Almost Half Of Workers Don’t Know What Impact Affordable Care Act Will Have On Them
Originally posted November 06, 2013 on https://www.insurancebroadcasting.com
Online resources cited as most reliable source of information about law
COLUMBIA, S.C.--(BUSINESS WIRE)--A survey conducted online by Harris Interactive on behalf of Colonial Life & Accident Insurance Company shows nearly half of American workers don’t feel knowledgeable about how the Affordable Care Act will impact them personally.
“Despite all the attention the Affordable Care Act has received in the past few years, nearly half of American workers still say they don’t know much about it”
In a poll of more than 1,000 U.S. employees (full-time and/or part-time)1, 47 percent of workers say they are not very knowledgeable or not at all knowledgeable about the impact the Affordable Care Act will have on them. Thirty-three percent say they’re not very knowledgeable about the law and its proposed personal impact, and 14 percent say they’re not at all knowledgeable.
“Despite all the attention the Affordable Care Act has received in the past few years, nearly half of American workers still say they don’t know much about it,” says Steve Bygott, assistant vice president of core market services at Colonial Life.
In other survey findings, 48 percent of workers say federal government websites are the most reliable source of information about the ACA and its personal impact on them. They rated internet or other online news sources as the next most reliable, cited by 44 percent of employees. Other sources viewed as reliable options include:
Their employers or HR departments
36 percent
Insurance company websites or literature
30 percent
TV news programs
25 percent
Printed magazines or newspapers
20 percent
Family or friends
18 percent
Other
8 percent
“Workers clearly need help understanding this law and its personal impact on them and their families,” says Bygott. “Because employers are viewed as one of the top three sources of reliable information on this topic, they have a tremendous opportunity to help their workers get the information they need when they communicate their benefits programs.”
Survey results were included as part of a white paper recently published by Colonial Life called “Beyond Health Care Reform.” The research paper outlines what employers should know about health care reform, employee benefits and the subsequent need for increased benefits education.
Survey Methodology
This survey was conducted online within the United States by Harris Interactive on behalf of Colonial Life from September 3-5, 2013 among 2,046 adults ages 18 and older, among whom 1,023 are employed full-time or part-time. This online survey is not based on a probability sample and therefore no estimate of theoretical sampling error can be calculated. For complete survey methodology, including weighting variables, please contact Jeanna Moffett at Colonial Life at JMoffett@ColonialLife.com.
1 Online survey conducted within the United States for Colonial Life & Accident Insurance Company by Harris Interactive, Sept. 3-5, 2013, among 2,046 U.S. adults age 18 and older, among whom 1,023 are employed full-time or part-time.
IRS Releases Tax Benefit Inflation Adjustments for 2014
Originally posted https://www.ifebp.org
Internal Revenue Service (IRS) Revenue Procedure 2013-35 provides the cost-of-living adjustments to certain items for 2014 as required under the Internal Revenue Code. This revenue procedure includes updates for numerous items including:
Adoption Assistance Programs
For taxable years beginning in 2014, under § 137(a)(2) the amount that can be excluded from an employee’s gross income for the adoption of a child with special needs is $13,190. Under § 137(b)(1) the maximum amount that can be excluded for amounts paid or expenses incurred by an employer for qualified adoption expenses furnished through an adoption assistance program for other adoptions by the employee is $13,190. The amount excludable from gross income begins to phase out for taxpayers with modified adjusted gross income in excess of $197,880 and completely phases out with modified adjusted gross income of $237,880 or more.
Health Flexible Spending Arrangements (Health FSA)
The Affordable Care Act amended § 125 to provide limitations on Health FSAs. The dollar limitation on voluntary employee salary reductions for a health FSA is adjusted for inflation for taxable years beginning after December 31, 2013. For taxable years beginning in 2014, the dollar limitation is $2,500.
Medical Savings Accounts
- Self-only coverage. For taxable years beginning in 2014, the term "high deductible health plan" as defined in § 220(c)(2)(A) means, for self-only coverage, a health plan with an annual deductible not less than $2,200 and not more than $3,250, and under which the annual out-of-pocket expenses required to be paid (other than for premiums) for covered benefits do not exceed $4,350.
