The do’s and don’ts of ADA accommodations: 3 new rulings
More than 25,000 ADA charges were filed by the EEOC in the past year, despite employers best compliance efforts. Continue reading this blog post to learn more.
Employers are facing more disability discrimination lawsuits than ever – despite their best compliance efforts.
In the past year alone, over 25,000 ADA charges were filed by the EEOC.
The right way to accommodate
One area that’s often a point of contention? The accommodation process. Workers and employers can have a very different idea of how a disability should be accommodated.
And while each disability needs to be evaluated on a case by case basis, several recent court rulings shed further light on employers’ ADA accommodation responsibilities.
1. In Brumley v. United Parcel Service, a court ruled that ADA accommodations don’t necessarily have to be given to employees immediately.
Melissa Brumley delivered packages for UPS when she hurt her back lifting a heavy box from her truck.
She took leave to heal, and her doctor said when she returned to work she could no longer lift packages or drive. Since these were two essential functions of her job, Brumley’s manager put her on leave while waiting on more information from her doctor.
After beginning the interactive process and considering a reassignment, Brumley’s doctor cleared her to go back to her old job, and UPS ended the process.
But Brumley sued the company for failing to accommodate her during those weeks she was on leave, which resulted in loss of pay.
A district court ruled in favor of UPS, and on appeal, the 6th Circuit agreed. It said just because the company didn’t accommodate the employee immediately didn’t mean it violated the ADA.
UPS began the interactive process and only stopped once Brumley was cleared to go back to her old job without an accommodation.
The key things the company did? Beginning the process and requesting additional info from Brumley’s doctor – this showed the court a good faith effort to comply with the ADA.
2. In Sharbono v. Northern States Power, a court ruled a company that failed to find an accommodation didn’t fail to fulfill its ADA duties.
After a foot injury, James Sharbono wasn’t able to wear the steel-toed boots required by his company’s safety procedures.
HR worked with Sharbono and suggested several accommodations, such as altering his boots and getting a custom pair made, but none worked out. Sharbono was forced to retire, and he sued for ADA violation.
But the 8th Circuit ruled the company acted in good faith. It worked with Sharbono and suggested several accommodations. It was only after exhausting all options that Sharbono was forced to retire. The court said the company fulfilled its ADA responsibilities, despite finding no accommodation for Sharbono.
3. In Stokes v. Nielsen, a court decided companies can be required to make accommodations that cover more than just essential job functions.
Jacqueline Stokes had impaired vision and received multiple accommodations that allowed her to do her job. Stokes then requested special meeting handouts, printed in large letters, that she could read beforehand.
Despite many promises from HR, Stokes never received her requested handouts. She sued, claiming to be denied a reasonable accommodation under the ADA.
While the company argued it gave Stokes everything she needed to do her job, therefore fulfilling its ADA responsibilities, the Fifth Circuit disagreed.
“Our circuit has explicitly rejected the requirement that requested modifications must be necessary to perform essential job functions to constitute a reasonable accommodation,” it said. And Stokes’ request was deemed reasonable.
This case shows if an employee makes a reasonable request for their job, it’s easier to just grant it.
SOURCE: Mucha, R. (4 January 2019) "The do’s and don’ts of ADA accommodations: 3 new rulings" (Web Blog Post). Retrieved from https://www.hrmorning.com/the-dos-and-donts-of-ada-accommodations-3-new-rulings/
Association Health Plans Meet the 2018 Form M-1
The Employee Benefits Security Administration (EBSA) recently released the 2018 version of the Form M-1. Read this blog post for more information about the new Form M-1.
The Employee Benefits Security Administration (EBSA) is continuing to do what it can to help bring the new class of association health plans (AHPs) to life.
EBSA, an arm of the U.S. Department of Labor, unveiled the 2018 version of the Form M-1 Monday.
Administrators of multiple employer welfare arrangements (MEWAs) that provide medical benefits use Form M-1 to report on the MEWAs’ operations to the DOL.
The administration of President Donald Trump completed work on major new AHP regulations in June. The administration is hoping small employers will use the new AHPs to shield themselves from some state and federal mandates and to get a chance to benefit from being part of a large coverage buyer.
Any AHPs out there, including any AHPs formed under the new regulations, will need to file the 2018 Form M-1 with the Labor Department, EBSA said Monday.
An AHP, or other MEWA, can use Form M-1 both to register a new plan and to file the annual report for an in-force plan.
The 2018 annual report for an AHP or other MEWA in operation now will be due March 1, 2019.
If agents, brokers, benefit plan administrators or other financial professionals are trying to start AHPs, they are supposed to use Form M-1 to register the AHPs at least 30 days before engaging in any AHP activity.
“Such activities include, but are not limited to, marketing, soliciting, providing, or offering to provide medical care benefits to employers or employees who may participate in the AHP,” EBSA officials said in the form release announcement.
