Health insurance surpass $20,000 per year, hitting a record
According to an annual survey of employers, the cost of family health coverage has now surpassed $20,000, a record high. The survey also revealed that while most employers pay most of the costs of coverage, workers' average contribution for a family plan is now $6,000. Read this blog post from Employee Benefit News to learn more.
The cost of family health coverage in the U.S. now tops $20,000, an annual survey of employers found, a record high that has pushed an increasing number of American workers into plans that cover less or cost more, or force them out of the insurance market entirely.
“It’s as much as buying a basic economy car,” said Drew Altman, chief executive officer of the Kaiser Family Foundation, “but buying it every year.” The nonprofit health research group conducts the yearly survey of coverage that people get through work, the main source of insurance in the U.S. for people under age 65.
While employers pay most of the costs of coverage, according to the survey, workers’ average contribution is now $6,000 for a family plan. That’s just their share of upfront premiums, and doesn’t include co-payments, deductibles and other forms of cost-sharing once they need care.
The seemingly inexorable rise of costs has led to deep frustration with U.S. healthcare, prompting questions about whether a system where coverage is tied to a job can survive. As premiums and deductibles have increased in the last two decades, the percentage of workers covered has slipped as employers dropped coverage and some workers chose not to enroll. Fewer Americans under 65 had employer coverage in 2017 than in 1999, according to a separate Kaiser Family Foundation analysis of federal data. That’s despite the fact that the U.S. economy employed 17 million more people in 2017 than in 1999.
“What we’ve been seeing is a slow, slow kind of drip-drip erosion in employer coverage,” Altman said.
Employees’ costs for healthcare are rising more quickly than wages or overall economy-wide prices, and the working poor have been particularly hard-hit. In firms where more than 35% of employees earn less than $25,000 a year, workers would have to contribute more than $7,000 for a family health plan. It’s an expense that Altman calls “just flat-out not affordable.” Only one-third of employees at such firms are on their employer’s health plans, compared with 63% at higher-wage firms, according to the Kaiser Family Foundation’s data.
The survey is based on responses from more than 2,000 randomly selected employers with at least three workers, including private firms and non-federal public employers.
Deductibles are rising even faster than premiums, meaning that patients are on the hook for more of their medical costs upfront. For a single person, the average deductible in 2019 was $1,396, up from $533 in 2009. A typical household with employer health coverage spends about $800 a year in out-of-pocket costs, not counting premiums, according to research from the Commonwealth Fund. At the high end of the range, those costs can top $5,000 a year.
While raising deductibles can moderate premiums, it also increases costs for people with an illness or who gets hurt. “Cost-sharing is a tax on the sick,” said Mark Fendrick, director of the Center for Value-Based Insurance Design at the University of Michigan.
Under the Affordable Care Act, insurance plans must cover certain preventive services such as immunizations and annual wellness visits without patient cost-sharing. But patients still have to pay out-of-pocket for other essential care, such as medication for chronic conditions like diabetes or high blood pressure, until they meet their deductibles.
Many Americans aren’t prepared for the risks that deductibles transfer to patients. Almost 40% of adults can’t pay an unexpected $400 expense without borrowing or selling an asset, according to a Federal Reserve survey from May.
That’s a problem, Fendrick said. “My patient should not have to have a bake sale to afford her insulin,” he said.
After years of pushing healthcare costs onto workers, some employers are pressing pause. Delta Air Lines Inc. recently froze employees’ contributions to premiums for two years, Chief Executive Officer Ed Bastian said in an interview at Bloomberg’s headquarters in New York last week.
“We said we’re not going to raise them. We're going to absorb the cost because we need to make certain people know that their benefits structure is real important,” Bastian said. He said the company’s healthcare costs are growing by double-digits. The Atlanta-based company has more than 80,000 employees around the globe.
Some large employers have reversed course on asking workers to take on more costs, according to a separate survey from the National Business Group on Health. In 2020, fewer companies will limit employees to so-called “consumer-directed health plans,” which pair high-deductible coverage with savings accounts for medical spending funded by workers and employers, according to the survey. That will be the only plan available at 25% of large employers in the survey, down from 39% in 2018.
