Apple launching concierge health care centers for employees
Did you know Apple is now offering healthcare centers for their employees? Check out this article from Benefit Pro for further information.
This spring, Apple employees will see the first phase of Apple’s new approach to employee health care: on-site health clinics.
According to Healthcare IT News, Apple plans to launch a group of internal health centers as it moves to boost the health and wellness of its employees. According to the report, the company has already “quietly published a webpage for the program, called AC Wellness Network, which includes a description of the company’s goals as well as information on a number of open positions.”
“AC Wellness Network believes that having trusting, accessible relationships with our patients, enabled by technology, promotes high-quality care and a unique patient experience,” Apple has said on the webpage. It continues, “The centers offer a unique concierge-like healthcare experience for employees and their dependents. Candidates must have an appreciation for the patient experience and passion for wellness and population health—integrating best clinical practices and technology in a manner that drives patient engagement.”
Apple’s move comes in the wake of an earlier declared partnership among Amazon, JPMorgan Chase and Berkshire Hathaway for their own independent health care company intended to bolster employee health at lower cost than conventional providers.
AC Wellness, says the report, will exist as “an independent medical practice,” although the company is a subsidiary of Apple. Job listings include not just physicians but also such positions as workflow designers, and the website listings suggest the first centers will be located in Santa Clara, California and in the company’s Cupertino, California campus.
Other recent health care steps taken by the company, according to an HRDive report, include its January announcement that it is making personal health records accessible on the latest iPhones, as well as its exploration of ways its Apple Watch could have medical applications, like detecting irregular heartbeats in wearers.
According to a CNBC report, some former Stanford Health Care employees have been affiliated with AC Wellness for at least five months. Says Healthcare IT News, “[t]hese sources also said that Apple will use the centers as a testing ground for its upcoming health and wellness products prior to large-scale consumer rollout, and that the company notified third-party vendors this week about its upcoming health clinics.”
Read the article.
Source: Satter M. (1 March 2018). "Apple launching concierge health care centers for employees" [Web Blog Post]. Retrieved from address https://www.benefitspro.com/2018/03/01/apple-launching-concierge-health-care-centers-for/
Employer Responsibility Under the Affordable Care Act
Here's a helpful chart from the Kaiser Family Foundation to decipher the penalties employers may have for not offering ACA coverage in 2018.
The Affordable Care Act does not require businesses to provide health benefits to their workers, but applicable large employers may face penalties if they don’t make affordable coverage available. The employer shared responsibility provision of the Affordable Care Act penalizes employers who either do not offer coverage or do not offer coverage that meets minimum value and affordability standards. These penalties apply to firms with 50 or more full-time equivalent employees. This flowchart illustrates how those employer responsibilities work.
Read the article.
Source:
Kaiser Family Foundation (5 March 2018). "Employer Responsibility Under the Affordable Care Act" [Web Blog Post]. Retrieved from address https://www.kff.org/infographic/employer-responsibility-under-the-affordable-care-act/
Strengthening the Relationship between Education and Employers: Johnny C. Taylor, Jr., Appointed Chair of President’s Board of Advisors on HBCUs
From the SHRM CEO, here is his opinion on the newly appointed Chair of President’s Board of Advisors on HBCUs.
Johnny C. Taylor, Jr., SHRM-SCP, president and chief executive officer of the Society for Human Resource Management, was appointed chair of the President’s Board of Advisors on Historically Black Colleges and Universities (HBCUs) at a White House ceremony today.
In accepting the volunteer advisory appointment to the White House Initiative on HBCUs by President Donald Trump, Taylor gave these remarks:
Thank you, President Trump and Secretary DeVos.
I appreciate the trust you have placed in me to chair the President’s Board of Advisors on HBCUs. It has been my life’s work to unleash talent — in all its forms, from wherever it originates.
As CEO of the Society for Human Resource Management (SHRM), I work with employers across the country. No matter their industry, size or longevity, today’s organizations all share the same challenge — closing the skills gap while building diverse, inclusive, engaged workforces.
For each of them, the “War for Talent” will never end and, thanks to this incredibly strong economy we’re experiencing, it is now a way of life. And today, people are an organization’s only competitive edge.
Employers depend on our country’s educational institutions as a reliable source of the multi-faceted talent they need. HBCUs are a critical conduit for this talent. Every year, over 300,000 students turn to these institutions for their education and to prepare them for their careers.
This President’s Advisory Board can be the nexus between higher education institutions and employers. As a CEO (in both non-profit and for-profit businesses), a former Fortune 500 chief HR executive, and someone with over 7½ years of experience in the HBCU space, I am up for this very challenge.
At SHRM, we are the experts on people and work and on building powerfully diverse organizational cultures that drive success. SHRM’s 300,000 members impact the lives of over 100 million people in the American workforce. SHRM is also an experienced academic partner, currently providing human resources curricula through 465 programs on 354 college campuses.
