5 ways employers can make diabetes education programs more inclusive
Employees struggling with diabetes often have to make difficult decisions when it comes to their medications. Often, it can be difficult to manage blood sugar daily and feel healthy enough to function at work. Read the following blog post from Employee Benefit News for five ways employers can make diabetes education programs more inclusive.
Diabetes doesn’t quit. Employees struggling with the disease often have to make difficult decisions about their medications. It can be hard to keep control of blood sugar every day and feel healthy enough to function well at work.
Many workers don’t tell their employer they have diabetes. Some 81% of benefits decision-makers believe employees with diabetes at their companies keep it a secret.
Giving voice to an issue is the first step toward solving it. Diabetes in the workplace is in need of attention: rates are rising in the U.S., as are the associated costs — unplanned missed workdays, reduced productivity and the stress associated with uncontrolled diabetes add up to billions of dollars per year.
To help employers find solutions, Roche Diabetes Care commissioned a survey of more than 200 benefits decision-makers at self-funded companies to learn their perceptions of the human and financial burden of diabetes. What’s clear is that addressing the myriad of concerns related to this condition is a top priority for benefits decision-makers; indeed, 70% say it keeps them awake at night.
Benefits decision-makers say the impact of diabetes on their companies is significant:
- More than one in four report diabetes results in increased costs to replace workers (28%), increased administrative and other indirect costs of managing absenteeism (29%);
- One in three believe diabetes results in indirect costs resulting from fatigue and understaffing as well as reduced productivity;
- One in four feel diabetes is responsible for poor morale among employees who must perform work to cover absent co-workers.
The majority (87%) agree it is vital that employers offer continual support to employees with diabetes. Listening, education and help simplifying everyday diabetes management emerge as ways employers can improve the health of their employees with diabetes and the company bottom lines. The following are five approaches to consider.
Cultivate a collaborative, supportive environment to encourage employees with diabetes to feel comfortable and at ease about sharing concerns.
Four in five (81%) benefits decision-makers surveyed say they believe employees keep their condition a secret. Fear of discrimination is one reason those with diabetes keep quiet along with the general sense that their colleagues and superiors just don’t know or understand what it’s like to live with the condition.
Secrets are also stressful. Employers can address this by including diabetes more frequently in workplace wellness education programs and discussions, and creating safe forums for employees with diabetes to share concerns and express their needs. Listening and making employees with diabetes part of a two-way dialogue demonstrate the company values not only their opinions but also their important contributions to the company community.
Designate private places at the office where employees with diabetes can test their blood sugar during the workday.
Some 90% of benefits decision-makers surveyed think their employees would value company access and time to monitor blood sugar or take injections.
Simplify daily diabetes management so employees have what they need to be in control of their blood sugar levels at home and at work.
People with diabetes have different concerns and different needs at different times. A company-sponsored program to simplify the daily decision-making and management of diabetes needs to be personalized, easily accessible and help the user keep track of their blood sugar levels automatically. Benefits decision-makers believe employers supported in this way would be:
- Less distracted and less stressed at work (37%);
- More productive (45%) and have better morale;
- Take fewer sick days (39%);
- Feel their employer cared about them (41%).
We have created a program that offers the elements that enable personalized accessible support. Participants say they feel more positively engaged in their daily management and more confident at work.
Demonstrate the value of supported employees with diabetes by measuring impact productivity and absenteeism.
Most of those surveyed say they believe company-supported programs that help employees with diabetes simplify daily management of the condition would have myriad benefits:
- 89% say it would lead to a higher quality of life and reduced sick time and related expenses;
- More than four in five say a company-supported program would result in more company loyalty and less turnover (83%) and contribute to increased productivity (84%);
- 90% believe employees with diabetes would feel more empowered at work if they participated in a company-supported program that helped them keep their blood sugar levels in control.
Consider conducting brief surveys of employees about their perceptions of diabetes. These can be done before or after education or awareness efforts are in place. For companies with support programs in place, surveys can be conducted among participants. Qualitative and quantitative data help demonstrate the value of these investments. Just asking the questions among employees show the company cares.
Show your successes; don’t just tell.
Show the value of educating about diabetes and supporting your employees with the condition. There are a number of ways to accomplish this. Collect and tell their stories. Create testimonials in articles for internal newsletters and videos that can be shown on monitors around the office. Stories are powerful ways to educate, build empathy and understanding, and perhaps most importantly, get the secret of diabetes out in the open.
SOURCE: Berman, A. (30 September 2019) "5 ways employers can make diabetes education programs more inclusive" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/how-to-make-diabetes-education-programs-more-inclusive
The Open Enrollment Checklist: Are You Poised for a Successful Season
Are you prepared for open enrollment? According to a recent survey, 56 percent of U.S. adults with employer-sponsored health benefits said health coverage satisfaction is a key factor in deciding whether they should leave their current job. Read this blog post from Employee Benefit News to learn more.
It’s here… the moment we’ve all been waiting for — or, in the case of HR, preparing for (at least we’d hope). That’s right, open enrollment season has arrived.
Open enrollment is a major opportunity for HR to contribute to their company’s performance — both in terms of healthcare savings and employee productivity. The better employees understand their benefits, the more likely they are to make cost-conscious decisions about their plan choices and their healthcare — saving themselves, and their employers, money. Not only that, but a recent survey found that 56% of U.S. adults with employer-sponsored health benefits said that whether or not they like their health coverage is a key factor in deciding to stay at their current job. And, interestingly, satisfaction with benefits and benefits communications have a tremendous impact on job satisfaction and engagement.
Not sure you’ve done everything you could to turn this annual necessity into a true financial, educational game-changer for your organizations? Ask yourself, did you:
Take stock of last year’s enrollment? Before diving into enrollment for 2020, employers should have taken stock of how the company fared last year. Post-mortem meetings with the enrollment team (along with key internal and external stakeholders) to assess what went well (or didn’t) can ensure the coming enrollment season runs smoothly.