Employers have to balance their desire to control costs with their need to attract and keep workers, said Kaiser’s Altman. That leaves them less inclined to make aggressive moves to tackle underlying medical costs, such as by cutting high-cost hospitals out of their networks. In recent years employers’ healthcare costs have remained steady as a share of their total compensation expenses.
“There’s a lot of gnashing of teeth,” Altman said, “but if you look at what they do, not what they say, it’s reasonably vanilla.”
SOURCE: Tozzi, J. (25 September 2019) "Health insurance surpass $20,000 per year, hitting a record" (Web Blog Post). Retrieved from https://www.benefitnews.com/articles/health-insurance-costs-surpass-20-000-per-year
6 voluntary benefits your employees want
Multigenerational workforces are no longer finding the run-of-the-mill benefits plans adequate. This is making voluntary benefits more important than ever in this age of the multigenerational workforce and a tight labor market. Read this blog post from for six voluntary benefits employees want.
In this age of the multigenerational workforce and a tight labor market, a one-size-fits-all group benefits model with medical, prescription, dental, vision and a retirement plan just doesn’t cut it. A workforce with Baby Boomers, Gen X’ers, Millennials and Generation Z means that employees are going to find the run-of-the-mill benefits plan inadequate. Ditto for job seekers.
What follows is that voluntary benefits are more important than ever. Offering a range of voluntary benefits can help meet the needs of employees at all life stages.
Voluntary benefits add value to benefit plans and are typically easy to administer. They’re low-to-no-cost because employees pay for them, and maintenance is often handled through a payroll deduction. Many voluntary benefits also offer guaranteed acceptance at a lower rate than medical benefits, so even if a small group within your company chooses a particular benefit, they’ll be covered.
This landscape is changing quickly. Here are six trending voluntary benefits your employees want.
Student loan debt repayment assistance
Debt among college graduates has grown to nearly $1.6 trillion. It’s preventing the largest employee segment at most companies from buying houses or cars, saving for retirement, having kids and getting married. To help employees repay their student loan debt, some employers are helping employees pay down student loan debt through a direct payroll deduction.
Others are offering a new, IRS-allowable retirement plan match swap where an employer can opt to increase its defined contribution match, enabling employees to reduce their retirement match and contribute funds to repaying student loans instead.
Interest in this benefit continues to grow. Employers looking to offer student loan debt repayment should be aware that not all platforms are created equal. Look out for high per-employee, per-month fees.
Individual long-term care
A growing number of people are beginning to understand the value of long-term care insurance because they have taken care of or currently care for a friend or relative who needs round-the-clock care. Long-term care insurance covers home or institutional care if a person is no longer able to perform at least two activities of daily living--eating, bathing, dressing, moving from a bed to a chair or using a toilet.
Employees are interested in buying long-term care insurance through their employer because they can offer better rates for simplified issue plans. If you plan to offer long-term care as an employer-sponsored benefit, I recommended rolling it out with a strategic project plan and a benefit counselor or a technology platform capable of providing decision-making tools for a smooth application process.
Executive reimbursement plans
Employee retention — especially executive retention — is on the minds of many employers in the midst of this thriving economy. Filling gaps in medical and prescription coverage is one way to provide executive teams with premium benefits they may be looking for.
Executive reimbursement plans provide reimbursement for out-of-pocket expenses, access to facilities and level of service not normally covered under most group health plans. Rather than simply increasing compensation to help cover out-of-pocket expenses, premiums for these plans are tax-deductible for the employer, and benefits are non-taxable for employees.
Executive individual disability insurance
Traditional employer-sponsored long-term disability (LTD) is likely not enough coverage for highly-compensated employees or some sales staff who depends heavily on commission and bonuses. Normally, LTD pays employees 50-70% of their salary up to a certain amount.