Resources
Links to AHP information, including information about the 2018 Form M-1, are available here.
SOURCE: Bell, A. (4 December 2018) "Association Health Plans Meet the 2018 Form M-1" (Web Blog Post). Retrieved from https://www.thinkadvisor.com/2018/12/04/association-health-plans-meet-the-2018-form-m-1/
From HSA to 401(k) contribution limits, 11 numbers to know for 2019
Do you offer HSAs, FSAs or 401(k)s to your employees? There are many important numbers companies and employees need to know regarding HSAs, FSAs and 401(k)s. Read this blog post to learn more.
There are a slew of important figures companies and employees need to know regarding health savings accounts, 401(k)s and flexible spending accounts. While the IRS announced HSA changes in May, the agency only recently announced annual changes to FSAs and 401(k)s. From contribution limits to out-of-pocket amounts, here are the figures employers need to know — all of which take effect in January.
$19,000: 401(k) pre-tax contribution limits
$6,000: 401(k) catch-up contribution limit
$6,000: IRA contribution limits
$3,500: Annual HSA contribution limit for individuals
$7,000: HSA contribution limit for family coverage
$1,350: HDHP minimum deductible for individual
$2,700: HDHP minimum deductible for family
$6,750: HDHP maximum out-of-pocket amounts (individual)
$13,500: HDHP maximum out-of-pocket amounts (family)
$1,000: HSA catch-up contributions
$2,700: FSA contribution limit
SOURCE: Mayer, K. (6 December 2018) "From HSA to 401(k) contribution limits, 11 numbers to know for 2019" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/from-hsa-to-401-k-contribution-limits-11-numbers-to-know-for-2019
2019: A Look Forward
A number of significant changes to group health plans have been made since the Affordable Care Act (ACA) was enacted in 2010. Many of these changes became effective in 2014 and 2015 but certain changes to a few ACA requirements take effect in 2019.
Changes for 2019
- Cost-sharing Limits – Non-grandfathered plans are subject to limitations on cost sharing for essential health benefits (EHB). The annual limits on cost sharing for EHB are $7,900 for self-only coverage and $15,800 for family coverage, effective January 1, 2019.
- Health plans with more than one service provider can divide maximums between EBH as long as the combined amount does not exceed the out-of-pocket maximum limit for the year.
- Beginning in 2016, each individual – regardless of the coverage the individual is enrolled – is subject to the self-only annual limit on cost sharing.
- The ACA’s annual cost-sharing limits are higher than high deductible health plans (HDHPs) out-of-pocket maximums. For plans to qualify as an HDHP, the plan must comply with HDHP’s lower out-of-pocket maximums. The HDHP out-of-pocket maximum for 2019 is $6,750 for self-only coverage and $13,500 for family coverage.
- Coverage Affordability Percentages – If an employee’s required contribution does not exceed 9.5 percent of their household income for the taxable year (adjusted each year), then the coverage is considered affordable. The adjusted percentage for 2019 is 9.86 percent.
- Reporting of Coverage – Returns for health plan coverage offered or provided in 2018 are due in early 2019. For 2018, returns must be filed by February 28, 2019, or April 1, 2019 (if electronically filed). Individual statements must be provided by January 31, 2019.
- ALEs are required to report information to the IRS and their eligible employees regarding their employer-sponsored health coverage. This requirement is found in Section 6056. Reporting entities will generally file Forms 1094-B and 1095-B under this section.
- Every health insurance issuer, self-insured health plan sponsor, government agency that provides government-sponsored health insurance, and any other entity that provides MEC is required to finalize an annual return with the IRS, reporting information for each individual who is enrolled. This requirement is found in Section 6055. Reporting entities will generally file Forms 1094-C and 1095-C under this section.
- ALEs that provide self-funded plans must comply with both reporting requirements. Reporting entities will file using a combined reporting method on Forms 1094-C and 1095-C.
- Forms Used for Reporting – Reporting entities must file the following with the IRS:
- A separate statement for each individual enrolled
- A transmittal form for all returns filed for a given calendar year.
- Electronic Reporting – Any reporting entity that is required to file 250 or more returns in either section must file electronically on the ACA Information Returns (AIR) Program. Reporting entities that file less than 250 returns can file in paper form or electronically on the ACA Information Returns (AIR) Program.
- Penalties – Entities that fail to comply with the reporting requirements are subject to general reporting penalties for failure to file correct information returns and failure to furnish correct payee statements. Penalty amounts for failure to comply with the reporting requirements in 2019 are listed below:
| Penalty Type | Per Violation | Annual Maximum | Annual Maximum for Employers with up to $5 million in Gross Receipts |
| General | $270 | $3,275,500 | $1,091,500 |
| Corrected within 30 days | $50 | $545,500 | $191,000 |
| Corrected after 30 days but before August 1 | $100 | $1,637,500 | $545,500 |
| Intentional Disregard | $540* | None | N/A |
**Intentional disregard penalties are equal to the greater of either the listed penalty amount or 10 percent of the aggregate amount of the items required to be reported correctly.