In particular, identify the most time-consuming tasks and discuss how they could be streamlined in the future. Second, determine what questions employees asked the most about last year — and be prepared to answer them again this year. Third, consider whether the company achieved its overall open enrollment goals, and what contributed to those results. By addressing the peaks and pitfalls of last year’s season, HR should have a head start on planning for 2020.
Plan your communications strategy?With a defined approach to open enrollment in place, HR at this point should have developed an organized, well-communicated strategy to keep employees informed about their plan options at enrollment and throughout the year. Have you:
· Defined corporate objectives and how to measure success? · Assessed what messages to share with employees, especially anything that is changing — such as adding or eliminating plans or changing vendors? · Determined what information is best delivered in print (e.g. newsletters, posters, postcards, enrollment guides), online or in person through managers or one-on-one enrollment support? Adopting a multi-channel engagement strategy will ensure key messages reach the intended audience(s).
Make sure employees understand the deadline and process for enrolling — and the implications of missing the enrollment window. They must understand whether their existing coverage will roll over, if they’ll default to a specific plan and/or level of coverage (perhaps different from what they currently have), or end up with no coverage at all.
Take a pro-active approach to open enrollment? Ninety percent of employees report that they roll over their same health plan year over year — though this doesn’t indicate overwhelming plan satisfaction. More typically, it’s because they’re intimidated about what they don’t know, are confused about their choices or just don’t care. Employees don’t have the information they need, and aren’t likely to seek it out on their own.
Offering — or even requiring — one-on-one meetings with benefit experts during open enrollment provides a forum for employees to discuss their individual needs and ensure they are selecting the right coverage. These services — often available through brokers or outside engagement firms — provide employees with a safe space to ask specific questions about their health conditions, family history and potential life changes that could affect their insurance needs. This is the ideal time to remind employees that there is no one-size-fits-all plan, and that the least expensive plan on paper may not, ultimately, be the most cost-effective plan over time.
Revisit your SPD? The document we all love to hate, summary plan descriptions (SPDs) remain the best source for information about how each plan works, what it covers and the participant’s rights and responsibilities under that plan.
Having an SPD that is current, appealing (or at least not off-putting) and easy to access can answer many employee questions before they find their way to HR. Simple fixes like adding charts, callout boxes or icons can make your SPDs easier to navigate. Many employers are taking it a step further and offering interactive SPDs, which include robust search functionality and links to definitions, important forms, modeling tools and calculators, vendor sites and even short video clips. By making SPDs digital and interactive, employers can provide employees access to important information about their coverage 24/7 via any device. And, by adding a data analytics component, HR can track which sections employees visit most and pinpoint knowledge gaps about their benefit options to enhance understanding and drive increased benefits usage.
Account for all demographics? With all the focus on today’s multigenerational workforce, it’s important to remember that there’s more to “demographics” than age and gender. Worksite (office vs. shop floor vs. construction site vs. road warrior) can have a tremendous impact on the communications channels you use and when you use them.
And while some “generational generalizations” hold true — many older workers prefer paper, and most young people prefer mobile communication channels — it’s more important to look at employee cohorts from the perspective of differing priorities (planning for retirement vs. retiring student debt), different levels of education and healthcare literacy, and experience with choosing and using benefits. Employees just starting their careers are likely to need more support and different information than a more seasoned worker who’s had years of experience with the enrollment process. Consider the most effective ways to engage the different demographics of your population to gain their attention and interest in choosing the right plan for them.
Equip employees for smart healthcare choices year-round? For most employees, becoming an educated healthcare consumer is a work in progress — which is why many employers offer year-round resources to support smart healthcare choices. That said, these resources are often under-utilized because employees don’t know they exist.
Open enrollment is the perfect time to spread the word about these programs and address the key question for employees: “What’s in it for me?” For example, many employers offer transparency services, which enable employees to research the potential cost of care and compare prices across several providers in their area.
Other resources, such as benefits advocates, can answer questions from employees in real time — including where to get care, how to get a second opinion and what the doctor’s instructions really mean. When used in conjunction, transparency and advocacy services can lower out-of-pocket spending for the employee and reduce costs for the employer. Does your open enrollment communications strategy highlight that these resources exist, outline how they work and explain how they benefit the employee?
What if open enrollment is only a week away and you haven’t taken most, if any, of these steps? It’s not too early to start your to-do list for next year — perhaps by first tackling your SPD and drafting that communications plan. Most importantly, get that post-mortem meeting on the schedule now, while the lessons learned from this year’s open enrollment are still fresh.
SOURCE: Buckey, K. (3 October 2019) "The Open enrollment checklist: Are you Poised for a successful season" (Web Blog Post) https://www.benefitnews.com/list/the-employers-open-enrollment-checklist
Providing an HSA, FSA, or HRA Health Plan for your Employees
When open enrollment hits annually, it is not uncommon for employers to feel exasperated when staring down a list of acronyms such as HSA, FSA and HRA. As it should go without saying, the most common first thought is, “What does any of this mean?” Even the most seasoned experts have difficulty with understanding the complexities of various care options. That’s why in this installment of CenterStage, Kelley Bell, a Group Health Benefits Consultant at Saxon Financial, is here to break down the ‘alphabet soup’ that is HSAs, FSAs and HRAs.

What Is an HSA?
An HSA stands for a Health Savings Account. Kelley stated that HSAs work in conjunction with your existing HDHP plan (given you already have one) to cover costs associated with eligible medical, dental and vision expenses. Available to open just like a bank savings account, Kelley said, “It is your account; yours if you leave the employer and can contribute as long as you have an HDHP and can use the funds until they are gone, even if you are no longer in an HDHP.” For most, this applies to retirement. If you are reasonably healthy throughout your working life, Kelley said you can carry a large HSA balance into retirement. At that point, the funds can be used to cover the out-of-pocket medical costs that often increase with you as you age.
In addition to all the above, certain tax advantages exist within an HSA plan:
- Contributions are excluded from federal income tax.