Employers can carve out additional coverage for employees based on their management level, performance or tenure. Individual disability insurance plans can protect employees until they turn 65; they can also protect job titles or levels until employees are well enough to return to work. Executive individual disability insurance, like executive reimbursement, can be offered as a form of compensation, or a form of financial asset protection for higher incomes.
Telemedicine
The rise of consumer-driven health plans has led to the need for telemedicine. Telemedicine provides a way for employees to see a physician or provider by video and get a diagnosis and/or prescription quickly. The success of telemedicine is leading some carriers to integrate it within their plan. However, standalones still exist and can provide employees with an easy way to get care faster and cheaper than before.
Pet Insurance
Pet parents spend nearly $70 billion on veterinarian costs for their pets, but just 10% of dogs and 5% of cats are covered by medical insurance. As pets begin to play a larger role in our lives, more employers are offering pet insurance to their employees to help defray the cost of unexpected medical expenses.
There are a number of plan options, and setting up a plan for employees’ pets is simple. However, it’s vital that employers do their research to ensure the veterinarian network includes the best vets.
As part of a voluntary benefit offering, be sure to develop a rollout strategy and communications plan so employees are thoroughly educated and you meet group minimums.
SOURCE: Park, N. (25 September 2019) "6 voluntary benefits your employees want" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/6-voluntary-benefits-your-employees-want
Key elements to consider when researching financial wellness programs
With financial wellness programs becoming a staple employee benefit, organizations find themselves implementing programs that only offer a few tools or resources. Read the following blog post from Employee Benefit Advisor for key elements to consider when researching financial wellness programs.
Financial wellness programs are becoming a staple in the employee benefit universe. But what should a successful financial wellness program encompass? As a rapidly growing industry, we often lack a consistent definition for financial wellness. This leads to organizations believing they have implemented a financial wellness program, when they may only be offering a few tools like education or counseling.
I define financial wellness as the process by which an individual can efficiently and accurately assess their financial posture, identify personal goals, and be motivated to gain the necessary knowledge and resources to create behavioral change. Behavioral change will result in improved emotional and mental well-being, along with short- and long-term financial stability.
As the administrator of your company’s benefits, you are responsible for bringing the best possible solution to your employees. That’s a tough ask, given the growing number of service providers. So, what is the most efficient and effective way to assess financial wellness services to determine which solution best fits your organizational needs? Ask yourself these questions:
Does the platform offer a personal assessment of each employee’s current financial situation and help them identify their financial goals? If the answer is yes: Does the assessment return quantifiable and qualifiable data unique to each individual employee?
Does the platform address 100% of your employee base, including the least sophisticated employees at various levels of employment? Much of your ROI from a financial wellness program does not come from your top performers. It comes from creating behavioral changes within your employees who need the most financial guidance.
Does the platform integrate the various components to provide a personalized roadmap for each employee? It should connect program elements like personal assessments, educational resources, tools, feedback and solutions to ensure the employee is presented with a cohesive, comprehensive plan to attack and improve their financial situation.
Does the platform offer solutions for short-term financial challenges like cash flow issues, as well as long-term financial challenges associated with saving and planning? A major return on your investment comes from reduced employee stress, which is substantially driven by short-term needs versus long-term objectives. The program must help employees deal with current financial challenges before they can focus on their longer-term vision.
About 78% of U.S. workers live paycheck to paycheck to make ends meet, according to data from CareerBuilder.com. The need for financial wellness is clear, but there are consistent pillars that must be addressed in any successful financial wellness program to affect change: spend, save, borrow and plan. When evaluating financial wellness programs, it’s important that these dots all connect if you are truly going to motivate behavioral change and recognize the ROI of a comprehensive financial wellness program.
SOURCE: Kilby, D. (13 September 2019) "Key elements to consider when researching financial wellness programs" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/opinion/key-considerations-for-employee-financial-wellness-programs
4 pitfalls of paid leave and how clients can avoid them
Employers are using paid leave options to help boost their employee benefits packages in efforts to better attract and retain talent. Read the following blog post from Employee Benefit Advisor for 4 common pitfalls of paid leave and how employers can avoid them.