- Family coverage. For taxable years beginning in 2014, the term "high deductible health plan" means, for family coverage, a health plan with an annual deductible not less than $4,350 and not more than $6,550, and under which the annual out-of-pocket expenses required to be paid (other than for premiums) for covered benefits do not exceed $8,000.
Qualified Transportation Fringe Benefit
For taxable years beginning in 2014, the monthly limitation under § 132(f)(2)(A) regarding the aggregate fringe benefit exclusion amount for transportation in a commuter highway vehicle and any transit pass is $130. The monthly limitation under § 132(f)(2)(B) regarding the fringe benefit exclusion amount for qualified parking is $250.
Cost of benefits, ACA compliance main concerns of midsized businesses
Originally posted by Andrea Davis on https://ebn.benefitnews.com
The cost of health coverage, the Affordable Care Act and the volume of government regulations are the top three concerns of midsized business owners and executives, according to a new survey from the ADP Research Institute.
Seventy percent of midsized businesses – those with between 50 and 999 employees – surveyed said their biggest challenge in 2013 is the cost of health coverage and benefits. ACA legislation came in as the No. 2 concern, cited by 59%, a 16% increase over last year. And rounding out the top three list of concerns was the level and volume of government regulations, cited by 54%.
“What was a surprise to us was that midsized business owners’ level of confidence in their ability to comply with the laws and regulations doesn’t reflect reality,” says Jessica Saperstein, division vice president of strategy and business development at ADP.
For example, the survey finds that, overall, 83% of midsized businesses are confident they’re compliant with payroll tax laws and regulations, nearly one-third reported unintended expenses – fines, penalties or lawsuits – as a result of not being compliant.
“The majority say they’re confident but many of them are experiencing these fines and penalties,” says Saperstein. “On average, it’s about six times a year and the average cost of one of these penalties or fines is $90,000.”
Nearly two-thirds of benefits decision-makers at midsized companies are not confident they understand the ACA and what they need to do to be compliant. Ninety percent aren’t confident their employees understand the effects of the ACA on their benefits choices.
U.S. Obesity Rate Climbing in 2013
Originally posted November 1, 2013 by Lindsey Sharpe on https://www.gallup.com
WASHINGTON, D.C. -- The adult obesity rate so far in 2013 is 27.2%, up from 26.2% in 2012, and is on pace to surpass all annual average obesity rates since Gallup-Healthways began tracking in 2008.
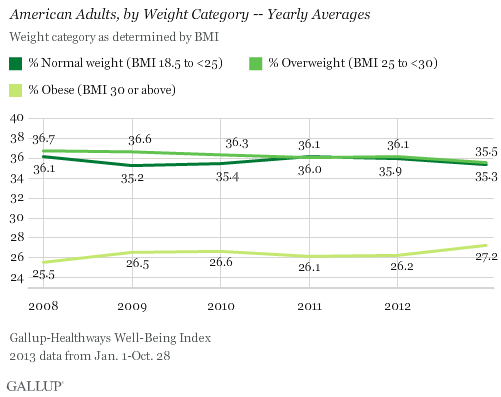
The one-percentage-point uptick in the obesity rate so far in 2013 is statistically significant and is the largest year-over-year increase since 2009. The higher rate thus far in 2013 reverses the lower levels recorded in 2011 and 2012, and is much higher than the 25.5% who were obese in 2008.
The increase in obesity rate is accompanied by a slight decline in the percentage of Americans classified as normal weight or as overweight but not obese. The percentage of normal weight adults fell to 35.3% from 35.9% in 2012, while the percentage of adults who are overweight declined to 35.5% from 36.1% in 2012. An additional 1.9% of Americans are classified as underweight in 2013 so far.
Since 2011, U.S. adults have been about as likely to be classified as overweight as normal weight. Prior to that, Americans were most commonly classified as overweight.
Gallup and Healthways began tracking Americans' weight in 2008. The 2013 data are based on more than 141,000 interviews conducted from Jan. 1 through Oct. 28 as part of the Gallup-Healthways Well-Being Index. Gallup uses respondents' self-reported height and weight to calculate body mass index (BMI) scores. Individual BMI values of 30 or above are classified as "obese," 25 to 29.9 are "overweight," 18.5 to 24.9 are "normal weight," and 18.4 or less are "underweight."