By working together, across all sectors, the HR profession, HBCUs and this Advisory Board can strengthen the relationship between education and employers. This Advisory Board can facilitate this critical relationship and support innovations in work-based learning opportunities for HBCU students. And as the world’s largest human resources association, SHRM can work with CEOs to connect industry to the diverse talent at these institutions.
This Board has an incredible opportunity to highlight HBCUs as wellsprings of the diverse talent American employers want and need today. HR and education, along with the support of this administration, must move together, forward.
Read the article.
Source: SHRM (27 February 2018). "Strengthening the Relationship between Education and Employers: Johnny C. Taylor, Jr., Appointed Chair of President’s Board of Advisors on HBCUs" [Web Blog Post]. Retrieved from address https://blog.shrm.org/blog/strengthening-the-relationship-between-education-and-employers-johnny-c-tay
Ahead of the Midterms, Voters across Parties See Costs as their Top Health Care Concern
From Kaiser Health News is this poll deciphering where the public sits ahead of Midterms. What is there top healthcare concern? Costs. Get all the information in this article.
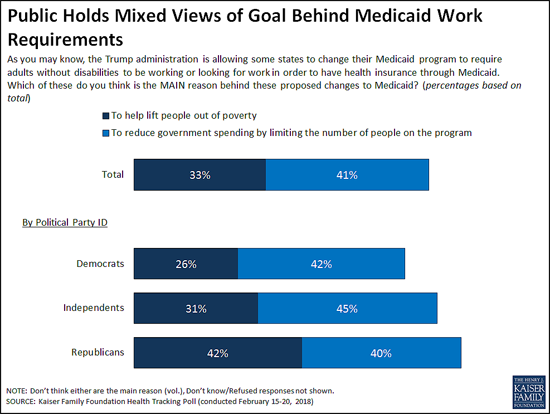
At a time when the Trump Administration is encouraging state efforts to revamp their Medicaid programs through waivers, the latest Kaiser Family Foundation tracking poll finds the public splits on whether the reason behind proposals to impose work requirements on some low-income Medicaid beneficiaries is to lift people out of poverty or to reduce spending.
The Centers for Medicare and Medicaid Services in January provided new guidance to states and has since approved such waivers in two states (Kentucky and Indiana). Eight other states have pending requests
When asked the goal of work requirements, four in 10 (41%) say it is to reduce government spending by limiting the people enrolled in the program, while a third (33%) say it is to lift people out of poverty as proponents say.
While larger shares of Democrats and independents say the reason is to cut costs, Republicans are more divided, with roughly equal shares saying it is to lift people out of poverty (42%) as to reduce government spending (40%). People living in the 10 states that have approved or pending work requirement waivers are similarly divided, with near-equal shares saying the goal is to lift people out of poverty (37%) as to reduce government spending (36%). This holds true even when controlling for other demographic variables including party identification and income.
In addition to work requirements, five states are currently seeking Medicaid waivers to impose lifetime limits on the benefits that non-disabled adults could receive under the Medicaid program. The poll finds the public skeptical of such a shift, with two thirds (66%) saying Medicaid should be available to low-income people as long as they qualify, twice the share (33%) as say it should only provide temporary help for a limited time.
Substantial majorities of Democrats (84%) and independents (64%) say Medicaid should be available without lifetime limits, while Republicans are divided with similar shares favoring time limits (51%) and opposing them (47%).
These views may reflect people’s personal experiences with Medicaid and the generally positive views the public has toward the current program, which provides health coverage and long-term care to tens of millions of low-income adults and children nationally.
Seven in 10 Americans report a personal connection to Medicaid at some point in their lives – either directly through their own health insurance coverage (32%) or their child being covered (9%), or indirectly through a friend or other family member (29%).
Three in four (74%) hold favorable views of Medicaid, including significant majorities of Democrats (83%), independents (74%) and Republicans (65%). About half (52%) of the public say the current Medicaid program is working well for low-income enrollees, while about a third (32%) say it is not working well.
Most Residents of Non-Expansion States Favor Medicaid Expansion to Cover More Low-Income People
Under the Affordable Care Act, most states expanded their Medicaid programs to cover more low-income adults. In the 18 states that have not done so, a majority (56%) say that their state should expand Medicaid to cover more low-income adults, while nearly four in 10 (37%) say their state should keep Medicaid as it is today.
Slightly more than half of Republicans living in the 18 non-expansion states (all of which have either Republican governors, Republican-controlled legislatures or both) say their state should keep Medicaid as it is today (54%) while four in 10 (39%) say their state should expand their Medicaid program.