- Interest earned is tax referable.
- Withdrawals for eligible expenses are exempt from federal income tax.
HSAs are typically available through employers, but individuals can establish one, as well. Many banks offer HSA programs for their customers, meaning if your employer does not offer the benefit, you can create an HSA account there.
What Is an FSA?
An FSA is a Flexible Savings Account. Much like an HSA, these plans cover the payment of medical, dental and vision-related expenses, and contributions you make to the plan are tax-deductible. Similarly, when you open an FSA account, you’re typically provided with a debit card or checkbook, so the funds can be accessed in the account. However, Kelley stated an FSA plan has a catch: “An FSA cannot roll over unused funds from year to year and is not portable.” Therefore, any contributions made to the plan that have not been spent by the end of the year are forfeited.
Some employers, as Kelley noted, do have options that will help you avoid complete forfeiture of unused funds. Certain employers allow their employees to carry over up to $500 of unused funds into the following year, while others will extend the use of the funds for up to two and a half months into the new year. Employers generally will offer one or the other, but never both. Some, however, offer no such option at all.
Kelley mentioned general purpose FSA coverage, and stated it can “make you ineligible for HSA contributions.” She continued to add that certain types will not prevent HSA eligibility, i.e. limited FSA for vision, dental, parking or “post-deductible FSA” which reimburses you for preventative care or for medical expenses that are incurred “after the minimum annual HDHP deductible has been met.” As a result of forfeiting any unused funds in the account, an FSA is best used by someone who has ongoing and predictable medical expenses. In this situation, it is likely you will deplete the funds in the account, whereas if you are considered healthy and have limited medical expenses (i.e. minor illness, sinus infection), the potential for forfeiture is high, and you may have to forgo the account. FSAs are employer-sponsored and typically are an option as part of a ‘cafeteria plan’.
What Is an HRA?
An HRA is a Health Reimbursement Arrangement. Like the other plans described in this article, an HRA is a tax-free employer funded amount of money for healthcare expenses. Contributions, as Kelley explained, “can be excluded from gross income, meaning that won’t pay taxes on that money and reimbursements from the HRA are tax-free when used for qualified medical expenses.” Depending upon the type of HRA, unused funds may or may not be rolled over from one year to the next. However, employers may also allow employees to use their HRA funds even into their retirement.
The benefits of an HRA take action after the employee has met a specific portion (i.e. employee meets 1st $2500 of a $5000 deductible), making it easier for the employee to meet their high deductible. HRAs are good for employers who want more control over how their medical dollars are put to use. Naturally, if the employer is paying the cost of the HRA, it can be of an increased advantage than contributory health insurance premiums and direct payment for out-of-pocket expenses. With an HRA, the employer determines the reimbursements and does not have to contribute the same amount for all employee groups (i.e. tiers of employee coverage, employee/child, employee/spouse and family).
How Saxon Helps
It is important to understand the needs of every client and educate their employees on how to use their healthcare. Saxon values client education and service above all else. We make educating employees a priority and ensure their benefits are understood and easy to use. Saxon represents all of the major carriers, allowing us to secure the best plans and rates for you and your staff, which we review annually.
If you are considering offering an HSA, FSA or HRA insurance plan to your employees, contact Kelley Bell today at (937) 672-1547 or kbell@gosaxon.com to begin exploring the benefits of adding this superior level of coverage today.
SIMPLE IRA vs. 401(k): How to Pick the Right Plan
Should you choose a SIMPLE IRA or a 401(k) for retirement saving? There are pros and cons to both types for employers. Read this blog post from NerdWallet for more on these two plan types and how to choose the right one for you.
The decision between a SIMPLE IRA and a 401(k) is, at its core, a choice between simplicity and flexibility for employers.
The aptly named SIMPLE IRA, which stands for Savings Incentive Match Plan for Employees, is the more straightforward of the two options. It’s quick to set up, and ongoing maintenance is easy and inexpensive. But if you have employees, you are required to provide contributions to their accounts. (See our SIMPLE IRA explainer.)
Although a 401(k) plan can be more complex to establish and maintain, it provides higher contribution limits and gives you more flexibility to decide if and how you want to contribute to employee accounts. Another big difference is that you can opt for a Roth version of the plan, whereas the SIMPLE IRA allows no Roth provision.
SIMPLE IRA vs. 401(k)
Here are the need-to-know differences between SIMPLE IRAs and 401(k)s:
SIMPLE IRA |
401(k) |
|
| Employer eligibility | Employers with 100 or fewer employees | Any employer with one or more employees |
| Employee eligibility | All employees who have compensation of at least $5,000 in any prior 2 years, and are reasonably expected to earn at least $5,000 in the current year |
All employees at least 21 years old who worked at least 1,000 hours in a previous year |
| Employer contribution rules |
|
|
| Contribution limits |
|
|
| Administrative responsibilities | No annual tax filing requirements; annual plan details must be sent to employees | Subject to annual compliance testing to ensure plan does not favor highly compensated employees |
| Fees | Minimal account fees | Varies by plan |
| Investment options | Any investments available through the financial institution that holds accounts | Investment selection curated by employer and plan administrator |
| Pros |
|
|
| Cons |
|
|
| More details | What Is a SIMPLE IRA? | What Is a 401(k)? |
SOURCE: IRS.gov
SIMPLE IRA or 401(k): How to decide
Startup costs and ease of setup often dictate the choice between retirement savings plans. But there are other factors to consider as well. To help decide which plan is best, answer the following questions:
Why are you setting up a retirement plan?
For many small-business owners, the answer is that they’re trying to maximize their own retirement savings dollars. If that’s the case, contribution limits should weigh heavily in your decision. For high earners especially, the higher contribution limit of the 401(k) makes it a more attractive choice than a SIMPLE IRA.
How important is it to offer the Roth option?
