Two Months After Hurricane Maria, A Growing Majority Of Americans Say Puerto Ricans are Not Yet Getting the Help They Need
Two months after Hurricane Maria struck Puerto Rico, a growing majority of Americans say that Puerto Ricans affected by the devastating storm are not yet getting the help they need, the November Kaiser Family Foundation Tracking Poll finds.
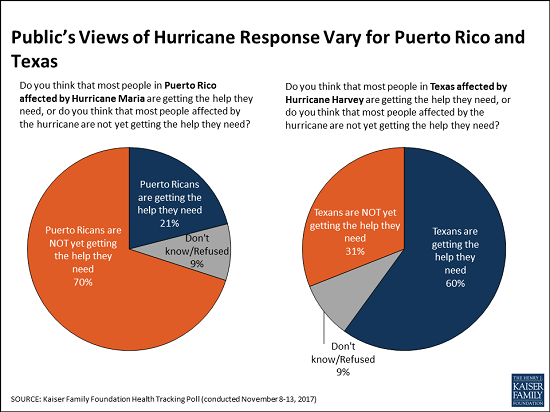
This month, 70 percent of the public say that people in Puerto Rico are not yet getting the help they need, up from 62 percent in October 2017. These perceptions vary by party, and half of Republicans (52%) now say Puerto Ricans aren’t yet getting needed help, up significantly from October (38%).
When asked whether the federal government is doing enough to restore electricity and access to food and water in Puerto Rico or not, a majority of the public (59%) says the federal government is not doing enough, up from 52 percent in October. Most Democrats (86%) and independents (59%) say the federal government is not doing enough, but most Republicans (63%) say it is doing enough.
In contrast, Americans see the recovery efforts in Texas following Hurricane Harvey in late August progressing more positively. Most (60%) of the public says Texans are getting the help they need, twice the share (31%) who say Texans aren’t yet getting needed help.
The poll finds similar shares of Americans they are closely following news about recovery efforts in Puerto Rico (63%) and in Texas (58%). Democrats are somewhat more likely to report closely following news about the Puerto Rico recovery (75%) than are independents (61%) and Republicans (54%). In contrast, there are no partisan differences for those following news about Texas.
Designed and analyzed by public opinion researchers at the Kaiser Family Foundation, the poll was conducted from November 8 – 13, 2017 among a nationally representative random digit dial telephone sample of 1,201 adults. Interviews were conducted in English and Spanish by landline (415) and cell phone (786). The margin of sampling error is plus or minus 3 percentage points for the full sample. For results based on subgroups, the margin of sampling error may be higher.
You can read the original article here.
Source:
Kaiser Family Foundation (20 November 2017). "Two Months After Hurricane Maria, A Growing Majority Of Americans Say Puerto Ricans are Not Yet Getting the Help They Need" [Web blog post]. Retrieved from address https://www.kff.org/other/press-release/poll-two-months-after-hurricane-maria-a-growing-majority-of-americans-say-puerto-ricans-are-not-ye-getting-the-help-they-need/
SaveSave
Is Social Media Putting Employees’ Health, Safety at Risk?
Do your employees know about all of the risks that can come from their social media? Find out how social media can affect your employee's safety and health in this article from Employee Benefit News by Jill Hazan.
The issue of personal online safety has finally crossed over into the healthcare arena — and employers need to step up and learn to best educate employees about keeping them safe.
A recent article in the Journal of the American Medical Association Pediatrics, “Parental Sharing on the Internet: Child Privacy in the Age of Social Media and the Pediatrician’s Role,” highlights how parents who post information about their children on social media put them at greater risk for identity theft. In addition, this trend toward oversharing compromises a child’s protected health information. What might happen when that child applies for a job in the future and a simple internet search reveals health information she would not want an employer to know?
While HIPAA protects the confidentiality of an individual’s medical records, it doesn’t provide comprehensive protections outside the healthcare environment. The laws around the privacy rights of children relative to their parents’ online disclosures are still evolving. The article recommends that pediatricians ask parents about their social media habits to help keep children safe and their data private. It is a natural extension that all primary care providers should be asking patients about social media behaviors, as the issues of identity theft and data privacy are relevant to children and adults alike.
This recommendation is increasingly significant from an employee benefit perspective.
So what should employers do?