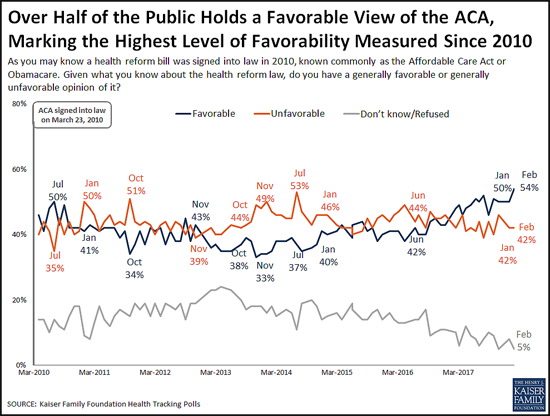
Favorable Views of the ACA Reach New High in More Than 80 KFF Polls
The poll finds 54 percent of the public now holds a favorable view of the Affordable Care Act, the highest share recorded in more than 80 KFF polls since the law’s enactment in 2010. This reflects a slight increase in favorable views since January (50%), while unfavorable views held steady at 42 percent.
The shift toward more positive views comes primarily from independents (55% view the ACA favorably this month, up slightly from 48% in January).
Public Remains Confused about Repeal of the ACA’s Individual Mandate
The poll also probes the public’s awareness about the repeal of the ACA’s requirement that nearly all Americans have health insurance or pay a fine, commonly known as the individual mandate. The tax legislation enacted in December 2017 eliminated this requirement beginning in 2019.
About four in 10 people (41%) are aware that Congress repealed the individual mandate, a slight increase from January, when 36 percent were aware of the provision’s repeal.
However, misunderstandings persist. Most (61%) of the public is either unaware that the requirement has been repealed (40%) or is aware of its repeal but mistakenly believes the requirement will not be in effect during 2018 (21%). Few (13%) are both aware that it has been repealed and that it remains in effect for this year.
Costs are Voters’ Top Health Care Concern ahead of the 2018 Midterm Elections
Looking ahead to this year’s midterm elections, the poll finds Democratic, Republican and independent voters most often cite costs as the health care issue that they most want candidates to address.
When asked to say in their own words what health care issue that they most want candidates to discuss, more than twice as many voters mention health care costs (22%) as any other issue, including repealing or opposing the Affordable Care Act (7%). Costs are the clear top issue for Democrats (16%) and independents (25%), and one of the top issues for Republicans (22%) followed by repealing or opposing the ACA (17%).
Designed and analyzed by public opinion researchers at the Kaiser Family Foundation, the poll was conducted from February 15-20, 2018 among a nationally representative random digit dial telephone sample of 1,193 adults. Interviews were conducted in English and Spanish by landline (422) and cell phone (771). The margin of sampling error is plus or minus 3 percentage points for the full sample. For results based on subgroups, the margin of sampling error may be higher.
Read the article.
Source: Kaiser Family Foundation (1 March 2018). "Poll: Public Mixed on Whether Medicaid Work Requirements Are More to Cut Spending or to Lift People Up; Most Do Not Support Lifetime Limits on Benefits" [Web Poll Post]. Retrieved from address https://www.kff.org/medicaid/press-release/poll-public-mixed-medicaid-work-requirements-more-to-cut-spending-lift-people-up-most-do-not-support-lifetime-limits/
While Talk About Opioids Continues In D.C., Addiction Treatment Is In Peril In States
How is Washington handling the opioid crisis? Let's find out in this article from Kaiser Health News.
Opioids were on the White House agenda Thursday — President Trump convened a summit with members of his administration about the crisis. And Congress authorized funds for the opioid crisis in its recent budget deal — but those dollars aren’t flowing yet, and states say they are struggling to meet the need for treatment.
The Oklahoma agency in charge of substance abuse has been told by the state’s legislature to cut more than $2 million from this fiscal year’s budget.
“Treatment dollars are scarce,” said Randy Tate, president of the Oklahoma Behavioral Health Association, which represents addiction treatment providers.
It’s like dominoes, Tate said. When you cut funding for treatment, other safety-net programs feel the strain.
“Any cuts to our overall contract,” he said, “really diminish our ability to provide the case management necessary to advocate for homes, food, shelter, clothing, primary health care and all the other things that someone needs to really be successful at tackling their addiction.”
In just three years, Oklahoma’s agency in charge of funding opioid treatment has seen more than $27 million dollars chipped away from its budget — thanks to legislative gridlock, slashed state taxes and a drop in oil prices (with the additional loss in state tax revenue that resulted).
Jeff Dismukes, a spokesman for Oklahoma’s Department of Mental Health and Substance Abuse Services, says the already lean agency has few cost-cutting options left.
“We always cut first to administration,” he said, “but there’s a point where you just can’t cut anymore.”
The agency may end up putting off payments to treatment providers until July — the next fiscal year. Tate says that could be devastating.
“Very thinly financed, small rural providers are probably at risk of going out of business entirely — up to and including rural hospitals,” he said.