As mentioned earlier, the IRS allows employers to offer a Roth 401(k). (Quick reminder: A Roth 401(k) is funded with after-tax contributions in exchange for tax-free distributions in retirement.) There is no Roth version of the SIMPLE IRA. The account is subject to many of the same rules as a traditional IRA: Contributions reduce your taxable income for the year, but distributions in retirement are taxed as ordinary income. That said, the IRS allows participants to save in both a SIMPLE IRA and a Roth IRA at the same time.
Will you need to adjust employer contributions?
Although a nice perk to attract potential employees, employer contributions are not required of companies that offer 401(k) plans. You also have the freedom to set vesting terms, which allows you to require employees remain employed by you for a set time before taking ownership of your contributions to their accounts. Employer contributions to employee SIMPLE IRA accounts are mandatory, though you can choose between two matching arrangements dictated by the IRS. Contributions to a SIMPLE IRA are immediately 100% vested.
You have other choices
If you are self-employed or a small-business owner, SIMPLE IRAs and 401(k) plans aren’t your only options. There are a variety of retirement plans at your disposal.
For example, if you run a business with no employees, a solo 401(k) is worth considering. As the employer and (your own) employee, you’re allowed to contribute a total of up to $56,000 in 2019 (or $62,000 if you’re age 50 or older).
A SEP IRA also has a high contribution limit for business owners and self-employed individuals, though there is no catch-up contribution for savers 50 or older. The drawbacks: Like the SIMPLE IRA, a SEP requires employers to contribute to eligible employee accounts, and no Roth version is allowed.
We’ve laid out the pros and cons for these and other retirement plan options for the self-employed.
SOURCE: Yochim, D. (8 June 2019) "SIMPLE IRA vs. 401(k): How to Pick the Right Plan" (Web Blog Post). Retrieved from https://www.nerdwallet.com/blog/investing/simple-ira-vs-401k-comparison-how-to-pick-the-right-plan/
Simple Open-Enrollment Tips That Can Make a Big Difference
Many employees associate fear, anxiety or apprehension with open enrollment, the annual period when they select which employer-sponsored benefits they will have the coming year. Read this blog post from SHRM For a few simple tips to help out with this open enrollment season.
Trepidation is what comes to mind for many employees when asked their feelings about open enrollment, the annual period when they select employer-provided benefits for the coming year.
According to a nationally representative sample of 1,000 employees polled earlier this year, 33 percent cited "annoyance" or "dread" as their primary emotions when they thought about open enrollment and just 10 percent of workers said they were "confident" in the benefits choices they made when the enrollment process was over, according to VSP Vision Care's annual Open Talk about Open Enrollment survey.
In another survey, HR software company Namely found that 31 percent of employees give their employer a "C" or lower when it comes to open enrollment.
Here are some tips from benefits experts that will help you raise your grade this open-enrollment season.
What to Do, and Not to Do
Jennifer Benz, national practice leader at benefits communications firm Segal Benz, shared three bad HR practices that undermine open enrollment and three best practices for doing open enrollment the right way.
- Don't hide vital information from employees. Benz recalls how one company sent out its benefits materials but didn't include monthly costs. "A group of enterprising employees crunched the numbers and came up with estimates and circulated a rogue spreadsheet. Dealing with this communications fiasco took more work" than being upfront about costs, she noted.
Best practice: Be transparent and share the reasons you are making benefits changes. Break down the details and do the work for the employees. Provide scenarios so employees can better understand their options and cost breakdowns for different life situations.
- Don't cram in every benefit at once. Some companies hand out pages and pages of text, jamming a year's worth of communications into a few weeks, and figure they have done what they need to do. "What they have done is confused their employees," Benz said.
Best practices: Communicate the technical details of your various benefits over time. "Don't assume employees will weed through all your materials to make sense of the benefits offered to them," Benz said. Also make full use of visual aids. "Photos, icons, infographics, memes, charts, graphics and more—they all help to attract, and more importantly hold, people's attention," noted Amber Riley, a communications consultant to Segal Benz. "Whether you're driving an open-enrollment campaign, creating a new benefits guide or promoting a wellness program, when you increase the visual pleasure of what you are communicating, your people are more likely to engage, learn, understand and ultimately take action."
- Don't give employees too little time to process their open-enrollment choices. While many people wait until the last day to fill out the health care selection forms, they may have been considering their options with family members for weeks, so giving them just a few days to make decisions is not going to be enough.
Best practice: Build in a time frame that gives HR staff and employees the time they need. Benz recommended three weeks.
"People are always talking about learning from the best practices and success stories, but you can also learn a lot from other companies' mistakes," she noted. "When you prepare for enrollment in advance and anticipate issues—including those you and others have experienced in the past—you are better-equipped to avoid missteps. Your employees will notice and appreciate the extra effort."
Help Employees Ace Open Enrollment
"Open enrollment is often time-consuming and confusing for employees, but these choices can make a huge financial impact," said Julie Stich, CEBS, vice president of content at the International Foundation of Employee Benefit Plans, an association of benefit plan sponsors. She suggested that HR share the following advice with employees to help prepare them for the upcoming enrollment season:
- Take your time. Take time to really read through the enrollment materials you receive. If you are invited to a face-to-face meeting, make time to attend. It's possible you'll be offered different plan options and coverages this year. The better you understand the changes, the better decisions you'll make.
-
Take a trip down memory lane. Think back to what happened in your life this year. How often did you and your family members need medical services? What kind? Are any treatments ongoing? Think about any life changes that could affect the benefits you need, like a marriage or divorce, a child going off to college, or a spouse changing jobs.
- Look ahead. Consider what the next year will look like for you and your family. Are you planning to have a baby? Knee replacement surgery? A root canal? Does someone need braces? New glasses? Keep this in mind as you look at your coverage options.
- Dive into the details. It's important to note whether the plans' provider networks have changed. Make sure your doctors are still in-network. Is your chiropractor also covered? Does the plan cover orthodontics? Is your spouse's daily prescription drug covered, and did the coverage change? Also consider areas of need like access to specialists, mental health care, therapies, complementary and alternative medicine, and chronic care. Look at the options offered in all plans, including health, dental, vision and disability.