Employers routinely provide healthcare benefits to employees. If health plans and physicians are acknowledging and addressing the risks of social media from a privacy and security perspective, shouldn’t employers extend that focus into the workplace? With the continued employer emphasis on wellness, it is incumbent on health plans and employers alike to educate employees on online security and the risks of identity theft.
There are a variety of resources and benefits that employers can access to assist employees in navigating the online world safely. A series of well-structured, engaging seminars on identity theft and online security that combine real-life stories with actionable advice are effective in educating employees and changing behaviors. Online tutorials, like those provided by the Center for Identity at the University of Texas, Austin, can guide employees on setting proper privacy settings on social media sites, such as Facebook, Twitter, LinkedIn and Pinterest.
Identity theft protection plans provide monitoring and restoration services, as well as education to help keep employees and their families secure. EAPs may provide guidance on identity theft and counseling for victims. Comprehensive legal benefit plans provide legal advice and representation for victims of identity theft. Employers may also provide employees access to online data protection tools for use at work and home with features that encrypt communication and block malware and phishing attempts.
Employees need to understand how to navigate the social media and online environment to keep their families safe. Identity theft of a family member affects more than just one person. It can register an emotional, physical and financial toll on the entire family. Employers need to structure a comprehensive approach to managing the health and wellness of employees as it relates to their online behaviors. A program with a combination of employee benefits, from healthcare to identity theft protection benefits, supplemented by onsite employee education, will support the goals of the health plan and, ultimately, the organization’s overall business objectives.
See the original article Here.
Source:
Hazan J. (2017 May 1). Is social media putting employees' health, safety at risk? [Web blog post]. Retrieved from address https://www.benefitnews.com/opinion/is-social-media-putting-employees-health-safety-at-risk?feed=00000152-18a4-d58e-ad5a-99fc032b0000
Photo Credit: HowToStartABlogOnline.net
Big “I” Applauds Senate Passage Of Flood Insurance Legislation
Originally posted March 19, 2014 on https://www.insurancebroadcasting.com
WASHINGTON, D.C., March 13, 2014 — The Big “I” applauds the U.S. Senate for passing H.R. 3370, the “Homeowner Flood Insurance Affordability Act of 2013,” by Sen. Bob Menendez (D-N.J.) and Rep. Michael Grimm (R-N.Y.).
The bipartisan bill would make changes to the Biggert-Waters Act of 2012 (Biggert-Waters) in order to help with the “sticker shock” some consumers are facing as a result of two provisions that create drastic premium increases in many parts of the country. The House passed H.R. 3370 on March 4, 2014 in a 306 – 91 vote.
“The Big ‘I’ would like to particularly commend Senators Menendez and Isakson and Representatives Grimm and Waters for their tireless work on fixing some of the unintended effects of Biggert-Waters,” says Robert Rusbuldt, Big “I” president & CEO. “This bill was a top priority for the Big ‘I’ as it will reduce some of the harmful effects of Biggert-Waters without undoing the numerous positive provisions within the law.”
In addition to other revisions to Biggert-Waters, the bill would repeal the entirety of Section 207 and would therefore reinstate the “grandfathering” of policies located in communities with a new or redrawn map. H.R. 3370 would also stop the elimination of subsidies for pre-FIRM properties that are bought and sold, which is an extremely problematic provision in Section 205 of Biggert-Waters.
“Today’s Senate vote represents a major victory for independent insurance agents, as Section 207 and the bought/sold provision of Section 205 were the two specific items that the Big ‘I’ has been asking Congress to revisit,” says Charles Symington, Big “I” senior vice president for external and government affairs. “The startling pace with which Congress acted in order to fix the unintended effects of these two provisions in Biggert-Waters, itself less than two years old, should be commended.”
Founded in 1896, the Big “I” is the nation’s oldest and largest national association of independent insurance agents and brokers, representing a network of more than a quarter of a million agents, brokers and their employees nationally. Its members are businesses that offer customers a choice of policies from a variety of insurance companies. Independent agents and brokers offer all lines of insurance—property, casualty, life, health, employee benefit plans and retirement products. Web address: www.independentagent.com.
High-level executives often do not understand company risks
Originally posted July 25, 2013 by Rodd Zolkos on https://www.businessinsurance.com
A new report from Forbes Insights sponsored by Zurich Insurance Group Ltd. suggests that many executives don't understand their companies' exposure to risks or their strategies to manage them.