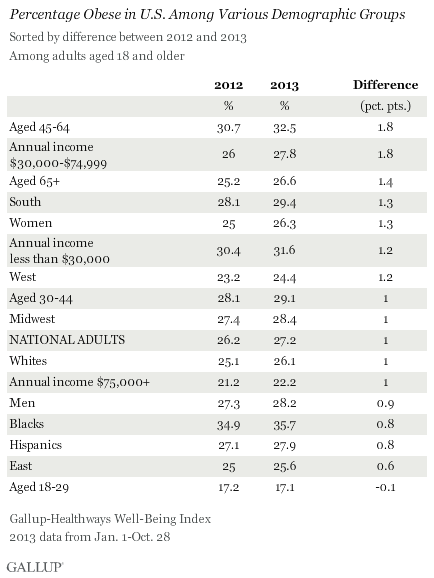
Obesity Rates Increase Across Almost All Demographic Groups
Obesity rates have increased at least slightly so far in 2013 across almost all major demographic and socioeconomic groups. One exception is 18- to 29-year-olds, among whom the percentage who are obese has remained stable. The largest upticks between 2012 and 2013 were among those aged 45 to 64 and those who earn between $30,000 and $74,999 annually. The obesity rate within both groups increased by 1.8 points, which exceeds the one-point increase in the national average.
At 35.7%, blacks continue to be the demographic group most likely to be obese, while those aged 18 to 29 and those who earn over $75,000 annually continue to be the least likely to be obese.
Bottom Line
The U.S. obesity rate thus far in 2013 is trending upward and will likely surpass all annual obesity levels since 2008, when Gallup and Healthways began tracking. It is unclear why the obesity rate is up this year, and the trend since 2008 shows a pattern of some fluctuation. This underscores the possibility that that the recent uptick is shorter-term, rather than a more permanent change. Still, if the current trend continues for the next several years, the implications for the health of Americans and the increased burden on the healthcare system could be significant.
Blacks, those who are middle-aged, and lower-income adults continue to be the groups with the highest obesity rates. The healthcare law could help reduce obesity among low-income Americans if the uninsuredsign up for coverage and take advantage of the free obesity screening and counseling that most insurance companies are required to provide under the law.
Employers can also take an active role to help lower obesity rates. Gallup has found that the annual cost for lost productivity due to workers being above normal weight or having a history of chronic conditions ranges from $160 million among agricultural workers to $24.2 billion among professionals. Thus, employers can cut healthcare costs by developing and implementing strategies to help workers maintain or reach a healthy weight.
Gallup has also found that employees who are engaged in their work eat healthier and exercise more. Therefore, employers who actively focus on improving engagement may see healthier and more productive workers, in addition to lower healthcare costs.
About the Gallup-Healthways Well-Being Index
The Gallup-Healthways Well-Being Index tracks well-being in the U.S. and provides best-in-class solutions for a healthier world. To learn more, please visit well-beingindex.com.
Results are based on telephone interviews conducted as part of the Gallup-Healthways Well-Being Index survey Jan. 1-Oct. 28, 2013, with a random sample of 141,935 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
For results based on the total sample of national adults, one can say with 95% confidence that the margin of sampling error is ±0.5 percentage points.
Interviews are conducted with respondents on landline telephones and cellular phones, with interviews conducted in Spanish for respondents who are primarily Spanish-speaking. Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by region. Landline and cellphone numbers are selected using random-digit-dial methods. Landline respondents are chosen at random within each household on the basis of which member had the most recent birthday.
Samples are weighted to correct for unequal selection probability, nonresponse, and double coverage of landline and cell users in the two sampling frames. They are also weighted to match the national demographics of gender, age, race, Hispanic ethnicity, education, region, population density, and phone status (cellphone only/landline only/both, and cellphone mostly). Demographic weighting targets are based on the March 2012 Current Population Survey figures for the aged 18 and older U.S. population. Phone status targets are based on the July-December 2011 National Health Interview Survey. Population density targets are based on the 2010 census. All reported margins of sampling error include the computed design effects for weighting.