- Get out your calculator. Add up the amount you'll need to pay toward your health premium plus deductibles, co-payments (flat-dollar amounts) for prescriptions and doctor office visits, and co-insurance (a percentage of the cost you'll pay) for services. Understand what you'll be asked to pay if you seek care outside your network. This will give you a clearer picture of how much you're likely to spend. The plan that looks to be the cheapest option may not really be the cheapest for you.
- Determine what's right for you. Consider your comfort level with risk. If you want your family to be covered for every eventuality, a more traditional plan, if one is offered, might be right for you. If you're comfortable taking on some upfront costs, a high-deductible plan with a lower premium ight be your plan of choice.
- Take advantage of extras. Your employer may offer the option to reduce your health premiums in exchange for your participation in a wellness program or health-risk assessment. It may match some or all of the money you save in your 401(k) plan. It might let you set aside tax-deferred money into a health savings account or flexible spending account. Also, check with your employer to see if it offers voluntary insurance with a group discount and payroll deduction for premiums—like critical-illness, pet, auto and homeowners coverage. If these options work for your situation, sign up.
- Ask questions. Don't be shy about asking your HR or benefits department to explain something if you're not sure. They're there to help and want you to make the best decisions for your situation.
"Taking the time upfront to carefully choose the best options will help employees better manage their finances throughout the year, alleviating stress and promoting productivity," Stich said.
SOURCE: Miller, S. (24 September 2019) "Simple Open-Enrollment Tips That Can Make a Big Difference" (Web Blog Post). Retrieved from https://www.shrm.org/ResourcesAndTools/hr-topics/benefits/Pages/simple-open-enrollment-tips-make-a-big-difference.aspx
‘Eye’ spy a savings opportunity for health and vision benefits
The National Eye Institute reported that 61 million adults are at high risk for serious vision loss. Conventionally, vision benefits were offered as an elective, with coverage is focusing on vision tests or discounts for corrective eyewear. Read the following blog post to learn more about vision benefits.
Sixty-one million adults are at high risk for serious vision loss, according to the National Eye Institute, but most U.S. employers don’t include eye care as part of their benefits package. Vision benefits have traditionally been offered as an elective, where coverage is focused on vision tests or discounts for corrective eyewear.
This often results in inadequate coverage for employees and dependents, which can result in unrecognized and untreated issues that impact employee health and productivity, as well as an employer’s bottom line.
Comprehensive eye exams are recommended for adults under the age of 65 at least every two years, according to the American Optometric Association (AOA). These exams are the only way a doctor can detect signs and symptoms of serious conditions without cutting into or scanning body parts.
The total economic burden of eye disorders and vision loss in the U.S. was $139 billion in 2013, which includes $65 billion in direct medical costs strictly due to eye disorders and low vision. Loss of vision among workers results in $48 billion in lost productivity per year.
When it comes to benefit management priorities employers often focus more on chronic condition management. Yet, eye health is often linked to common chronic conditions including diabetes and hypertension. Without early detection of eye and vision health issues, employees cannot properly manage these conditions. Delaying medical treatment can lead to increased absenteeism and reduced productivity, eventually resulting in treatment that comes too late, and at a much higher price tag for employers, employees and family members.
About 68% of Americans with diabetes have been diagnosed with eye complications, many of which could have been prevented through a comprehensive eye exam. Diabetes is the leading cause of blindness among adults, according to the National Institutes of Health. Its prevalence is increasing as one in 10 people worldwide may be affected by 2040, according to research from the International Diabetes Federation.
Nearly half of Americans don’t know that diabetic eye diseases have visible symptoms, according to a 2018 AOA survey. More than one-third of respondents didn’t know a comprehensive eye exam is the only way to determine if a person’s diabetes will cause blindness. These exams, considered the gold standard in clinical vision care, should be covered under the employees’ medical benefits.
Three years ago the Midwest Business Group on Health began a collaboration with the AOA to better understand how employers think about and implement eye health and vision benefits. As part of this partnership, a no-cost eye care benefits toolkit was developed to support employers in evaluating their current eye health and vision care benefits to:
- Understand the importance of early detection so that employees can effectively manage chronic and more serious conditions
- Recognize how to integrate primary and preventive eye care into an overall medical benefit design
- Educate employees on the importance of periodic eye examinations
It’s important that employers better understand the impact of vision care benefits, including lower costs, better employee health, improved job satisfaction, better employee quality of life, and work productivity.
SOURCE: Larson, C. (20 September 2019) "‘Eye’ spy a savings opportunity for health and vision benefits" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/vision-loss-resulting-in-billions-in-lost-productivity
DOL issues finalized overtime regulation
The DOL recently released their finalized overtime rule. This new rule raises the minimum salary level to $35,568 per year for a full-year worker to earn overtime wages. Read this blog post from Employee Benefit News to learn more about this new rule.
The DOL on Tuesday released its highly anticipated finalized overtime rule, raising the minimum salary level to $35,568 per year for a full-year worker to earn overtime wages.
“Today’s rule is a thoughtful product informed by public comment, listening sessions and long-standing calculations,” Wage and Hour Division Administrator Cheryl Stanton says in a statement. “The DOL’s wage and hour division now turns to help employers comply and ensure that workers will be receiving their overtime pay.”
The final rule, effective Jan. 1, 2020, updates the earnings thresholds necessary to exempt executive, administrative or professional employees from the FLSA’s minimum wage and overtime pay requirements, and allows employers to count a portion of certain bonuses (and commissions) toward meeting the salary level.