The survey of 414 U.S. executives in the banking and financial services, real estate, health care and construction industries found that 28% indicated their company had suffered financial damage as a result of operational risk, 27% because of regulatory or compliance risk and 26% as a result of financial risk.
But when asked about the top barriers to effective risk management, 36% of executives in banking and financial services and 29% of those in real estate cited a lack of understanding of how to mitigate exposures as the top barrier. Among construction executives, 43% cited a lack of understanding of the sources of risk as the top barrier, while insufficient risk management budget was cited as the top barrier by 33% of health care executives.
A lack of understanding of how to mitigate risks was the second-greatest barrier cited by construction executives, at 27%, and health care executives, at 30%.
However, large percentages of executives in each industry category indicated they would manage risk no differently in the next three years: 41% of banking and financial services executives, 50% of construction executives, 42% of health care executives and 47% of real estate executives.
Of the total group, 76% of executives rated the need to align risk management with their company's growth strategy as very or extremely important, and 68% said they thought their company was doing so. But only 54% said they were confident or very confident of how aware they were of the risks associated with their company's growth strategies.
The report, “The Sharp Side of Risk: Understanding, Anticipating and Managing Business Risk,” is available here.
New OSHA code employers should know
Original article https://eba.benefitnews.com
By Martha J. Zackin
A spike in reports of temporary workers suffering fatal injuries on the job has spurred a new initiative to protect them. On April 29, the U.S. Department of Labor's Occupational Safety and Health Administration announced an initiative to protect temporary employees from workplace hazards. The initiative, announced through a press release and a memorandum sent to all of OSHA’s regional administrators, directs field inspectors to assess whether employers who use temporary workers are complying with their responsibilities under the OSH Act.
Inspectors will use a newly created code in their information system to denote when temporary workers are exposed to safety and health violations. Additionally, they will assess whether temporary workers received required training in a language and vocabulary they understand.
In many cases of recent injuries of temporary workers, OSHA reports, the employer failed to provide safety training or, if some instruction was given, it inadequately addressed the hazard, and this failure contributed to their death.
OSHA field inspectors are now directed to determine, within the scope of their inspections, whether any employees are temporary workers and whether any of the identified temporary employees are exposed to a volatile condition. In addition, inspectors are directed to assess — using both records review and interviews — whether those workers have received required training in a language and vocabulary they understand. A new OIS code has been established to identify temporary workers. In addition, field inspectors are directed to identify the workers’ staffing company, the company’s location, and the supervising structure under which the temporary workers are reporting (i.e., the extent to which the temporary workers are being supervised on a day-to-day basis either by the staffing client or the staffing agency).
OSHA has also begun working with the American Staffing Association and employers that use staffing agencies to promote best practices ensuring that temporary workers are protected from job hazards.
Both staffing firms and companies that use temporary workers are required to provide safe workplaces, as well as necessary safety and health training regarding workplace hazards. Although allocation of safety-related duties and responsibilities should be clearly spelled out in contracts between staffing firms and client companies, both entities may be held liable by OSHA and the courts. Please consult your employment counsel and OSHA consultants for further information and assistance.
Lighting Indoors and Out for Safety, Efficiency, Comfort, and Security
Source: https://safetydailyadvisor.blr.com
Yesterday, we provided tips for improving workplace lighting to boost safety and productivity. Today, we offer some tips from Facebook on indoor lighting as well as advice from DOE on outdoor lighting.
Facebook, which is always a consistent innovator in technology and media, is now leading the way in energy efficiency, says BLR Legal Editor and Green Team member Amanda Czepiel, J.D. According to Naveen Lakshmipathy, a 2011 EDF Climate Corps fellow at Facebook, the company’s new 1 million square foot office campus can teach other companies three lessons in energy efficiency.
1. Plan ahead. The best way to integrate lighting energy efficiency without losing good design is to involve many people in the design process, from architects to engineers to energy efficiency experts, to ensure that all factors are considered from the start of the design process. For example, walls can be painted in appropriate shades to reflect light where it is best to do so.
2. Know how you want your lighting system to behave. If you want to use lighting controls such as occupancy and daylight sensors to vary light levels and optimize energy efficiency, you must plan ahead of time how you want your system to behave and test its functions.
3. Remember productivity and occupant comfort. There is a direct relationship between workplace comfort and increased productivity, so effectively using daylight to reduce the use of artificial lighting and eliminating overlighted or underlighted areas should be a priority.