Getting treatment providers to open up shop in rural areas is really hard, even in good times, and more financial uncertainty could make that problem worse. In the meantime, according to an Oklahoma state commission’s opioid report, just 10 percent of Oklahomans who need addiction treatment are getting it.
That statistic is similar in Colorado. And as 2018 began, Colorado’s escalating opioid crisis got worse, when the state’s largest drug and alcohol treatment provider, Arapahoe House, shut its doors.
The facility provided recovery treatment to 5,000 people a year. Denise Vincioni, who directs another treatment center, the Denver Recovery Group, says other facilities have scrambled to pick up the patients.
Most of Arapahoe’s clients were on Medicaid. Autumn Haggard-Wolfe, a two-time Arapahoe House client who is now in recovery, worries the facility’s closing will have dire consequences, especially for people who need inpatient care, as she did.
“I feel like the only other option right now in therapy would be jail for people,” she said, “and people die in there from withdrawing.”
Arapahoe House’s CEO blamed its closure on the high cost of care and poor government reimbursement for services.
The mother of Colorado state lawmaker Brittany Pettersen struggled with addiction, and was treated at Arapahoe House. Pettersen says treatment centers rely on a crazy quilt of funding sources and are chronically underfunded — often leaving people with no treatment options.
“We have a huge gap in Colorado,” Pettersen said, “and that was before Arapahoe House closed.”
She is pushing legislation in the state to increase funding for treatment. But to get tens of millions of dollars in federal matching funds, Colorado lawmakers need to approve at least $34 million a year in new state spending.
That price tag may simply be too high for some lawmakers. But either way, she added, “It’s going to take a lot to climb out of where we are.”
Colorado did get new federal funds to fight the opioid crisis through the 21st Century Cures Act, passed in December of 2016, but it was just $7.8 million a year for two years — divvied up among a long list of programs.
Read the article.
Source: Daley J.,Fortier J. (5 March 2018). "While Talk About Opioids Continues In D.C., Addiction Treatment Is In Peril In States" [Web Blog Post]. Retrieved from address https://khn.org/news/while-talk-about-opioids-continues-in-dc-addiction-treatment-is-in-peril-in-states/
How Are Health Centers Responding to the Funding Delay?
Unfortunately, the funding delay is impacting healthcare centers everywhere - and not in a great way. Get the information you need to know in this article.
Health centers play an important role in our health care system, providing comprehensive primary care services as well as dental, mental health, and addiction treatment services to over 25 million patients in medically underserved rural and urban areas throughout the country. Health care anchors in their communities and on the front lines of health care crises, including the opioid epidemic and the current flu outbreak, health centers rely on federal grant funds to support the care they provide, particularly to patients who lack insurance coverage. However, the Community Health Center Fund (CHCF), a key source of funding for community health centers, expired on September 30, 2017, and has since been extended through only March 31, 2018. The CHCF provides 70% of grant funding to health centers. With these funds at risk, health centers have taken or are considering taking a number of actions that will affect their capacity to provide care to their patients. This fact sheet presents preliminary findings on how health centers are responding to the funding uncertainty.
WHAT FUNDING IS AT STAKE FOR HEALTH CENTERS
The Community Health Center Fund represents 70% of federal grant funding for health centers. Established by the Affordable Care Act, the CHCF increased federal grant fund support for health centers, growing from $1 billion in 2011 to $3.6 billion in 2017.1Authorized for five years beginning in 2010, and extended for two years through September 2017, the CHCF also provided a more stable source of grant funding for health centers that was separate from the annual appropriations process. Prior to the CHCF, federal 330 grant funds were appropriated annually. In fiscal year 2017, federal section 330 grant funding totaled $5.1 billion, $3.6 billion from the CHCF and $1.5 billion from the annual appropriation.
Federal health center grants represent nearly one-fifth of health center revenues. Federal Section 330 grant funds are the second largest source of revenues for health centers behind revenues from Medicaid. Overall, 19% of health center revenues (including US territories) come from federal grants; however, reliance on 330 grant funds varies across health centers. Federal grant funds are especially important for health centers in southern and rural non-expansion states where Medicaid accounts for a smaller share of revenue (Figure 1).2 These funds finance care for uninsured patients and support vital services, such as transportation and case management, that are not typically covered by insurance
HOW ARE HEALTH CENTERS RESPONDING TO THE LOSS OF FEDERAL FUNDS?
Health centers have taken or are considering taking a number of actions that will affect their ability to serve their patients. Overall, seven in ten responding health centers indicated they had taken or planned to take action to put off large expenditures or curtail expenses in face of reduced revenue. Some of these actions involve delaying or canceling capital projects and other investments or tapping into reserve funds. Other actions, however, have or will reduce the number of staff or the hours they work, which may in turn, affect the availability of services. Already 20% of health centers reported instituting a hiring freeze and 4% have laid off staff. Another 45% are considering a hiring freeze and 53% said they might lay off staff. While health centers seemed to focus on shorter-term actions that could easily be reversed were funding to be restored, 3% of responding health centers had already taken steps to close one or more sites and an additional 36% indicated they are considering doing so (Figure 2).