The new thresholds account for growth in employee earnings since the currently enforced thresholds were set in 2004. In the final rule, the department is:
- Raising the standard salary level from the currently enforced level of $455 to $684 per week (equivalent to $35,568 per year for a full-year worker);
- Raising the total annual compensation level for highly compensated employees from the currently-enforced level of $100,000 to $107,432 per year;
- Allowing employers to use nondiscretionary bonuses and incentive payments (including commissions) that are paid at least annually to satisfy up to 10% of the standard salary level, in recognition of evolving pay practices; and
- Revising the special salary levels for workers in U.S. territories and in the motion picture industry.
This finalized rule is a shift from the previous administration's proposed rule, which would have doubled the salary threshold.
Under the Obama administration, the Labor Department in 2016 raised the minimum salary to roughly $47,000, extending mandatory overtime pay to nearly 4 million U.S. employees. But the following year, a federal judge in Texas ruled that the ceiling was set so high that it could sweep in some management workers who are supposed to be exempt from overtime pay protections. Business groups and 21 Republican-led states then sued, challenging the rule.
The overturning of the 2016 rule that increased the salary level from the 2004 level has created a lot of uncertainty, says Susan Harthill, a partner with Morgan Lewis. The best way to create certainty is to issue a new regulation, which is what the administration's done, Harthill adds.
While the final rule largely tracks the draft, there are two changes that should be noted: the salary level is $5 higher and the highly compensated employee salary level is dramatically reduced from the proposed level, she says.
“This is an effort to find a middle ground, and while it may be challenged by either or maybe both sides, the DOL’s salary test sets a clear dividing line between employees who must be paid overtime if they work more than 40 hours per week and employees whose eligibility for overtime varies based on their job duties,” Harthill adds.
The DOL estimates 1.3 million employees could now be eligible for overtime pay under this rule (employees who earn between $23,600 and $35,368 no longer qualify for the exemption).
A majority of business groups were critical of Obama’s overtime rule, citing the burdens it placed particularly on small businesses that would be forced to roll out new systems for tracking hours, recordkeeping and reporting.
SHRM, for example, expressed it's opposition to the rule, noting it would have fundamentally changed the rules for employee classification, dramatically increased the salary under which employees are eligible for overtime and provided for automatic increases in the salary level without employer input.
“Today’s announcement finalizing DOL’s overtime rule provides much-needed clarity for workplaces," SHRM says in a statement. "This rule marks the first increase to the salary threshold since 2004 and gives employers more flexibility to plan for the future. We appreciate DOL’s willingness to work with SHRM, other organizations and America’s workers to enact an overtime rule that benefits both employers and their employees.”
But the finalized rule still will have implications for employers.
“Education and health services, wholesale and retail trade, and professional and business services, are the most impacted industries, according to DOL, but all industries are potentially impacted,” Harthill, also former DOL deputy solicitor of labor for national operations, adds. “Also often overlooked is the impact on nonprofits and state and local governments, which are subject to the FLSA and often have lower salaries.”
All companies should be taking a close look at their employees to make sure workers are properly classified, but what they do after that will depend entirely on individual business needs, she says. “Some will hire additional employees to reduce the amount of overtime, while others will just pay overtime if their workers in this salary bracket spend more than 40 hours a week on the job.”
Employers who haven’t already reviewed their exempt workforce should do so now, before the Jan. 1 effective date, Harthill advises.
“They can opt to pay overtime, raise salary levels above $35,368, or review and tighten policies to ensure employees do not work more than 40 hours per week,” she says. “There could be job positions that need to be reclassified and that might have a knock-on effect for employees who earn above the new salary level.”
Many employers increased their salaries when DOL issued the 2016 rule, and some states have higher salary levels, so not all businesses will need to make an adjustment. “But even those employers should review their highly compensated employees — they may still be exempt even if they earn less than $107,432 but the analysis will be more complicated,” she adds.
“We did not hear any objections from employers when these rules were initially proposed," adds Jason Hammersla, vice president of communications at the American Benefits Council. "That said, aside from the obvious compensation and payroll tax implications, this rulemaking is significant for employers who include overtime compensation in the formula for retirement plan contributions as it could increase any required employer contributions."
"The change could also affect plans that exclude overtime pay from the plan’s definition of compensation if the new overtime pay causes the plan to become discriminatory in favor of highly compensated employees," he adds.
SOURCE: Otto, N. (24 September 2019) "DOL issues finalized overtime regulation" (Web Blog Post). Retrieved from https://www.benefitnews.com/news/dol-issues-finalized-overtime-regulation
Health insurance surpass $20,000 per year, hitting a record
According to an annual survey of employers, the cost of family health coverage has now surpassed $20,000, a record high. The survey also revealed that while most employers pay most of the costs of coverage, workers' average contribution for a family plan is now $6,000. Read this blog post from Employee Benefit News to learn more.
The cost of family health coverage in the U.S. now tops $20,000, an annual survey of employers found, a record high that has pushed an increasing number of American workers into plans that cover less or cost more, or force them out of the insurance market entirely.
“It’s as much as buying a basic economy car,” said Drew Altman, chief executive officer of the Kaiser Family Foundation, “but buying it every year.” The nonprofit health research group conducts the yearly survey of coverage that people get through work, the main source of insurance in the U.S. for people under age 65.
While employers pay most of the costs of coverage, according to the survey, workers’ average contribution is now $6,000 for a family plan. That’s just their share of upfront premiums, and doesn’t include co-payments, deductibles and other forms of cost-sharing once they need care.
The seemingly inexorable rise of costs has led to deep frustration with U.S. healthcare, prompting questions about whether a system where coverage is tied to a job can survive. As premiums and deductibles have increased in the last two decades, the percentage of workers covered has slipped as employers dropped coverage and some workers chose not to enroll. Fewer Americans under 65 had employer coverage in 2017 than in 1999, according to a separate Kaiser Family Foundation analysis of federal data. That’s despite the fact that the U.S. economy employed 17 million more people in 2017 than in 1999.
“What we’ve been seeing is a slow, slow kind of drip-drip erosion in employer coverage,” Altman said.