Expected Changes
- Health FSA Contributions – Effective January 1, 2018, health FSA salary contributions were limited to $2,650. The IRS usually announces limit adjustments at the end of each year. This limit does not apply to employer contributions or limit contributions under other employer-provided coverage.
- Employer Shared Responsibility Regulations – The dollar amount for calculating Employer Shared Responsibility 2 penalties is adjusted for each calendar year. Applicable large employers (ALEs) must offer affordable, minimum value (MV) healthcare coverage to full-time employees and dependent children or pay a penalty. If one or more full-time employees of an ALE receive a subsidy for purchasing healthcare coverage through an Exchange, the ALE is subject to penalties.
- Applicable Large Employer Status – ALEs are employers who employ 50 or more full-time employees on business days during the prior calendar year.
- Offering Coverage to Full-time Employees – ALEs must determine which employees are full-time. A full-time employee is defined as an employee who worked, on average, at least 30 hours per week or 130 hours in a calendar month. There are two methods for determining full-time employee status:
- Monthly Measurement Method – Full-time employees are identified based on a month-to-month analysis of the hours they worked.
- Look-Back Measurement Method – This method is based on whether employees are ongoing or new, and whether they work full time or variable, seasonal or part-time. This method involves three different periods:
- Measurement period – for county hours of service
- Administration period – for enrollment and disenrollment of eligible and ineligible employees
- Stability period – when coverage is provided based on an employee’s average hours worked.
- Applicable Penalties – ALEs are liable for penalties if one or more full-time employees receive subsidies for purchasing healthcare coverage through an Exchange. One of two penalties may apply depending on the circumstances:
- 4980H(a) penalty – Penalty for not offering coverage to all full-time employees and their dependents. This penalty does not apply if the ALE intends to cover all eligible employees. ALEs must offer at least 95 percent of their eligible employees’ health care coverage. Monthly penalties are determined by this equation:
- ALE’s number of full-time employees (minus 30) X 1/12 of $2,000 (as adjusted), for any applicable month
- The $2,000amount is adjusted for the calendar year after 2014:
- $2,080 – 2015; $2,160 – 2016; $2,260 – 2017; $2,320 – 2018
- 4980H(b) penalty – penalty for offering coverage – ALEs are subject to penalties even if they offer coverage to eligible employees if one or more full-time employees obtain subsidies through an Exchange because:
- The ALE didn’t offer all eligible employees coverage
- The coverage offered is unaffordable or does not provide minimum value.
- Monthly penalties are determined by this equation: 1/12 of $3,000 (as adjusted) for any applicable month
- $3,120 – 2015; $3,240 – 2016; $3,390 – 2017; $3,480 – 2018
- 4980H(a) penalty – Penalty for not offering coverage to all full-time employees and their dependents. This penalty does not apply if the ALE intends to cover all eligible employees. ALEs must offer at least 95 percent of their eligible employees’ health care coverage. Monthly penalties are determined by this equation:
Contact one of our advisors for assistance or if you have any questions about compliance in the New Year.
SOURCES: www.dol.gov, www. HHS.gov, https://www.federalregister.gov/documents/2018/04/17/2018-07355/patient-protectionand-affordable-care-act-hhs-notice-of-benefit-and-payment-parameters-for-2019, https://www.irs.gov/e-fileproviders/air/affordable-care-act-information-return-air-program
DOL reverses course on ‘80/20’ limitations for tipped employees
On November 8, the Department of Labor (DOL) released four new opinion letters, providing insight into their views on compliance with federal labor laws. Read this blog post to learn more.
Last week, the DOL issued four new opinion letters providing both employers and employees further insight into the agency’s views regarding compliance with federal labor laws.
While the letters touch on a variety of issues, perhaps the most notable change involves the DOL’s about-face regarding the amount of “non-tipped” work an employee can perform while still receiving a lower “tip-credit” wage.
Essentially, this new guidance does away with the previous “80/20” rule regarding tipped employees. Under the 80/20 rule, businesses were barred from paying employees traditionally engaged in tip-based work, like servers and bartenders, a lower minimum wage and taking a tip credit for the other portion of the employee’s wage up to applicable state and federal minimum wage requirements when those employees’ side work, like napkin folding or making coffee, accounted for more than 20% of the employee’s time.
