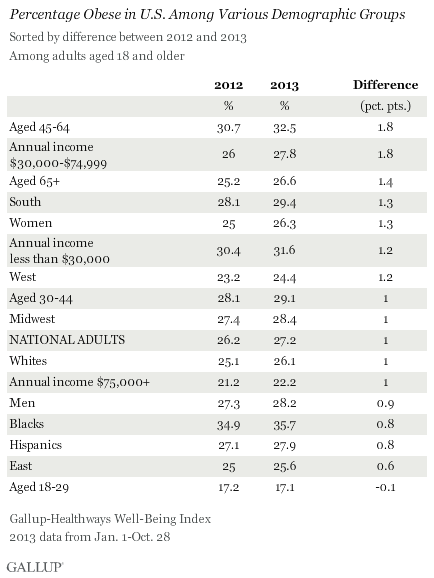
Obesity Rates Increase Across Almost All Demographic Groups
Obesity rates have increased at least slightly so far in 2013 across almost all major demographic and socioeconomic groups. One exception is 18- to 29-year-olds, among whom the percentage who are obese has remained stable. The largest upticks between 2012 and 2013 were among those aged 45 to 64 and those who earn between $30,000 and $74,999 annually. The obesity rate within both groups increased by 1.8 points, which exceeds the one-point increase in the national average.
At 35.7%, blacks continue to be the demographic group most likely to be obese, while those aged 18 to 29 and those who earn over $75,000 annually continue to be the least likely to be obese.
Bottom Line
The U.S. obesity rate thus far in 2013 is trending upward and will likely surpass all annual obesity levels since 2008, when Gallup and Healthways began tracking. It is unclear why the obesity rate is up this year, and the trend since 2008 shows a pattern of some fluctuation. This underscores the possibility that that the recent uptick is shorter-term, rather than a more permanent change. Still, if the current trend continues for the next several years, the implications for the health of Americans and the increased burden on the healthcare system could be significant.
Blacks, those who are middle-aged, and lower-income adults continue to be the groups with the highest obesity rates. The healthcare law could help reduce obesity among low-income Americans if the uninsuredsign up for coverage and take advantage of the free obesity screening and counseling that most insurance companies are required to provide under the law.
Employers can also take an active role to help lower obesity rates. Gallup has found that the annual cost for lost productivity due to workers being above normal weight or having a history of chronic conditions ranges from $160 million among agricultural workers to $24.2 billion among professionals. Thus, employers can cut healthcare costs by developing and implementing strategies to help workers maintain or reach a healthy weight.
Gallup has also found that employees who are engaged in their work eat healthier and exercise more. Therefore, employers who actively focus on improving engagement may see healthier and more productive workers, in addition to lower healthcare costs.
About the Gallup-Healthways Well-Being Index
The Gallup-Healthways Well-Being Index tracks well-being in the U.S. and provides best-in-class solutions for a healthier world. To learn more, please visit well-beingindex.com.
Results are based on telephone interviews conducted as part of the Gallup-Healthways Well-Being Index survey Jan. 1-Oct. 28, 2013, with a random sample of 141,935 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
For results based on the total sample of national adults, one can say with 95% confidence that the margin of sampling error is ±0.5 percentage points.
Interviews are conducted with respondents on landline telephones and cellular phones, with interviews conducted in Spanish for respondents who are primarily Spanish-speaking. Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by region. Landline and cellphone numbers are selected using random-digit-dial methods. Landline respondents are chosen at random within each household on the basis of which member had the most recent birthday.
Samples are weighted to correct for unequal selection probability, nonresponse, and double coverage of landline and cell users in the two sampling frames. They are also weighted to match the national demographics of gender, age, race, Hispanic ethnicity, education, region, population density, and phone status (cellphone only/landline only/both, and cellphone mostly). Demographic weighting targets are based on the March 2012 Current Population Survey figures for the aged 18 and older U.S. population. Phone status targets are based on the July-December 2011 National Health Interview Survey. Population density targets are based on the 2010 census. All reported margins of sampling error include the computed design effects for weighting.
In addition to sampling error, question wording and practical difficulties in conducting surveys can introduce error or bias into the findings of public opinion polls.
For more details on Gallup's polling methodology, visit www.gallup.com.