Employees’ costs for healthcare are rising more quickly than wages or overall economy-wide prices, and the working poor have been particularly hard-hit. In firms where more than 35% of employees earn less than $25,000 a year, workers would have to contribute more than $7,000 for a family health plan. It’s an expense that Altman calls “just flat-out not affordable.” Only one-third of employees at such firms are on their employer’s health plans, compared with 63% at higher-wage firms, according to the Kaiser Family Foundation’s data.
The survey is based on responses from more than 2,000 randomly selected employers with at least three workers, including private firms and non-federal public employers.
Deductibles are rising even faster than premiums, meaning that patients are on the hook for more of their medical costs upfront. For a single person, the average deductible in 2019 was $1,396, up from $533 in 2009. A typical household with employer health coverage spends about $800 a year in out-of-pocket costs, not counting premiums, according to research from the Commonwealth Fund. At the high end of the range, those costs can top $5,000 a year.
While raising deductibles can moderate premiums, it also increases costs for people with an illness or who gets hurt. “Cost-sharing is a tax on the sick,” said Mark Fendrick, director of the Center for Value-Based Insurance Design at the University of Michigan.
Under the Affordable Care Act, insurance plans must cover certain preventive services such as immunizations and annual wellness visits without patient cost-sharing. But patients still have to pay out-of-pocket for other essential care, such as medication for chronic conditions like diabetes or high blood pressure, until they meet their deductibles.
Many Americans aren’t prepared for the risks that deductibles transfer to patients. Almost 40% of adults can’t pay an unexpected $400 expense without borrowing or selling an asset, according to a Federal Reserve survey from May.
That’s a problem, Fendrick said. “My patient should not have to have a bake sale to afford her insulin,” he said.
After years of pushing healthcare costs onto workers, some employers are pressing pause. Delta Air Lines Inc. recently froze employees’ contributions to premiums for two years, Chief Executive Officer Ed Bastian said in an interview at Bloomberg’s headquarters in New York last week.
“We said we’re not going to raise them. We're going to absorb the cost because we need to make certain people know that their benefits structure is real important,” Bastian said. He said the company’s healthcare costs are growing by double-digits. The Atlanta-based company has more than 80,000 employees around the globe.
Some large employers have reversed course on asking workers to take on more costs, according to a separate survey from the National Business Group on Health. In 2020, fewer companies will limit employees to so-called “consumer-directed health plans,” which pair high-deductible coverage with savings accounts for medical spending funded by workers and employers, according to the survey. That will be the only plan available at 25% of large employers in the survey, down from 39% in 2018.
Employers have to balance their desire to control costs with their need to attract and keep workers, said Kaiser’s Altman. That leaves them less inclined to make aggressive moves to tackle underlying medical costs, such as by cutting high-cost hospitals out of their networks. In recent years employers’ healthcare costs have remained steady as a share of their total compensation expenses.
“There’s a lot of gnashing of teeth,” Altman said, “but if you look at what they do, not what they say, it’s reasonably vanilla.”
SOURCE: Tozzi, J. (25 September 2019) "Health insurance surpass $20,000 per year, hitting a record" (Web Blog Post). Retrieved from https://www.benefitnews.com/articles/health-insurance-costs-surpass-20-000-per-year
6 voluntary benefits your employees want
Multigenerational workforces are no longer finding the run-of-the-mill benefits plans adequate. This is making voluntary benefits more important than ever in this age of the multigenerational workforce and a tight labor market. Read this blog post from for six voluntary benefits employees want.
In this age of the multigenerational workforce and a tight labor market, a one-size-fits-all group benefits model with medical, prescription, dental, vision and a retirement plan just doesn’t cut it. A workforce with Baby Boomers, Gen X’ers, Millennials and Generation Z means that employees are going to find the run-of-the-mill benefits plan inadequate. Ditto for job seekers.
What follows is that voluntary benefits are more important than ever. Offering a range of voluntary benefits can help meet the needs of employees at all life stages.
Voluntary benefits add value to benefit plans and are typically easy to administer. They’re low-to-no-cost because employees pay for them, and maintenance is often handled through a payroll deduction. Many voluntary benefits also offer guaranteed acceptance at a lower rate than medical benefits, so even if a small group within your company chooses a particular benefit, they’ll be covered.
This landscape is changing quickly. Here are six trending voluntary benefits your employees want.
Student loan debt repayment assistance
Debt among college graduates has grown to nearly $1.6 trillion. It’s preventing the largest employee segment at most companies from buying houses or cars, saving for retirement, having kids and getting married. To help employees repay their student loan debt, some employers are helping employees pay down student loan debt through a direct payroll deduction.
Others are offering a new, IRS-allowable retirement plan match swap where an employer can opt to increase its defined contribution match, enabling employees to reduce their retirement match and contribute funds to repaying student loans instead.
Interest in this benefit continues to grow. Employers looking to offer student loan debt repayment should be aware that not all platforms are created equal. Look out for high per-employee, per-month fees.
Individual long-term care
A growing number of people are beginning to understand the value of long-term care insurance because they have taken care of or currently care for a friend or relative who needs round-the-clock care. Long-term care insurance covers home or institutional care if a person is no longer able to perform at least two activities of daily living--eating, bathing, dressing, moving from a bed to a chair or using a toilet.
Employees are interested in buying long-term care insurance through their employer because they can offer better rates for simplified issue plans. If you plan to offer long-term care as an employer-sponsored benefit, I recommended rolling it out with a strategic project plan and a benefit counselor or a technology platform capable of providing decision-making tools for a smooth application process.
Executive reimbursement plans
Employee retention — especially executive retention — is on the minds of many employers in the midst of this thriving economy. Filling gaps in medical and prescription coverage is one way to provide executive teams with premium benefits they may be looking for.
Executive reimbursement plans provide reimbursement for out-of-pocket expenses, access to facilities and level of service not normally covered under most group health plans. Rather than simply increasing compensation to help cover out-of-pocket expenses, premiums for these plans are tax-deductible for the employer, and benefits are non-taxable for employees.