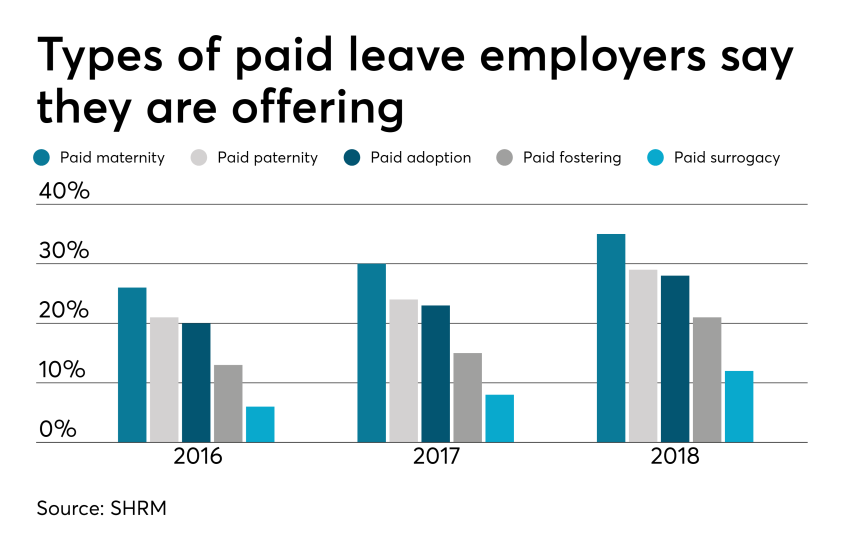 Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
But some employers are getting themselves into trouble in the process, facing accusations of gender discrimination or improper use of leave.
Here are four potential pitfalls of paid leave, and how employers can avoid them.
1. Be careful what you call “maternity leave.”
Employers have long been granting leave for new moms in the form of disability coverage. In fact, the top cause of short term disability is pregnancy. Disability insurance usually grants new moms six to eight weeks of paid leave to recover from childbirth.
Because this coverage applies to the medical condition of recovering from childbirth, it shouldn’t be lumped in with bonding leave.
Guidance from the Equal Employment Opportunity Commission says leave granted for new moms for bonding must also be extended to new dads, so separating disability leave from bonding leave is crucial to avoiding gender discrimination.
2. Don’t make gender assumptions.
The amount of bonding time for new parents after birth, adoption or fostering must be granted equally for men and women. Companies that don’t provide the same amount of paid leave for men and women may find themselves in a discrimination lawsuit.
It’s not just the time away from work that matters, but also the return-to-work support provided. If new moms are granted temporary or modified work schedules to ease the transition back to work, new dads must also have access to this.
Some companies may choose to differentiate the amount of leave and return-to-work support for primary or secondary caregivers. That’s compliant as long as assumptions aren’t made on which gender is the primary or secondary caregiver.
The best way to avoid potential gender discrimination pitfalls is to keep all parental bonding and related return-to-work policies gender neutral.
3. Avoid assuming the length of disability.
Be careful about assuming the length of time a new mom is disabled, or recovering medically, after birth. Typical coverage policies allot six to eight weeks of recovery for a normal pregnancy, so assuming a new mom may be out for 10 weeks might be overestimating the medical recovery time, and under-representing the bonding time, which must be gender neutral.
4. Keep up with federal, state and local laws.
Mandated leave laws are ever-evolving, so employers should consistently cross-check their policies with state and local laws. For instance, do local paid leave laws treat adoption the same as birth? Are multistate employers compliant? What if an employee lives in one state but works in another: Which state’s leave policies take precedence?
Partnering with a paid leave service provider can mitigate the risk of improperly administering leave. Paid leave experts can help answer questions, review guidelines and provide information regarding job-protecting medical or family leave.
They can also help flag potential pitfalls, ensuring leave requests from all areas of your company are managed uniformly and in accordance with state and federal laws, including the EEOC.