In recent years, there has been an explosion of litigation across the country over the 80/20 rule, questioning whether the tipped employee’s “side work” amounted to more than 20% of the employee’s duties and time. Likewise, in many of those same suits, plaintiffs would challenge individual tasks associated with their side work, attempting to claim that those tasks were not so closely related to their tipped duties, but rather rose to the level of a completely different or “dual job,” meaning that the employer should not be permitted to take the tip credit for hours worked performing those tasks.
What followed was case after case of lawyers, courts and employers quibbling over minutes spent folding napkins, wiping counters, slicing lemons, and painstakingly calculating and arguing as to whether those tasks added up to 20% and whether those tasks were not closely related enough to be included in the 20% calculation.
In these kinds of cases, we’d see arguments over circumstances like the server that moonlights as a “maintenance man” versus the server that changed the lightbulb or helped sweep underneath the tables.
The ultimate result: confusion, chaos and, frankly, a treasure trove for plaintiff’s attorneys who had another arrow in their quiver in which to seek additional purported wages for clients from employers that would find it difficult, if not impossible, to account for all minutes and tasks employees were performing in busy restaurants.
Following the DOL’s opinion letter, the landscape will change. Recognizing that the existing guidance and case law had created “some confusion,” the DOL expressly stated that they “do not intend to place a limitation on the amount of duties related to a tip-producing occupation that may be performed, so long as they are performed contemporaneously with direct customer-service duties...”
However, in attempting to provide additional clarity, the DOL may have instead opened up the proverbial Pandora ’s Box of uncertainty. In identifying the list of duties that the DOL would consider “core or supplemental,” the DOL refers to the Tasks section of the Details report in the Occupational Information Network (O*NET). It goes without saying that no document can provide an exhaustive list of tasks in today’s changing marketplace. While the DOL attempted to recognize the changing nature of today’s environment in a savings-type footnote, one does not have to look too far ahead to foreshadow the response from the plaintiff’s bar arguing over the related duties listed on O*NET.
While the DOL’s new position on the 80/20 rule will certainly come as a relief to many employers with tipped employees, employers should still be mindful in evaluating tipped employees’ job duties on a regular basis. Employees that are engaged in “dual jobs” are entitled to the full minimum wage, without the tip credit.
SOURCE: Kennedy, C. (15 November 2018) "DOL reverses course on ‘80/20’ limitations for tipped employees" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/dol-reverses-course-on-80-20-limitations-for-tipped-employees?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001
This article originally appeared on the Foley & Lardner website. The information in this legal alert is for educational purposes only and should not be taken as specific legal advice.
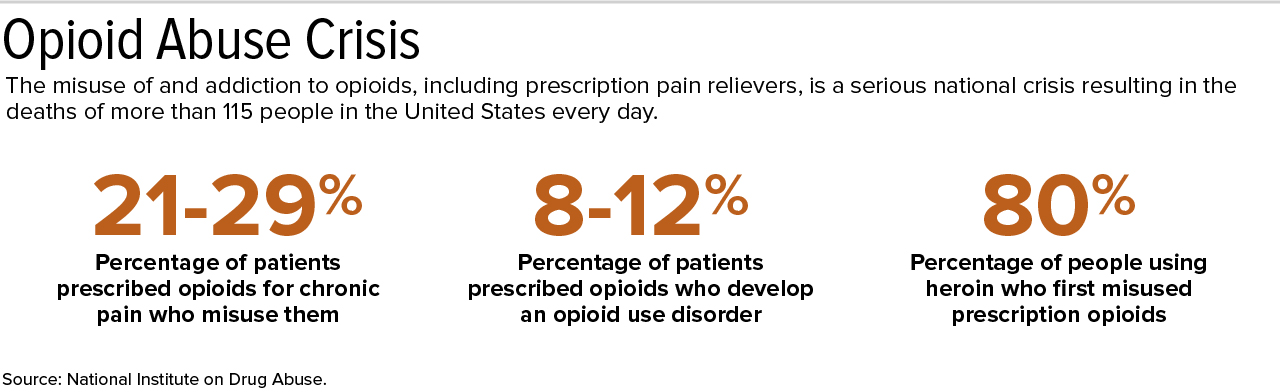
Interact Sensitively with Employees Addicted to Opioids
Opioid addiction is running rampant across the U.S. According to the National Institute of Drug Abuse, 8-12 percent of patients prescribed opioids develop an opioid use disorder. Read this blog post to learn more.
Employees who abuse opioids often are given a second chance by their employers. But well-meaning employers could wind up being sued for discriminating against those workers in violation of the Americans with Disabilities Act (ADA) if they don't handle the situation very carefully.
Opioid addiction has been rampant in the U.S. for some time. More than three out of five drug overdose deaths last year involved an opioid, and overdoses rose 70 percent in the 12 months ending September 2017, according to the Centers for Disease Control and Prevention.