Health centers are considering cuts to patient services. While most health centers have not yet taken steps to cut or reduce patient care services, many reported they are weighing such actions if funding is not restored (Figure 3). Over four in ten indicated they might eliminate or reduce some enabling services, such as case management, translation, or transportation services. Additionally, over a third of reporting health centers indicated they might have to reduce the dental, medical, and/or mental health services they provide while 29% said cuts to addiction treatment services are being contemplated. Fewer health centers reported that cuts to pharmacy services might be made.

Figure 3: Services Health Centers Are Considering Eliminating or Reducing in Response to Funding Uncertainty
WHAT ARE THE IMPLICATIONS OF THE FUNDING DELAY?
Continued delays in restoring funding will likely lead to cuts in health center services and staff. To date, health centers have tried to mitigate the effects of the funding delay by forgoing major investments or dipping into reserve funds. However, the longer the funding delay continues, the greater the likelihood health centers will be compelled to cut services and staff, actions they are currently considering but have not yet adopted in large numbers. These cuts could reverse gains health centers have made in recent years in increasing patient care capacity and expanding the range of services they provide, particularly in the areas of mental health and addiction treatment. Health centers play a particularly important role in rural and medically underserved areas. The failure to reauthorize the CHCF and restore health center funding could jeopardize access to care for millions of vulnerable patients.
SOURCE: Kaiser Family Foundation (1 February 2018). "How Are Health Centers Responding to the Funding Delay?" [Web Blog Post]. Retrieved from address https://www.kff.org/medicaid/fact-sheet/how-are-health-centers-responding-to-the-funding-delay/
SaveSave
Understanding the Intersection of Medicaid and Work
Sometimes, healthcare is confusing. We know this, which is why today we are focusing on Medicaid and work. Check out the snippet below, and check out the link for the full article.
Medicaid is the nation’s public health insurance program for people with low incomes. Overall, the Medicaid program covers one in five Americans, including many with complex and costly needs for care. Historically, nonelderly adults without disabilities accounted for a small share of Medicaid enrollees; however, the Affordable Care Act (ACA) expanded coverage to nonelderly adults with income up to 138% FPL, or $16,642 per year for an individual in 2017. As of December 2017, 32 states have implemented the ACA Medicaid expansion.1 By design, the expansion extended coverage to the working poor (both parents and childless adults), most of whom do not otherwise have access to affordable coverage. While many have gained coverage under the expansion, the majority of Medicaid enrollees are still the “traditional” populations of children, people with disabilities, and the elderly.
Some states and the Trump administration have stated that the ACA Medicaid expansion targets “able-bodied” adults and seek to make Medicaid eligibility contingent on work. Under current law, states cannot impose a work requirement as a condition of Medicaid eligibility, but some states are seeking waiver authority to do so. These types of waiver requests were denied by the Obama administration, but the Trump administration has indicated a willingness to approve such waivers. This issue brief provides data on the work status of the nearly 25 million non-elderly adults without SSI enrolled in Medicaid (referred to as “Medicaid adults” throughout this brief) to understand the potential implications of work requirement proposals in Medicaid. Key takeaways include the following:
- Among Medicaid adults (including parents and childless adults — the group targeted by the Medicaid expansion), nearly 8 in 10 live in working families, and a majority are working themselves. Nearly half of working Medicaid enrollees are employed by small firms, and many work in industries with low employer-sponsored insurance offer rates.
- Among the adult Medicaid enrollees who were not working, most report major impediments to their ability to work including illness or disability or care-giving responsibilities.
- While proponents of work requirements say such provisions aim to promote work for those who are not working, these policies could have negative implications on many who are working or exempt from the requirements. For example, coverage for working or exempt enrollees may be at risk if enrollees face administrative obstacles in verifying their work status or documenting an exemption.
Get the full report and findings.
SOURCE: Kaiser Family Foundation (5 January 2018). "Understanding the Intersection of Medicaid and Work" [Web Blog Post]. Retrieved from address https://www.kff.org/medicaid/issue-brief/understanding-the-intersection-of-medicaid-and-work/
CenterStage: February is American Heart Month - Are Your Loved Ones Knowledgeable?
Heart disease is the leading cause of death for men and women in the United States. Every year, 1 in 4 deaths are caused by heart disease, according to the American Heart Association.
Talking with your loved ones about heart disease can be awkward, but it’s important. In fact, it could save a life. At the dinner table, in the car, or even via text, have a heart-to-heart with your loved ones about improving heart health as a family. Engaging those you care about in conversations about heart disease prevention can result in heart-healthy behavior changes.