SOURCE: Bennett, A. (12 September 2019) "4 pitfalls of paid leave and how clients can avoid them" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/list/4-pitfalls-of-paid-leave-and-how-clients-can-avoid-them
U.S. Jobs Increase by 130,000 in August
According to a recent report from the Bureau of Labor Statistics (BLS), U.S. employers added 130,000 jobs this past August and the unemployment rate stayed unchanged at 3.7 percent for the third month in a row. Read this article from SHRM to learn more.
U.S. employers added 130,000 jobs in August, coming in below economists' expectations, and the unemployment rate held at 3.7 percent for the third straight month, according to the latest Bureau of Labor Statistics (BLS) report.
July's employment total was revised down from 164,000 new jobs to 159,000. In the past three months, job gains averaged 156,000 a month after revisions.
"Today's jobs report shows slowing private-sector job growth and slowing wage growth, which—while expected this late in the recovery—is somewhat disappointing after the rapid gains of the past two years," said Julia Pollak, a labor economist at employment marketplace ZipRecruiter.
On Sept. 5, the ADP Research Institute and Moody's Analytics reported private-sector growth of 195,000 new jobs, better than economists' expectations of about 160,000 jobs.
"Despite the slower growth in jobs added, labor force participation did perk up, a sign that the healthy labor market is still drawing in workers from the sidelines," said Glassdoor senior economist Daniel Zhao.
The labor force participation rate—which includes people who are working and those looking for work—ticked up to 63.2 percent, one of its highest readings in years. The proportion of the population currently employed is at 60.9 percent, its highest point since December 2008. And the employment-to-population ratio for workers aged 25-54 reached 80 percent for the first time since January 2008.
Zhao said that the increases signal that the tightness of the labor market is putting upward pressure on labor force participation despite an aging population pulling it down.
Michael Stull, senior vice president at the staffing and recruiting firm Manpower North America, said other positive takeaways from the report are better than expected wage growth and strong hiring in the professional and business, financial and health care sectors.
Job gains in August were led by professional and business services (37,000 new jobs), which includes many technology jobs and the nation's booming health care industry (23,900). Other industries showing gains include finance (15,000) and construction (14,000).
"Health care and professional services have both grown strongly across 2019, carrying the labor market despite weakness in the goods-producing sectors," Zhao said. "Additionally, the increase in temporary help services [15,400 jobs] is a good sign that employers are not cutting back on the most flexible parts of their workforces in the face of recession chatter."
However, Pollak noted that the BLS reported that the private sector only added 96,000 jobs, marking a slowdown from the pace of job growth over the last two years.
Industries like mining and manufacturing are struggling. Mining employment fell by 5,600 jobs and manufacturers have seen a marked slowdown in job creation, with only 3,000 jobs added in August. "In 2018, manufacturing job growth exceeded 10,000 jobs in 11 of 12 months, but this year job growth has been below 10,000 or even negative in six of eight months," Pollak said. "Trade policy uncertainty and a global manufacturing slowdown seem to have brought the 2017-2018 manufacturing boom to a halt."
The retail sector lost 11,000 jobs in August, continuing a trend of month-over-month declines for the seventh consecutive month. "Despite strong consumer spending, increasing labor costs and the rise of e-commerce are keeping retail hiring down even as we begin to enter the holiday hiring season," Zhao said. "We'll be watching the next few reports for signs that the holiday retail hiring season has slowed or that the latest round of tariffs are having a larger effect on the retail industry."
Juiced by Census Hires
U.S. jobs data is now—and will for some time be—inflated by a temporary spike in government hiring for 2020 Census workers. The federal government added 28,000 workers (excluding U.S. Post Office hires) to its payrolls in August. The majority of those—25,000 temporary workers—will go door-to-door over the next several weeks to verify addresses ahead of the 2020 count.
The Census Bureau expects to hire about 40,000 people for this preliminary duty and about 500,000 workers next year for the actual canvassing.