So what can HR professionals do about it? If a worker admits to the problem, the path is fairly clear. But if the employer merely suspects that an employee is addicted to prescription pain relievers but has no real proof, the employee should be treated like any other employee who is having attendance or performance issues, said Kathryn Russo, an attorney with Jackson Lewis in Melville, N.Y.
An employer should never accuse someone of having an addiction, because if the employer is wrong, the accusation could lead to an ADA claim, Russo cautioned. Although current drug use isn't considered an ADA disability, a history of drug addiction is. Moreover, someone using prescription drugs might have an underlying condition covered by the ADA.
If an employee admits to opioid abuse, or the problem is discovered through drug testing, the employer should discuss it with the employee to determine if he or she needs a reasonable accommodation, such as leave to obtain treatment, Russo said. The illegal use of drugs need not be tolerated at work, she added.
Reasonably accommodate the employee so long as there's no direct threat to the health and safety of himself or herself, or others, recommended Nancy Delogu, an attorney with Littler in Washington, D.C.
Drug Testing
The Equal Employment Opportunity Commission has opined that employers may ask about an employee's use of prescribed medicine or conduct a drug test to determine such use only if the employer has reasonable suspicion that its use will interfere with the employee's ability to perform the job's essential functions or will pose a direct threat.
Many employers are expanding their drug-testing panels to include semisynthetic opioids such as hydrocodone, hydromorphone, oxycodone and oxymorphone, in addition to traditional opioids such as heroin, codeine and morphine, Russo said. This is lawful in most states as long as the employer does not take adverse employment actions when drugs are used legally, she noted, which is why an employer should use a medical review officer in the drug-testing process. If the medical review officer concludes that the positive test result is the result of lawful drug use, the result is reported to the employer as negative.
Sometimes an employer will say it has reasonable suspicion that the employee came to work impaired by drug use and is considering a mandatory drug test. At that point, some employees will say the drug test would be positive and the test consequently is not necessary.
Discussions with Employees
If there are performance problems and the employee has admitted to opioid addiction, some employers tell employees that they can remain employed so long as they go through inpatient treatment. Delogu discourages that approach. Employers aren't workers' doctors, so they shouldn't be deciding whether someone needs a treatment program, she explained.
But if someone voluntarily seeks to enter an addiction-recovery program, that person may have legal protections under state law, said Wendy Lane, an attorney with Greenberg Glusker in Los Angeles. For example, California has a law requiring employers with 25 or more employees to reasonably accommodate alcohol and drug rehabilitation.
Delogu recommended that employers that believe there is a problem with substance abuse ask if the addicted employee needs assistance from the employee assistance program.
An employer can require that an employee who has violated a policy be evaluated by a substance abuse professional and complete treatment prescribed for them, without dictating what that treatment will be, she said. The employer may choose to forgo disciplinary action if an employee agrees to these terms and signs an agreement to this effect. The employer then would not have to be informed about the person's decided course of treatment, whether inpatient, outpatient or no treatment at all, she said. The employee typically will be subjected to follow-up drug testing to make sure he or she hasn't resumed the use of illegal drugs.
Many employers are willing to give employees with performance problems resulting from opioid addiction a second chance, she noted.
SOURCE: Smith, A. (1 November 2018) "Interact Sensitively with Employees Addicted to Opioids" (Web Blog Post). Retrieved from https://www.shrm.org/ResourcesAndTools/legal-and-compliance/employment-law/Pages/employees-addicted-to-opioids.aspx
How to Handle Employee Requests for Time Off to Vote
Do you know how to handle employee requests for time off to vote? In some states, it is a requirement to give employees time off to vote. Read this blog post to learn more.
Many employees will be eligible to cast their ballot on Nov. 6, but will they have time to vote? Some states require employers to give workers time off to vote, and even in states that don't, some businesses are finding other ways to get employees to the polls.
With Election Day around the corner, employers should be mindful that, while no federal law provides employees leave to vote, many states have enacted laws in this area, said Marilyn Clark, an attorney with Dorsey & Whitney in Minneapolis. Depending on the state, employers may have to give workers notice about their voting rights and provide paid or unpaid time off to vote.
Even in states where there is no voting leave law, it is good practice to let employees take up to two hours of paid time off to vote if there isn't enough time for the employee to vote outside of working hours. "Encouraging and not discouraging employees should be the general rule," said Robert Nobile, an attorney with Seyfarth Shaw in New York City.
Encourage Employees
"Here in the United States, too many people don't vote because they don't have time due to jobs, child care and other responsibilities," said Donna Norton, executive vice president of MomsRising, an organization of more than 1 million mothers and their families. "Getting to the polls can be especially challenging for people in rural communities [or] single-parent households, and those who are juggling multiple jobs."
About 4 in 10 eligible voters did not vote in the 2016 presidential election, according to research conducted by Nonprofit VOTE and the U.S. Elections Project. And voter turnout has been historically lower for midterm elections, such as this year's, which are held near the midpoint of a president's four-year term, according to Pew Research Center.