In addition to sampling error, question wording and practical difficulties in conducting surveys can introduce error or bias into the findings of public opinion polls.
For more details on Gallup's polling methodology, visit www.gallup.com.
FSA use-it-or-lose-it rule changed!
Originally posted October 31, 2013 by Kathryn Mayer on https://www.benefitspro.com
Use-it-or-lose-it is no more.
The U.S. Department of the Treasury and the IRS on Thursday issued a notice modifying the longstanding “use-or-lose” rule for health flexible spending arrangements. Participants now can carry over up to $500 of their unused balances remaining at the end of a plan year.
The rule will go into effect for the 2014 plan year.
Effective immediately, employers that offer FSAs that don't include a grace period will have the option of allowing employees to roll over up to $500 of unused funds at the end of this plan year.
An employer cannot offer a FSA carryover provision and an FSA grace period at the same time, officials said.
For nearly 30 years, employees eligible for FSAs have been subject to the use-it-or-lose-it rule, meaning any account balances remaining unused at the end of the year are forfeited.
FSAs allow employees to contribute pre-tax dollars to pay for out-of-pocket health care expenses – including deductibles, copayments, and other qualified medical, dental or vision expenses not covered by the individual’s health insurance plan.
Health savings accounts, on the other hand, are similar vehicles, but allow participants to build up savings over time.
The move, the departments announced, is making “FSAs more consumer-friendly and provide added flexibility.”
“Across the administration, we’re always looking for ways to provide added flexibility and commonsense solutions to how people pay for their health care,” Treasury Secretary Jacob Lew said in a statement. “Today’s announcement is a step forward for hardworking Americans who wisely plan for health care expenses for the coming year.”
The change responds directly to more than 1,000 public comments the Treasury fielded. Employers and employees complained about the difficulty for employees to predict future needs for medical expenditures. Many FSA users said they scrambled at year end to spend the remaining amounts, often buying unnecessary medical supplies.
IRS officials said they believe a $500 rollover cap is appropriate because most employees who lost money under the rule lost far less than that amount.
Bob Natt, executive chairman of Alegeus Technologies, a health and benefits payments firm, said he’s grateful the administration has “eliminated the most significant barrier to FSA participation – namely consumers’ fear of losing their money.”
He said that though more than 85 percent of large employers offer FSAs, only about 20 percent of eligible employees actually enroll, mainly for “fear of forfeiting unused funds at the end of the plan year.”
“With this new provision in effect, there is really no reason for eligible employees not to enroll and contribute to an FSA," Natt said. "All contributions are tax-free, the employee’s full election is available on the first day of the plan year, and now unused funds up to $500 can be rolled over to the next plan year.”
Alegeus Technologies has been lobbying for four years to modify the use-it-or-lose-it provision, he said.
Wageworks, a benefits management provider of consumer-directed benefits, has also been pushing the administration for flexibility on FSA provisions. The company's CEO, Joe Jackson, said it's a very "positive change" and a long time coming.
"The timing of this change could not be better, as most companies are now in their open enrollment period," Jackson said. "We encourage all eligible employees to take advantage of this change and sign up for an FSA and lower their health care expenses.”
The rule will have far-reaching effects: An estimated 14 million families participate in FSAs.
Under the Patient Protection and Affordable Care Act, the amount an employee can set aside in an FSA dropped to $2,500 this year. The $500 carryover won’t reduce the $2,500 maximum a worker can contribute to a FSA each year, Treasury officials said.
5 myths about millennials and benefits
Originally posted by Lindsey Pollak on https://www.benefitspro.com
Millennials (ages 18-31), also known as Gen Y, are 80 million strong, according to the U.S. Census Bureau. As this generation climbs into leadership roles, they’ll change many aspects of the workplace, including the benefits landscape.
To help better understand this giant generation of consumers and employees, it’s time to dispel five common myths about who millennials are and what they want.
1.) Millennials all live at home and don’t have financial responsibilities.
True, many millennials are living at home today. Three out of 10 parents (27 percent) have at least one adult child, between the ages of 21 and 40, still living with them at home, according to the National Housing Federation. But that doesn’t mean they don’t have financial responsibilities: Mom and Dad might be asking Junior to chip in on rent or expecting him to pay off his student loans they co-signed.