Unemployment Stays Low
The BLS data showed that the national unemployment rate remained below 4 percent for the 18th consecutive month. The number of unemployed people held at 6 million.
"The unemployment rate remains near its lowest level in 50 years, again signaling the strength of the labor market for workers as the number of job openings continues to exceed the number of unemployed workers," Zhao said.
The number of long-term unemployed (those jobless for 27 weeks or more) rose from 1.1 million to 1.2 million in August and accounted for 20.6 percent of the unemployed.
The U-6 unemployment rate—a broader measure capturing both the unemployed, underemployed and those too discouraged to seek work—continued its long decline and held at 7.3 percent for the second month in a row. There were 467,000 discouraged workers in August, about the same as a year ago.
"There are still more discouraged workers than we would expect, given the low unemployment rate," Pollak said. "Discouraged workers are those who are out of work but have not applied for a job in the past four weeks because they think there are none available or none for which they qualify," she explained. "If there were fewer discouraged workers, labor force participation and employment rates would be higher, and more vacancies would be filled."
Wages Inch Up
Average hourly earnings increased 11 cents to $28.11, following 9-cent gains in both June and July. Over the past 12 months, average hourly earnings have increased by 3.2 percent.
"At this point in the expansion, we'd expect wage growth to pick up, but it is continuing to stall," said Nick Bunker, a Washington, D.C.-based economist at the Indeed Hiring Lab. "Wage growth continues to be strongest for workers in lower-wage industries."
SOURCE: Maurer, R. (06 September 2019) "US Jobs increase by 130,000 in August" (Web Blog Post). Retrieved from https://www.shrm.org/resourcesandtools/hr-topics/talent-acquisition/pages/bls-hr-jobs-unemployment-august-2019.aspx
What would change if your employees were CEO for a day?
How is your workplace culture? New data shows that employees are 4.6 times more likely to contribute their best work when they feel like their voices are being heard. Read this blog post from Employee Benefits News to learn more about building a strong workplace culture.
When employees feel like their voices are being heard, they are reportedly 4.6 times more likely to contribute their best work, according to SalesForce data. Ultimately, knowing that the company is interested in what employees have to say builds trust and encourages loyalty among members of the workforce.
Respect is the most important leadership behavior, according to a Georgetown University survey of nearly 20,000 employees. More than merely listening, making employees a part of a two-way conversation shows that the company values their opinions.
With this in mind, we set out to develop a process to help Nearmap increase workplace communication. Along the way, we found that creating opportunities for interaction, encouraging honest participation and involving executive participation were all keys to building a stronger corporate culture.
Invite employee interaction
We recognized that we needed a conversation starter to open the lines of communication and spark a little enthusiasm. We discovered that engagement surveys work the best for our circumstances because they’re quick and easy to take, which results in high completion rates.
We like to include thought-provoking questions like “if you were CEO for a day, what is the one thing you would change?” to keep the employees engaged. At first, that particular question provided some of our most entertaining suggestions, including “free umbrellas for all,” “I would like the CEO’s paycheck,” “change my LinkedIn profile,” and “put margarita slushy machines in the kitchen.” When employees saw that the CEO responded to every answer, they realized that we were taking the feedback seriously, and that changed the tone of their responses.
Anonymity invites honest responses
It was essential to Nearmap that we collect unfiltered, honest feedback from our employees. This meant reassuring participants that their responses were completely anonymous. We believe this confidentiality encouraged authentic and candid submissions from employees that otherwise would have remained silent for fear of reprimand or judgment.
For instance, we’ve received excellent insights about driving the strategy and growth of the business, giving Nearmap valuable concepts that we’ve been able to embed into the business.
In addition, we present the survey results back to the employees so they can see how their thoughts align with those of their co-workers. We believe this commitment to being open is an excellent way to motivate honest dialog.
Executive participation leads by example
When the survey concludes, we group all of the responses under different headings, such as collaboration and communication, marketing, mission, planning, product, compensation, recognition, and general. Then, our CEO, Rob Newman, gets together with other executives to provide answers and comments on many of the submissions. In turn, those responses are shared with the employees via the HR newsletter and on our company collaboration app.