"Businesses can help solve this problem by making sure that all employees have paid time off to vote," Norton said.
Some employers are offering solutions by making Election Day a corporate holiday, offering a few hours of paid time off for employees to vote and giving employees information about early and absentee voting, according to TheWashington Post.
Giving employees time off to participate in civic or community activities tends to improve worker performance, said Katina Sawyer, Ph.D., an assistant professor of management at George Washington University. Employers who are offering paid time off to vote will likely reap the benefits through improved employee attitudes and performance.
Know the Law
Employers in states with voting-leave laws should be familiar with the specific requirements, as some state laws have a lot of details. Even in states without such laws on the books, employers should check to see if there are any local voting leave ordinances in their cities.
Employers required to give workers time off to vote should plan for adequate work coverage to ensure that all employees can take time off, Clark said.
In many states, the employer may ask workers to give advance notice if they need time off and may require that workers take that leave at a specific time of the workday. In some states where leave is paid, employers might have the right to ask employees to prove they actually voted. Most states prohibit employers from disciplining or firing an employee who takes time off from work to vote.
"Ultimately, fostering an environment that generally encourages employees to exercise this important right is a good practice to mitigate the risk of a potential retaliation claim," Clark said.
Although state laws vary, "the general theme across the U.S. with respect to voting laws is that employees will be given time off to vote if there is insufficient time between the time the polls open and close within the state and the time employees start and finish work," Nobile said. "Typically, two to three consecutive nonworking hours between the opening and closing of the polls is deemed sufficient."
Some state laws provide unpaid leave to vote or do not address whether the leave must be paid. Oregon and Washington no longer have voting leave laws because they are "vote-by-mail" states.

In some states, such as California and New York, employers must post notices in the workplace before Election Day to inform employees of their rights. Employers might have to pay penalties if they don't comply.
The consequences for denying employees their voting rights can be harsh, with some states even imposing criminal penalties, Clark noted.
Create a Policy
At a minimum, employers should adopt a policy spelling out the voting rights available to employees under applicable laws, Clark said. For businesses that operate in states that don't have a voting-leave law, employers may still wish to adopt a policy outlining their expectations about time off for voting.
Multistate employers may elect to adopt a single policy that includes the most employee-friendly provisions of the state and local laws that cover them. "By taking this approach, employers avoid the administrative burden of adopting and promulgating multiple policies for employees working in different locales," Clark said. All voting-leave policies should be sure to include strong anti-retaliation provisions, which make clear that the employer will not take any adverse action against employees for exercising their voting rights.
"It's important to remember that the law sets the floor," said Bryan Stillwagon, an attorney with Sherman & Howard in Atlanta. "Companies with the happiest and most-engaged employees recognize that positive morale comes from doing more than what is required."
Nagele-Piazza, L. (29 October 2018) "How to Handle Employee Request for Time Off to Vote" (Web Blog Post). Retrieved from https://www.shrm.org/ResourcesAndTools/legal-and-compliance/state-and-local-updates/Pages/How-to-Handle-Employee-Requests-for-Time-Off-to-Vote.aspx
Dana Wilkie contributed to this article.
4 best practices for implementing a gamification-based compliance training system
Many employees may dislike and even disengage when their employer mentions implementing training sessions. Continue reading to learn how implementing a gamification-based training system can help improve employee engagement.
For most employees, compliance training is the Brussels sprouts on the kid’s plate of working life. Everyone knows it’s good for you — one mistake could lead to violations, accidents, reputation issues and maybe a not-so-friendly visit from regulatory body officials — but most workers turn up their noses and disengage when it’s time to dig in.
Considering that merely a third of American workers report feeling engaged at work as it stands, anything that makes matters worse is dangerous. Why risk inflaming indifference — not to mention spending money for on-site instructors — with dull-as-dry-toast workshops?
A far better bet is to embrace technology and go virtual. Of course, online-based compliance training won’t guarantee heightened participation or enthusiasm unless they have one specific aspect: gamification.
Gaming elements can turn any virtual compliance training learning management system (LMS) into an immersive experience. ELearning compliance training participants can enjoy customization and flexibility while getting up to speed on the latest rules, guidelines and protocols. With LMS gamification, HR managers and chief learning officers can cultivate and retain top talent. Best of all, it’s far easier to get buy-in for a robust LMS system with badges, bells and whistles than it is to make a pile of Brussels sprouts disappear from a toddler’s tray.
What exactly is so exciting about game-based learning? In essence, the process prompts active and immediate participation because of extra motivation in the form of rewards. Whether it’s badges or points, these features make eLearning interesting and enjoyable.