The Hartford 2013 Benefits for Tomorrow Study found two-thirds of workers today have loved ones relying on their paycheck, with 10 percent of millennials reporting that their parents rely on their salary. That’s all the more reason for millennials to protect their paycheck by signing for disability insurance at work.
For many millennials living at home, one of their primary financial responsibilities is dealing with student loan debt. The average debt for students graduating in 2013 is $35,000, according to Fidelity. If parents are co-signers on those student loans, it’s in their best interest to encourage their kids to sign up for disability and life insurance at work. Disability insurance can help keep an income coming in (and the ability to pay back loans) should the millennial worker become ill or injured off the job, while life insurance can help provide funding to pay off student loan debt.
Help the millennials make the connection between benefits and their very real financial responsibilities.
2.) Millennials want all digital communications all the time.
True, millennials are considered “digital natives.” They’ve grown up with technology their entire lives. While they like digital options, many appreciate help in real life, as well. They appreciate an advisor who can provide advice in whatever way they desire — text, email, instant message, phone call, or an in-person meeting.
Help millennials by providing the benefits advisors that they’re looking for. They want to be able to review their benefits options online but have a real-live person available to answer their specific questions. Help your clients make this connection possible.
3.) Millennials all want to start their own companies like Mark Zuckerberg.
True, many millennials think like entrepreneurs. Many even have side projects, like a blog, in addition to their 9-to-5 jobs. But the vast majority of millennials like to work for companies of all sizes — as long as those companies understand them and their needs.
Help the millennials on your team feel like entrepreneurs, by allowing them to express their individuality and effect change around them. And share this advice with your employer clients, as well.
For example, some companies allow millennials to pursue small projects related to their particular interests or participate in occasional community service projects during work hours.
4.) Millennials don’t want baby boomers’ help or advice.
True, millennials enjoy their independence. But in the workplace they actually appreciate theirbaby boomer co-workers’ experience and knowledge. Don’t forget that the millennials are the children of baby boomers, and many raised their kids in their own image. Millennials tend to like and appreciate their baby boomer bosses and colleagues.
The Hartford 2013 Benefits For Tomorrow Study found that 93 percent of baby boomers believe millennials bring new skills and ideas to the workplace, and 89 percent of millennials agree baby boomers in the workplace are a great source of mentorship.
Help millennials by making connections between the two generations — either at your workplace or among your employer clients. Consider the idea of co-mentoring, in which employees of different generations share knowledge and skills with each other.
When you are having discussions around company policies and decisions, make sure to have representative employees present from all generations in your company. This way there will be someone who can offer each generation’s point of view on the items under discussion.
5.) Millennials aren’t serious about being leaders.
True, millennials are often viewed as “entitled” and carefree. Case in point: the YOLO (you only live once) catchphrase. But many are leaders in all aspects of life. In fact, 15 percent of millennials are already in management positions, and there are many young people who want to move into leadership positions soon.
Help millennial leaders to understand that they need to protect their potential. Show them how insurance benefits can keep them on track to meet their professional and personal goals. For example, if they can’t work because they tore a ligament during a 5K, disability insurancemay help them pay bills — and stay on track to buying a house or traveling around the world.
By helping millennials as both consumers and employees, you can better advise your clients and manage your business today — and into the increasingly millennial-dominated future.
Stories that Will Make HR Scream
Originally posted by Denise Rand on hrdailyadvisor.blr.com
Happy Halloween!!! HR Daily Advisor decided to put together a list of some of the scariest HR Strange but True! stories from this year, guaranteed to frighten any HR pro.
- 10 Most Outrageous Things Applicants Have Done that Did and Didn’t Work—Candidates want to stand out from the crowd and be memorable. However, sometimes their outside-the-box methods just bomb.
- Trick or Treat: Employee Hands Out Pot Brownies to Employees—A former San Diego bus driver joined the ranks of going too far with a prank by handing out pot brownies at work.
- Does that Tweet Scream ‘Fire Me’?—If you’re a Twitter user, you’ve probably seen a few Tweets from disgruntled workers. The problem—Twitter is a public social media site, a fact that this app exploits.