Here are three reasons to talk to the people in your life about heart health and three ways to get the conversation started.
Three Reasons You Should Talk to Your Loved Ones About Heart Health
#1. More than physical health is at risk

Millions of people in the US don’t know that they have high blood pressure. High blood pressure raises the risk for heart attacks, stroke, heart disease, kidney disease and many other health issues. Researchers are learning that having high blood pressure in your late 40s or early 50s can lead to dementia later in life. Encourage family members to be aware of blood pressure levels and monitor them consistently.
#2. Feel Younger Longer

Just as bad living habits can age you prematurely and shorten your lifespan, practicing good heart healthy habits can help you feel younger longer. On average, U.S. adults have hearts that are 7 years older than they should be, according to the Center for Disease Control and Prevention. Just beginning the conversation with the people in your life that you care about can begin to make changes in their heart health.
#3. You Are What You Eat

Even small changes can make a big difference. Prepare healthier versions of your favorite family recipes by making simple ingredient swaps, simply searching the internet is all it usually takes to find an easy ingredient alternative. Find a new
recipe to cook for your family members, or get in the kitchen together and you’ll finish with something delicious and possibly making some new favorite memories as well. When grocery shopping, choose items low in sodium, added sugar, and trans fats, and be sure to stock up on fresh fruits and vegetables.
Three Ways to Start the Conversation
- Encourage family members to make small changes, like using spices to season food instead of salt.
- Motivate your loved ones to incorporate physical activity into every day. Consider a family fitness challenge and compete with each other to see who can achieve the best results.
- Avoid bad habits together. It has been found that smokers are twice as likely to quit if they have a support system. This applies to practicing healthier practices as well. Set goals and start by making small, positive changes, chances are they may have a big difference.
The key to heart health is a healthy lifestyle. It’s important to try to let go of bad habits that increase your risk of heart disease. By setting small, achievable goals and tracking those goals, you can possibly extend your life expectancy a little bit each day.
Heart disease can be prevented by making healthy choices and consciously monitoring health conditions. Making healthy choices a topic of conversation with your family and loved ones is a great way to open the door to healthier practices in all walks of life.
Download the PDF
SaveSaveSaveSaveSaveSave
Health Care Lags As Hot-Button Issue
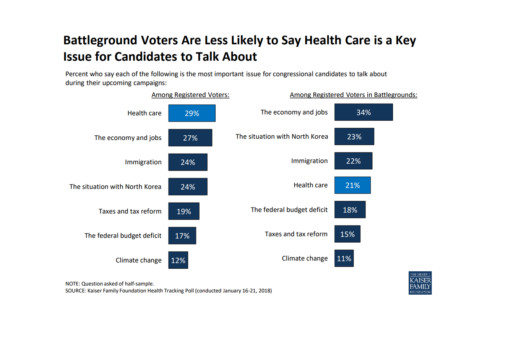
As it turns out - according to this poll conducted by Kaiser Health News - health care is not a key issue battleground voters wish to discuss. Instead, a large number of voters are more interested in dealing with issues regarding our economy and jobs.
Read further in this article below.