In one study, workers who enjoyed themselves retained concepts 40% better than those who weren’t having fun. As you might guess, this is what game-based learning is all about. Engaged employees who rapidly earn rewards are less likely to make errors, so they naturally increase a company’s bottom line and lower the likelihood of compliance fees and penalties. Plus, according to research from TalentLMS, 87% of employees report that gamification makes them more productive.
Merging gamification with training makes plenty of sense. It’s also easy to build a gamification-based compliance training LMS by following a straightforward LMS implementation checklist.
1. Identify your training goals and gaps. Before you can find the best LMS for your needs and move forward with an implementation project plan, you need to spot the inefficiencies of your existing compliance training program. For example, your strategy might not facilitate real-world applications. Knowing this, you would want a compliance training LMS that bridges gaps and imparts practical experience.
2. Discover what motivates and drives employees. Employee gamification only works when employees are properly incentivized, so find out what motivates your team based on their backgrounds and experience levels. Whether a task is challenging or boring, people respond better when they are internally driven to succeed.
Do you need an intuitive LMS with a personalized dashboard? Are the introverts on your team more driven by badges and points than by a sense of competition? Conduct surveys to gauge expectations, and try to follow a 70:20:10 model of training amplified by gaming to foster experimentation and collaboration.
3. Choose the right rewards for desired outcomes. With the plethora of LMS choices on the market, you can select from rewards and mechanics that lead to the exact behaviors and criteria you desire. Want employees to achieve safety online training certifications? Reward “graduates” with points after they have displayed their proficiency. Reinforce favorable behaviors without punishing workers who lag behind. Carrots are far more effective than sticks.
4. Invest in a feature-rich, gamification-supported LMS. Your LMS should not only be user-friendly, but it should also be a portal to game-based learning support and an online asset library. Ideally, your gamified learning platform should include themes and templates that allow you to design visually appealing rewards without reinventing the wheel. Just make sure you have game-based reporting on your side, which makes it simple to track employee performance, completion rates, and other LMS metrics.
Implementing a gamification-based compliance training strategy requires careful budgeting, planning, and analysis. Once you find an LMS platform that delivers the features you need within your price range, you’ll be on your way to mitigating risks and retaining superstar employees. And thanks to gamification, everyone can have a little fun along the way.
SOURCE: Pappas, C. (10 October 2018) "4 best practices for implementing a gamification-based compliance training system" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/4-best-practices-for-implementing-a-gamification-based-compliance-training-system?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001
Severance plans: How savvy employers can stay ERISA compliant
How can employers’ severance plans stay ERISA compliant? There are significant advantages associated with ERISA severance plans. Continue reading to learn more.
An employer’s promise to provide severance benefits may be written or oral, formal or informal, and individual or group. Determining whether an ERISA plan already exists, or whether an employer wants its severance arrangement to be subject to ERISA, is an important consideration in determining an employer’s obligation and liabilities associated with a severance arrangement.
There are significant advantages associated with a severance arrangement that is an ERISA plan as discussed in detail below. An employer, however, cannot unilaterally decide that the severance arrangement is an ERISA plan. Instead, an employer, when designing and administering a severance arrangement, can take definitive steps to ensure that the arrangement is treated as an ERISA plan.
Employers may assume that the first step to ensure the existence of an ERISA plan is to have a written plan document, which is required by ERISA. Surprisingly, this is not necessarily determinative as to whether an ERISA plan exists. Courts have held that ERISA plans can exist without a written plan document and vice versa.
Case law has provided the broad outlines of the nature of an ERISA-governed severance plan. An essential characteristic of ERISA severance plans is that, by their nature, they necessitate “an ongoing administrative scheme.” Courts have looked at the following indicators when determining what constitutes an ongoing administrative scheme:
- The employer’s discretion in determining (1) eligibility for benefits or (2) available plan benefits
- The form of payment such as lump sums versus periodic payments
- Any ongoing demand on the employer’s assets such that there is an ongoing scheme to coordinate and control the distribution of benefits
- Calculations based on certain factors such as job performance, length of service, reemployment prospects, and so forth.
Severance plans or arrangements that normally do not require an ongoing administrative scheme, and therefore, do not implicate ERISA, are plans that have lump-sum payments that are calculated under a formula and are mechanically triggered by a single event (such as termination). Where severance payments are made over time (through payroll, for example) and/or additional benefits (such as continuation of benefits or outplacement services) are provided, the severance arrangement is likely subject to ERISA.
As a practical matter, whether severance arrangements are ad hoc or recognized in a formal plan document, they may end up providing ERISA-covered benefits. In a dispute, an employer generally prefers that ERISA applies because of ERISA’s preemption of state laws. Preemption protects employers from state laws that may favor employees and generally limits the dispute to an ERISA claim for benefits, thereby avoiding the potential exposure to punitive, extra-contractual or special damages under state laws. In addition, ERISA’s claim procedure, which provides a pre-litigation administrative process for dispute resolution, will apply if proper plan language is provided. If employees with a severance claim fail to faithfully follow the ERISA claims procedure, their lawsuits may be dismissed for failure to exhaust administrative remedies.