- Strange Sightings at Company Parties—As part of a survey, respondents were asked to recount the wackiest or most outrageous thing they have heard of an employee doing at a company event.
- The Man and the Mooning—After a Chicago investment analyst learned of a colleague’s termination, he took matters into his own hands. He went into an executive meeting and expressed his anger by mooning the group.
- Dirty Rats and Crazy Ants: Here’s Your Workplace Vermin Update—Here’s an animal-related SBT that’s not about dogs, goats, or monkeys (our usual favorites), but about what OSHA calls “vermin.”
And last, but certainly not least, here are a few frightening tales from our readers:
- Toilet Talk or Dirty Seat? Clean It Up—This reader shared a story about how HR had to clean up a messy issue.
- The Creepy Coworker—One SBT reader wrote in about an employee who had his own weird way to personalize his workspace.
- Keep Your Clippings to Yourself—Personal hygiene can be an issue in the workplace. While you may immediately think of body odor as the main culprit, this SBT reader shows that there are other grooming issues that HR may have to address.
Do you have an odd workplace story? Share your story in the comments below!!! Thanks!
Self-insured win partial PPACA fee exemption
Originally posted October 28, 2013 by Dan Cook on www.lifehealthpro.com
Self-insured employers and self-administered health plans are about to catch a break, thanks to fine-tuning of the Patient Protection and Affordable Care Act by the Department of Health and Human Services.
In a soon-to-be-published compendium of rule modifications, HHS says it will exempt certain self-insured employers from the second two years of paying the reinsurance fee.
HHS says the proposed modifications — of which there are quite a few — are the result of its “listening” sessions with interested parties about specific requirements of the act. The full list can be found in the proposal, “Program Integrity: Exchange, Premium Stabilization Programs, and Market Standards; Amendments to the HHS Notice of Benefit and Payment Parameters for 2014.”
HHS doesn’t offer a whole of detail on the exemption matter. It says in order to address employer feedback that the fees are burdensome, it will accept payment of the fee in two chunks instead of one (at the beginning of 2014 and at the end of the year) and will “exempt certain self-insured, self-administered plans from the requirement to make reinsurance contributions for the 2015 and 2016 benefit years” in future rulemaking and/or guidance proposals.
However, all employers will be required to pay the first-year fee for the program, which begins in 2014.
The 2014 fee for the three-year Transitional Reinsurance Program was set at $63 per plan participant. Fee levels have not been set for 2015 and 2016.
The fees are designed to yield $25 billion over the three-year program – money that would help offset costs incurred by insurers covering high-cost individuals purchasing coverage in public insurance exchanges.
HHS’s missive addressed other matters, including what happens when a small company buys small group insurance, and then it becomes a large company. The employer can keep the small group insurance package as long as it doesn’t make substantial modifications to it. But if discontinues small group coverage, it will then have to purchase insurance through the large group exchanges.
HHS also promised to provide further guidance on the sticky issue of what constitutes a fulltime employee for purposes of the all-important employee head count.
The proposals are scheduled to be published in the Federal Register on Wednesday.
The Evil Presence that Lurks in the Workplace at Halloween
Originally posted by Denise Rand on https://hrdailyadvisor.blr.com
Halloween can be a very scary time of the year for HR pros! An evil presence is out to kill the efforts being put into company wellness programs—Halloween candy. Yes, it seems like Halloween becomes the end of year "kickoff party" for calorie-, sugar-, and fat-filled holiday celebrations in workplaces, sabotaging companies’ health efforts.
And besides candy, it’s a safe bet there will be plenty of orange-colored cakes, cupcakes, donuts, and even orange bagels within easy reach. However, there are some proactive steps the HR department can take to keep your employees from falling victim to a sugar rush and extra holiday pounds.
Health experts Dian Griesel, PhD, and Tom Griesel, authors of the book The TurboCharged Mind (January 2012, BSH), offer the following tips to avoid a crash:
- Make an office resolution to keep out of the office all the extra candy that the kids brought home or that didn’t go to the trick-or-treaters.
- Start the day by brewing a pot of pumpkin-flavored coffee or tea. This should help get coworkers in the spirit of things.