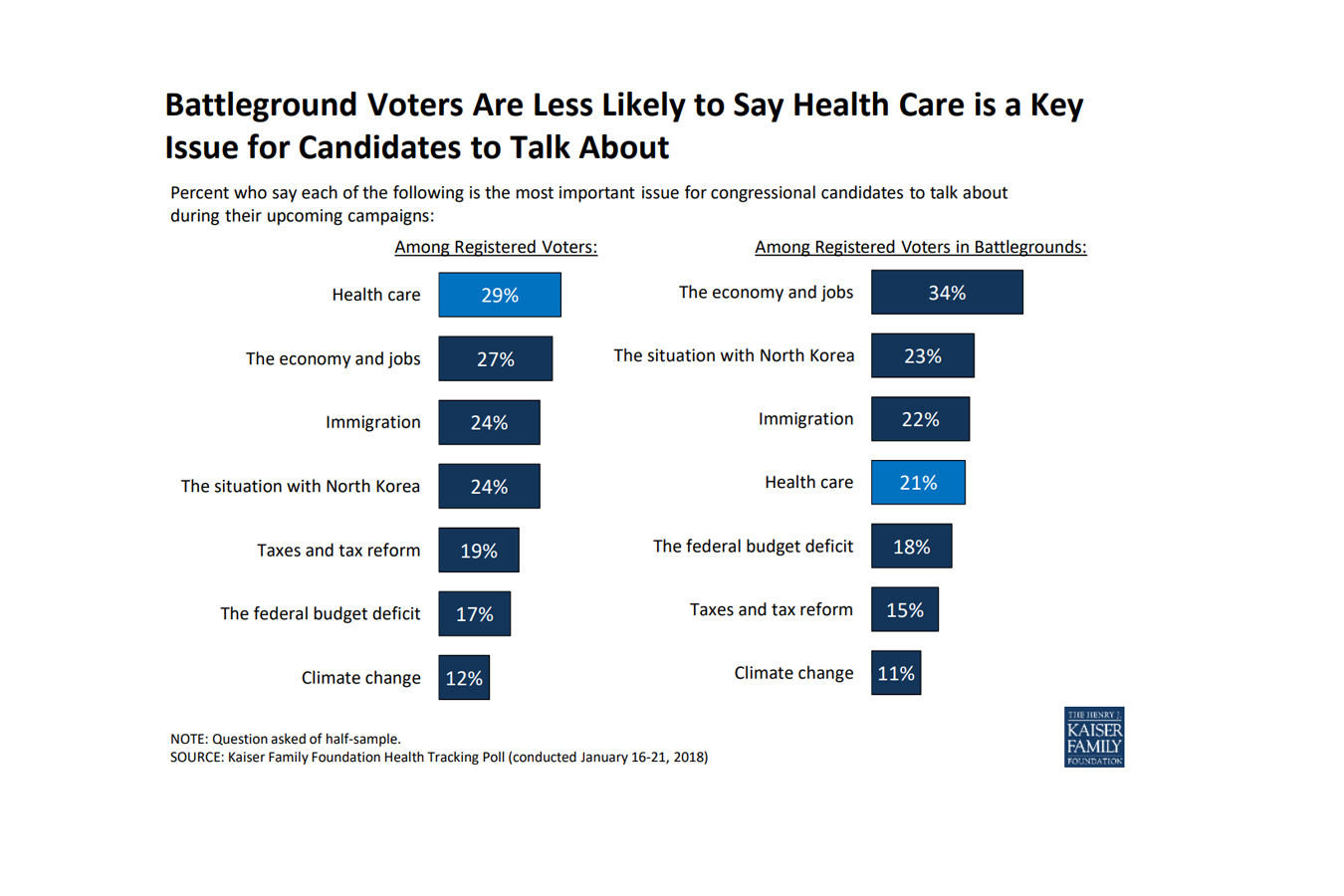 As the midterm elections approach, health care ranks as the top issue, mentioned more frequently among voters nationwide than among those living in areas with competitive races, a new poll finds.
As the midterm elections approach, health care ranks as the top issue, mentioned more frequently among voters nationwide than among those living in areas with competitive races, a new poll finds.
In areas with competitive congressional or gubernatorial races, the economy and jobs ranked as the top issue for candidates to discuss, with 34 percent of registered voters listing it as No. 1, according to the poll from the Kaiser Family Foundation. (Kaiser Health News is an editorially independent program of the foundation.) Following economics was the conflict with North Korea (23 percent), immigration (22 percent) and health care (21 percent). The competitive areas are 13 states with statewide races and 19 House districts judged as toss-ups by the nonpartisan Cook Political Report.
Nationwide, 29 percent of registered voters ranked health care as the most important issue for electoral discussion — though it was far more important for Democrats than Republicans. Economy and jobs were close behind with 27 percent of voters rating it most important, and then immigration, with 24 percent listing it.
The poll found that nearly half of Americans believed there is still a federal requirement for everyone to obtain health insurance, even though Congress’ tax bill last year repealed the penalties for that requirement in the Affordable Care Act, known as the individual mandate. Only a third of the public was sure that those penalties had been repealed.
Fifty percent of the public expressed a favorable view of the health law, while 42 percent disliked it. Six in 10 people said that since President Donald Trump and the Republicans in Congress have altered the law, they are responsible for any problems. Like other opinions about the law, there was a strong partisan split: Only 38 percent of Republicans thought their party is now responsible, while 77 percent of Democrats thought so. Half of Republicans still listed repealing the health law as a top priority.
There was less of a partisan split over the importance that the president and Congress address the epidemic of prescription painkiller addiction. Among Republicans, 43 percent rated it a top priority; 54 percent of Democrats agreed.
There was no such comity over whether lawmakers should allow people brought illegally to this country by their parents — the so-called Dreamers — to stay in the country legally: 21 percent of Republicans called that a top priority, while 66 percent of Democrats did. And while 43 percent of Republicans said they wanted lawmakers to focus on passing federal funding for a border wall with Mexico, only 5 percent of Democrats and 19 percent of independents did.
The poll was conducted Jan. 16-21 among 1,215 adults. The margin of error was +/-3 percentage points. The poll included 298 people who said they were registered to vote in one of the areas the Cook Report identified as a battleground in the fall elections. The margin of error for results for this group was +/-7 percentage points.
Read the original article.