Typically, the plan document gives the employer, in its capacity as plan administrator, the discretionary authority to interpret the plan’s language and make decisions about the plan. If the employee follows the claim procedures and the claim is denied, the decision-making process of the employer (or its designee) if done properly, is given deferential treatment by a reviewing court. Moreover, in many cases, judicial review is limited to only those matters addressed in the administrative record of the claim. In other words, many federal courts would decline to consider factual matters that were not raised by the employee in the claim procedure process.
Another consideration for the savvy employer is that severance benefits are almost always considered to be “welfare” benefits. Welfare benefits, as opposed to pension benefits, are afforded an extremely low level of protection under ERISA. Essentially, the employer’s exposure as to promised severance benefits is only as broad as its express contractual commitment to them. By appropriately documenting the benefits with “best practices” language (such as specifying that the amendment or termination of benefits may be done with or without advance notice), employers can take advantage of the opportunity afforded by the relatively thin protections provided by ERISA. On the other hand, poor or no documentation of a severance arrangement may leave an employer with difficult-to-prove assertions as to what severance commitments were actually made.
In summary, an ERISA-governed plan provides an employer with significant advantages in litigation. In addition, a severance arrangement subject to ERISA will enjoy the powerful benefits of ERISA preemption and the ERISA claims procedures.
SOURCE: Rothman, J.; Ninneman, S. (3 October 2018) "Severance plans, Part 1: How savvy employers can stay ERISA compliant" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/opinion/how-employers-can-stay-erisa-compliant-with-severance-plans
The approaching ACA premium tax moratorium – take 2
In 2010, Congress scheduled the 2014 Affordable Care Act premium tax. Then in 2015 Congress introduced a one-year moratorium on the premium tax that would take place in 2017. This past January, Congress placed another moratorium for the ACA premium tax in 2019. Continue reading to learn more.
In 2010, Congress scheduled the 2014 introduction of the Affordable Care Act premium tax (aka the health insurer fee). Then, via the PACE Act of October 2015, Congress placed a one-year moratorium on this 4% or so premium tax for calendar year 2017. You might recall our ensuing discussion a couple of years ago about how employers sponsoring fully insured medical, dental and/or vision plans could leverage this 2017 moratorium to their advantage.
See also: ACA: 4 things employers should focus on this fall
Meanwhile, did you notice back in January that Congress placed another moratorium on this tax, this time for 2019? To review:
- 2014-2016 – Tax applies
- 2017 – Under moratorium
- 2018 – Tax applies
- 2019 – Under moratorium
- 2020 – Tax scheduled to return
Fortunately, in moratorium years, fully insured medical, dental and vision premiums should be about 4% lower than they would have been otherwise, with these savings passed along proportionately by most employers to their plan participants.
Unfortunately, the budgetary challenge of this on-again-off-again Congressional approach is that when the tax returns, fully insured renewals naturally go up about 4% more than they would have otherwise. For example, an 8% premium increase becomes 12%.
See also: Proposals for Insurance Options That Don’t Comply with ACA Rules: Trade-offs In Cost and Regulation
Another complication occurs as employers annually compare the expected and maximum costs of self-funding their plans versus fully insuring the plans. Because this tax generally does not apply to self-funded plans, in “tax applies” years, any expected savings from self-funding will show about 4% higher than in moratorium years. This math especially complicates the financial comparison of level funding contracts to fully insured contracts (almost all level funding products are self-funded contracts).
With the Jan. 1 fully insured medical, dental and vision renewals beginning to cross our desks, what should employers do?
First, they should review the renewal’s rating methodology page and ensure that this tax was not included in the proposed 2019 premiums. If the rating methodology page was not provided, request it. If this request fails, ask for written confirmation that this tax is not included in your plan’s 2019 premiums.
Second, when comparing 2019 expected and maximum mature self-funded plan costs to 2019 fully insured premiums, extend the analysis to 2020 and project what will happen when this 4% fully insured tax tide returns.
See also: Pre-existing Conditions and Medical Underwriting in the Individual Insurance Market Prior to the ACA
Finally, complicating matters, several states, including Maryland, introduced new or higher state premium taxes for 2019. Ask your benefits consultant if these actions will impact your plans. For Maryland employers sponsoring fully insured plans, for example, the new additional one-year premium tax will essentially cancel out the 2019 ACA premium tax moratorium.
SOURCE: Pace, Z (27 September 2018) "The approaching ACA premium tax moratorium – take 2" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/the-approaching-obamacare-premium-tax-moratorium?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001