- Bring in a variety of fruit for morning break and colored veggies for enjoyment at lunch or afternoon break.
- Take a lunchtime walk to see the change of foliage and get some fresh autumn air.
- If your “office bakers” must produce Halloween treats, have them try making a gluten-free, low-, or sugar-free pumpkin pie. There are even many recipes for crust-less, no-shortening versions that make things even more healthful—and easy.
What really scares us these days
Originally posted October 24, 2013 by Corey Dahl on https://www.lifehealthpro.com
When I was in sixth grade, I went to my first commercial (as in, non-neighbor’s-darkened-basement-strewn-in-cotton-cobwebs-and-paper-bats) haunted house.
It was the ‘90s, the heyday of those cheap, ill-produced FrightFezts and ScReAm ZoNes that sprouted in derelict shopping centers every fall, and you weren’t cool — by middle school standards, anyway — if you didn’t go to at least one. So my friends and I skipped trick-or-treating that year, stood in an hour-long line and paid $10 of our parents’ money to see what all the hype was about.
When we emerged about 15 minutes later, I wished I’d gone trick-or-treating instead. My friends were pumped — screaming and giggling — and, wanting to fit in, I played along. But really, the entire thing had bored me. I mean, toy chain saws? Fog machines? Cheap makeup? Yawn.
Maybe I was just a really jaded 11 year old, or maybe it was just a really crappy haunted house — this was before they became the multi-story productions they are today, after all — but there was nothing in that Hobby Lobby-cum-House of Horrors that scared me in the slightest.
And, while I haven't been to a haunted house since, I don’t think it would be much different for me these days, either. I spend the entirety of slasher movies critiquing plot holes and poor acting. I’m not really into the whole zombie trend. When the electricity goes out, I worry about my frozen foods melting, not a potential ghost attack.
Increasingly, it seems I’m not alone. I read an article last week about the scaring difficulties haunted houses have been facing lately. Despite spending thousands on machines, effects, masks and professional actors, the houses’ operators are watching a lot of their guests walk away unperturbed.
The haunted house operators blamed technology. Better movie and video game special effects have upped the ante considerably, they said. And yeah, okay. Maybe. But as a longtime non-scared, I think the better culprit might be real life.
Because, the more I look back on it, the more I’m convinced that my blasé attitude toward that strip-mall haunted house (and all cheap frights) was entirely due to the fact that I’d seen a lot of things scarier than pimply, dressed-up teenagers jumping out from behind cardboard trees.
By the time I was 11, one of my grandmas had died. The other was in failing health, requiring my mom to juggle nursing home bills and the care of a senior and three daughters.
Our house had been robbed a few years earlier, and they’d run off with my life savings ... which was $20 in an old Folgers coffee can.
And I’d traveled extensively with my somewhat directionally challenged family, which meant we often got lost in the bad neighborhoods of big cities. A homeless man, dressed in nothing but a garbage bag and asking for spare change, had chased me down a street in New York just a few months earlier.
So my lack of fear didn’t come from extraordinary bravery of some kind — I was scared of miller moths until I was well into college — but probably from simply knowing that rubber masks and strobe lights couldn’t hold a candle to most of the things real life had in store.
Following one of our country’s worst economic downturns and given the employment, retirement andlong-term care struggles most Americans continue to face — to say nothing of the real-life tragedies we’ve experienced, from hurricanes, tsunamis, mass shootings and the like — I suspect a lot of other people have started to realize the same. We’re living at a time when you’ll get more screams from people with a bank statement than a bludgeon.
Part of that makes me glad; it’s a sign that we’re finally facing facts, I think. But it’s also incredibly sad, this idea that our reality has outpaced the worst horrors we could previously imagine.
But it doesn’t have to be like this. If my theory’s even slightly correct, I think it also proves the dramatic need for the advice of insurance agents and financial advisors these days. With a suitable plan in place, a lot of people could avoid the real-life horrors of unpaid bills and underfunded retirements.
And the faster producers can ease clients’ worst fears, the sooner they can get back to freaking out over corn-syrup blood. Or, if they’re like me, making fun of it.
Happy Halloween!