Executive individual disability insurance
Traditional employer-sponsored long-term disability (LTD) is likely not enough coverage for highly-compensated employees or some sales staff who depends heavily on commission and bonuses. Normally, LTD pays employees 50-70% of their salary up to a certain amount.
Employers can carve out additional coverage for employees based on their management level, performance or tenure. Individual disability insurance plans can protect employees until they turn 65; they can also protect job titles or levels until employees are well enough to return to work. Executive individual disability insurance, like executive reimbursement, can be offered as a form of compensation, or a form of financial asset protection for higher incomes.
Telemedicine
The rise of consumer-driven health plans has led to the need for telemedicine. Telemedicine provides a way for employees to see a physician or provider by video and get a diagnosis and/or prescription quickly. The success of telemedicine is leading some carriers to integrate it within their plan. However, standalones still exist and can provide employees with an easy way to get care faster and cheaper than before.
Pet Insurance
Pet parents spend nearly $70 billion on veterinarian costs for their pets, but just 10% of dogs and 5% of cats are covered by medical insurance. As pets begin to play a larger role in our lives, more employers are offering pet insurance to their employees to help defray the cost of unexpected medical expenses.
There are a number of plan options, and setting up a plan for employees’ pets is simple. However, it’s vital that employers do their research to ensure the veterinarian network includes the best vets.
As part of a voluntary benefit offering, be sure to develop a rollout strategy and communications plan so employees are thoroughly educated and you meet group minimums.
SOURCE: Park, N. (25 September 2019) "6 voluntary benefits your employees want" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/6-voluntary-benefits-your-employees-want
4 pitfalls of paid leave and how clients can avoid them
Employers are using paid leave options to help boost their employee benefits packages in efforts to better attract and retain talent. Read the following blog post from Employee Benefit Advisor for 4 common pitfalls of paid leave and how employers can avoid them.
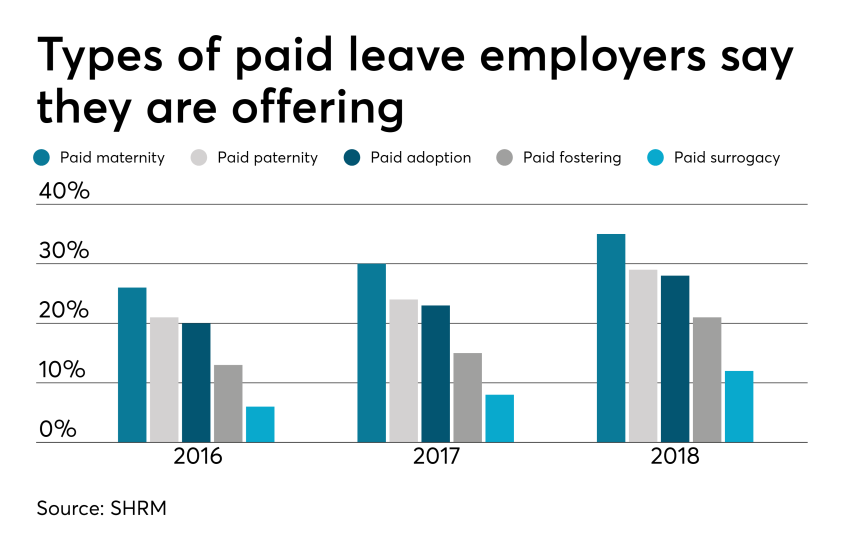 Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
But some employers are getting themselves into trouble in the process, facing accusations of gender discrimination or improper use of leave.
Here are four potential pitfalls of paid leave, and how employers can avoid them.
1. Be careful what you call “maternity leave.”
Employers have long been granting leave for new moms in the form of disability coverage. In fact, the top cause of short term disability is pregnancy. Disability insurance usually grants new moms six to eight weeks of paid leave to recover from childbirth.
Because this coverage applies to the medical condition of recovering from childbirth, it shouldn’t be lumped in with bonding leave.
Guidance from the Equal Employment Opportunity Commission says leave granted for new moms for bonding must also be extended to new dads, so separating disability leave from bonding leave is crucial to avoiding gender discrimination.
2. Don’t make gender assumptions.
The amount of bonding time for new parents after birth, adoption or fostering must be granted equally for men and women. Companies that don’t provide the same amount of paid leave for men and women may find themselves in a discrimination lawsuit.
It’s not just the time away from work that matters, but also the return-to-work support provided. If new moms are granted temporary or modified work schedules to ease the transition back to work, new dads must also have access to this.
Some companies may choose to differentiate the amount of leave and return-to-work support for primary or secondary caregivers. That’s compliant as long as assumptions aren’t made on which gender is the primary or secondary caregiver.
The best way to avoid potential gender discrimination pitfalls is to keep all parental bonding and related return-to-work policies gender neutral.
3. Avoid assuming the length of disability.
Be careful about assuming the length of time a new mom is disabled, or recovering medically, after birth. Typical coverage policies allot six to eight weeks of recovery for a normal pregnancy, so assuming a new mom may be out for 10 weeks might be overestimating the medical recovery time, and under-representing the bonding time, which must be gender neutral.
4. Keep up with federal, state and local laws.
Mandated leave laws are ever-evolving, so employers should consistently cross-check their policies with state and local laws. For instance, do local paid leave laws treat adoption the same as birth? Are multistate employers compliant? What if an employee lives in one state but works in another: Which state’s leave policies take precedence?
Partnering with a paid leave service provider can mitigate the risk of improperly administering leave. Paid leave experts can help answer questions, review guidelines and provide information regarding job-protecting medical or family leave.
They can also help flag potential pitfalls, ensuring leave requests from all areas of your company are managed uniformly and in accordance with state and federal laws, including the EEOC.
SOURCE: Bennett, A. (12 September 2019) "4 pitfalls of paid leave and how clients can avoid them" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/list/4-pitfalls-of-paid-leave-and-how-clients-can-avoid-them