Source: Rau J. (26 January 2018). "In Battleground Races, Health Care Lags As Hot-Button Issue, Poll Finds" [Web Blog Post]. Retrieved from address https://khn.org/news/in-battleground-races-health-care-lags-as-hot-button-issue-poll-finds/
Tax Bill Provision Designed To Spur Paid Family Leave To Lower-Wage Workers

Tucked into the new tax law is a provision that offers companies a tax credit if they provide paid family and medical leave for lower-wage workers.
Many people support a national strategy for paid parental and family leave, especially for workers who are not in management and are less likely to get that benefit on the job. But consultants, scholars and consumer advocates alike say the new tax credit will encourage few companies to take the plunge.
The tax credit, proposed by Sen. Deb Fischer (R-Neb.), is available to companies that offer at least two weeks of paid family or medical leave annually to workers, but two key criteria must be met. The workers must earn less than $72,000 a year and the leave must cover at least 50 percent of their wages.
If contributing at the half-wage level, a company receives a tax credit equal to 12.5 percent of the amount it pays to the worker. The tax credit will increase on a sliding scale if the company pays more than 50 percent of wages. It could go up to a maximum credit of 25 percent of the amount the employer paid for up to 12 weeks of leave.
Payments to full- and part-time workers taking family leave who’ve been employed for at least a year would be eligible for the employer’s tax break. But the program, which is designed to test whether this approach works well, is set to last just two years, ending after 2019.
Aparna Mathur, a resident scholar in economic policy studies at the American Enterprise Institute, says the new tax credit sidesteps a pitfall for Republicans. They are wary of any legislation mandating that employers provide paid leave. The tax credit also is appropriately aimed at lower-wage workers who are most likely to lack access to paid leave, said Mathur, who co-authored a recent report on paid family leave.
But it’s not a big enticement.
“Providing this benefit is a huge cost for employers,” Mathur said. “It’s unlikely that any new companies will jump on board just because they have a 12.5 to 25 percent offset.”
That view is shared by Vicki Shabo, vice president for workplace policies and strategies at the National Partnership for Women & Families, an advocacy group, who said it will primarily benefit workers at companies already offering paid family leave. The new tax credit “just perpetuates the boss lottery,” she added.
Heather Whaling said her 22-person public relations company probably qualifies for the new tax credit, but she doesn’t think it’s the right approach. Whaling, the president of Geben Communication in Columbus, Ohio, already offers paid leave. The company provides up to 10 weeks of paid leave at full pay for new parents. Four employees have taken leave, and by divvying up their work to other team members and hiring freelancers they’ve been able to get by.
“It is an expense, but if you plan and budget carefully it’s not cost-prohibitive,” she said.
The tax credit isn’t big enough to provide a strong incentive to provide paid leave, said Whaling, 37. Besides, “having access to paid family leave shouldn’t be luck of the draw, it should be available to every employee in the country.”
Still, the tax credit may be appealing to companies that have been considering adding a paid family and medical leave benefit, said Rich Fuerstenberg, a senior partner at benefits consultant Mercer.
By defraying some of the cost, the tax credit could help “tip them over” into offering paid leave, he said. But “I’m not even sure I’d call it the icing on the cake,” Fuerstenberg said. “It’s like the cherry on the icing.”
Only 15 percent of private-sector and state and local government workers had access to paid family and medical leave in 2017, according to the Bureau of Labor Statistics’ National Compensation Survey. Eighty-eight percent had access to unpaid leave, however.
Under the federal Family and Medical Leave Act, employers with 50 or more workers generally must allow eligible employees to take unpaid leave for up to 12 weeks annually for specified reasons. These include the birth or adoption of a child, caring for your own or a family member’s serious health condition, or leave for military caregiving or deployment. An individual’s job is protected during such leaves.
A tax credit that can be claimed at the end of the year is unlikely to encourage small businesses to offer paid family and medical leave, said Erik Rettig, an expert on family leave policies at the Small Business Majority, which advocates for those firms on national policy.
“It isn’t going to help the family business that has to absorb the costs of this employee while they’re gone,” Rettig said.
A better solution, according to Shabo and others, is to provide a paid family leave benefit that’s funded by employer and/or employee payroll contributions. Sen. Kirsten Gillibrand (D-N.Y.) and Rep. Rosa DeLauro (D-Conn.) last year reintroduced such legislation. Their bill would guarantee workers, including those who are self-employed, up to 12 weeks of family and medical leave with as much as two-thirds of their pay.
A handful of mostly Democratic states — including California, New Jersey, Rhode Island and New York — have similar laws in place, and a program in the District of Columbia and Washington state will begin in 2020.
“We know from states that this approach works for both employees and their bosses,” Shabo said.
Read the original article.
Source: Andrews M. (23 January 2018). "Tax Bill Provision Designed To Spur Paid Family Leave To Lower-Wage Workers" [Web blog post]. Retrieved from address https://khn.org/news/tax-bill-provision-designed-to-spur-paid-family-leave-to-lower-wage-workers/
SaveSave