Outdoor Lighting
According to the U.S. Department of Energy, effective lighting for safety and security should consider:
Horizontal illuminance. This is the standard for assessing effective lighting primarily because many tasks are horizontal and the measurements are easy to make. However, this is less critical for security than other metrics such as vertical illuminance and uniformity.
Vertical illuminance. This is critical because one of the main security issues is identifying persons and vehicles and their movement that is best done by viewing their vertical surfaces.
Uniformity and shadows. This is important primarily to avoid dark areas where people or objects may be hidden. Uniformity has also been found to be useful in enhancing video camera effectiveness.
Glare. Lighting aimed in the wrong direction can cause glare that can adversely affect the ability of occupants and security personnel to identify people and/or objects.
Furthermore, research shows that simply increasing light levels or maintaining high lighting levels does not necessarily promote or maintain enhanced safety or security. It is primarily factors associated with the placement and quality of exterior lighting that enhances facility and employee safety and security outside your workplace.
Light Up Your Workplace with Safer, Healthier Lighting
Source: https://safetydailyadvisor.blr.com
Light is a force that has a powerful impact on the human body. Studies have shown that dedicated applications of lighting can have an effect on all aspects of a worker's experience, including reduction in accidents, illness, eyestrain, and absenteeism.
Lighting in the average workplace ranges from 50 to 500 lux (a measurement of illumination equal to the intensity of one candle). Research has shown that proper use of lighting can lessen the loss of alertness, production errors, and accidents, especially among nightshift workers and those on rotating shifts.
A 60-watt incandescent bulb in a 10-foot-high ceiling will produce only about 100 lux at eye level. Studies show that carefully timed exposure to bright light (over 1,000 lux) decreases fatigue and increases alertness.
You may want to have your facility manager assess the wattage of lights over workstations, check for burned-out bulbs, and make sure lighting fixtures are dusted and cleaned periodically.
Supplemental lighting with lamps, rather than more overhead lighting, can be added at workstations as needed to adequately illuminate tasks.
Interior Colors
Interior colors, especially in production areas, should be of medium value. Therefore, dark-colored carpeting and flooring, window treatments, walls, and cubicles may not be the best choice. Dark colors also absorb light, thus requiring the use of more wattage—and electricity—to illuminate an area. On the other hand, light or bright colors can contribute to glare and eyestrain.
Surface Reflectants
Make sure that lighting is diffused through baffles or bounced off surfaces in such a way that serious shadows and glare are avoided. Use of matte finishes, rather than glossy or polished surfaces, is also recommended for work areas.
Types of Lighting
- Incandescent. This type of lighting was invented by Thomas Edison and has been used for over 100 years. Modern technology has reduced glare through the development of soft white, reflector, linestra, and other types of bulbs.
- Halogen. This type of bulb is often used in task lighting and track lighting because it saves energy.
- Fluorescent. New energy-saving fluorescent bulbs can be used as direct replacements for incandescent bulbs. They give more realistic color quality and can save as much as 75 percent in energy cost.
- Full-spectrum. These new bulbs simulate the full-spectrum light of natural sunshine. Not only do they reduce eyestrain, but they have the added dimension of improving mood, especially during the shorter days of winter or for night workers. Studies also show that worksites with full-spectrum lighting have half the absenteeism for illness than those that do not.
- Sunlight. It is obvious, but the effective use of natural sunlight to reduce the use of artificial lighting and eliminate overlighted or underlighted areas should be a priority.
Five trends in wellness incentives for 2013
Five trends in wellness incentives for 2013
Employers want return of investment for their wellness programs. They want to know what incentive dollars are really being used for. Here are five trends to look for in wellness incentives in 2013.
1. Personalization of incentives
The idea of incentivizing people to participate in wellness programs is one of the few to be embraced with equal enthusiasm across the board.
While the concept held enough innovation and promise to spur health plans and employers to spend over $60 billion last year to motivate consumers to engage in health, incentives have often been primitive in execution. Incentive dollars flow to plan members as reward or encouragement for healthy behaviors, but what consumers do with that money has until now been largely a mystery to employers and health insurers.
A 2009 survey conducted by MasterCard and Harris Interactive found 61% of employees participate in a wellness program if incentives are offered versus only 26% when there is no added incentive. Additionally, 25% of employees reported that being incentivized was actually the driver and the very reason they agreed to enroll in a wellness program at all.
Instead, the answer is to better tailor the incentives to fit the person, and to provide incentives that motivate while driving program ROI. A recent study from the Journal of Economic Psychology shows consumers prefer to be incentivized with cash. Yet the utility of cash (even cash rebated to a paycheck) leads many to decisions that fail to drive long-term engagement, satisfaction and ultimately outcomes.
2. Incentives tailored around health related products and services
Health incentives need to focus on an emotional affinity felt by participants toward earned rewards—a paradigm that has the potential to create the initial embrace of health behavior change and perpetuate it. Yet, today’s healthcare dollars are stretched thin, and employers want to make sure every dime spent on health and wellness programs is targeted to accomplish health goals. They have increasingly offered discounts to fitness clubs, healthy foods, supplements and Weight Watchers as incentives.
3. New focus on analytics
The Patient Protection and Affordable Care Act (PPACA) increases the cap on wellness incentives—now at 20% of an employee’s total health insurance premium cost—to 30% and then 50% by 2014. This provides an opportunity to create an incentive program with influence.
Yet as increasing dollar amounts are being driven towards wellness/incentive programs; understanding exactly how funds are being spent; what they are being spent on; and how the actual spending is impacting outcomes and ROI will be critical to understanding the overall impact and success of wellness incentive programs. To that end, rich new data sets being driven by innovation in payments technology will play a key role over the next 18 to 24 months in determining how funds can better be allocated within programs to achieve results.
4. Deeper integration of wellness incentives into overall care continuum
Through a richer data set of spend analytics tied back into larger Big Data initiatives focused on efficient healthcare dollar allocation, the role of wellness incentives, their impact on behavioral economics, and ultimately their importance within the overall care continuum will be far better understood. Health plans and employers will increasingly have the ability to design and integrate highly targeted incentive dollar programs to reduce costs, and improve outcomes.
5. Continued focus on gamification
The recent gamification of wellness programs, employee challenges and the role that both competition and fun in wellness program engagement will continue, as these wellness tools have proven successful in driving initial and—in many cases—longer term engagement and results. That said, there will be an increased focus in 2013 on the actual currency being offered as rewards.
According to a March 2012 study by Fidelity and the National Business Group on Health, employers on average are spending a $169 per-employee per-year on wellness platforms. Yet they are spending nearly three times that on the actual incentive, or $460 per-employee per-year. The incentive dollars represent the single greatest investment into wellness programs. Until now, these dollars have been limited in their ability to be tangibly measured and evaluated for their effectiveness. This will be a critical area of change in 2013, and one that will fundamentally shift how actual incentive dollars are perceived and utilized across all aspects of healthcare to drive cost reduction.
IRS Issues Three Proposed Regulations Addressing Open Issues Under PPACA
On Nov. 20, 2012, the Department of Health and Human Services issued three sets of proposed rules that provide some of the needed details on how PPACA will probably unfold. The proposed rules address:
- Wellness programs under PPACA
- Essential health benefits and determining actuarial value
- Health insurance market reforms
The proposed rule largely carries forward the rules that have been in effect since 2006. There still would not be limits on the incentives that may be provided in a program that simply rewards participation, such as a program that pays for flu shots or reimburses the cost of a tobacco cessation program, regardless whether the employee actually quits smoking. Programs that are results-based (which will be called "health-contingent wellness programs") still would need to meet several conditions, including a limit on the size of the available reward or penalty. Beginning in 2014, the maximum reward/penalty would increase to 50 percent for tobacco nonuse/use and to 30 percent for other health-related standards.
The proposed rule confirms that nongrandfathered plans in the exchanges and the small-group market will be required to cover the 10 essential health benefits and provide a benefit expected to pay 60, 70, 80 or 90 percent of expected allowed claims. The proposed rule also says that self-funded plans and those in the large employer market would not need to provide the 10 EHBs; instead, they would need to provide a benefit of at least 60 percent of expected allowed claims and provide coverage for certain core benefits. The proposed rule would consider current year employer contributions to a health savings account (HSA) or a health reimbursement arrangement (HRA) as part of the benefit value calculation.
The proposed rule confirms that nongrandfathered health insurers (whether operating through or outside of an exchange) would be prohibited from denying coverage to someone because of a pre-existing condition or other health factor. The proposed rule also provides that premiums for policies in the exchanges and individual and small-group markets could only vary based upon age, tobacco use, geographic location, and family size and sets out details on how premiums could be calculated.