In reply to an inquiry about creating a green initiative for the company, our CEO shared a list of active programs that Nearmap was involved in to reduce not only our carbon footprint but also that of our customers as well.
While we may not know what we would change if we were the CEO for a day, we are convinced that employee interaction, honest responses and executive participation are reliable and important ways to make impactful connections with our employees and build a stronger corporate culture in our company.
SOURCE: Steel, S. (13 September 2019) "What would change if your employees were CEO for a day?" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/what-would-change-if-your-employees-were-ceo-for-a-day
8 renewal considerations for 2020
Are you prepared for open enrollment 2020? With renewal season quickly approaching, plan administrators have a lot of considerations to make regarding employee health plans. Read the following blog post from Employee Benefit News for eight things to consider this year.
The triumphant return of the Affordable Care Act premium tax (the health insurer provider fee).
This tax of about 4% is under Congressional moratorium for 2019 and returns for 2020. Thus, fully insured January 2020 medical, dental and vision renewals will be about 4% higher than they would have been otherwise. Of note, this tax does not apply to most self-funded contracts, including so-called level-funded arrangements. Thus, if your plans are presently fully insured, now may be a good time to re-evaluate the pricing of self-funded plans.
Ensure your renewal timeline includes all vendor decision deadlines.
As the benefits landscape continues to shift and more companies are carving out certain plan components, including the pharmacy benefit manager, you may be surprised with how early these vendors need decisions in order to accommodate benefit changes and plan amendments. Check your contracts and ask your consultant. Further, it seems that our HRIS and benefit administration platforms are ironically asking for earlier and earlier decisions, even with the technology seemingly improving.
Amending your health plan for the new HSA-eligible expenses.
In July of this year, the U.S. Treasury loosened the definition of preventive care expenses for individuals with certain conditions.
While these regulations took effect immediately, they won’t impact your health plan until your health plan documents are amended. Has your insurer or third-party administrator automatically already made this amendment? Or, will it occur automatically with your renewal? Or is it optional? If your answer begins with “I would assume…,” double-check.
Amending your health plan for the new prescription drug coupon regulations.
As we discussed in July of this year, these regulations go into effect when plans renew in 2020. In short, plans can only prevent coupons from discounting plan accumulators (e.g., deductible, out-of-pocket maximum) if there is a “medically advisable” generic equivalent.
If your plan is fully insured, what action is your insurer taking? Does it seem compliant? If your plan is self-funded, what are your options? If you can keep the accumulator program and make it compliant, is there enough projected program savings to justify keeping this program?
Is your group life plan in compliance with the Section 79 nondiscrimination rules?
A benefit myth that floats around from time to time is that the first $50,000 in group term life insurance benefits is always non-taxable. But, that’s only true if the plan passes the Section 79 nondiscrimination rules. Generally, as long as there isn’t discrimination in eligibility terms and the benefit is either a flat benefit or a salary multiple (e.g., $100,000 flat, 1 x salary to $250,000), the plan passes testing. Ask your attorney, accountant, and benefits consultant about this testing. If you have two or more classes for life insurance, the benefit is probably discriminatory. If you fail the testing, it’s not the end of the world. It just means that you’ll likely need to tax your Section 79-defined “key employees” on the entire benefit, not just the amount in excess of $50,000.
Is your group life maximum benefit higher than the guaranteed issue amount?
Surprisingly, I still routinely see plans where the employer-paid benefit maximum exceeds the guaranteed issue amount. Thus, certain highly compensated employees must undergo and pass medical underwriting in order to secure the full employer-paid benefit. What often happens is that, as benefit managers turnover, this nuance is lost and new hires are not told they need to go through underwriting in order to secure the promised benefit. Thus, for example, an employee may think he or she has $650,000 in benefit, while he or she only contractually has $450,000. What this means is the employer is unknowingly self-funding the delta — in this example, $200,000. See the problem?
Please pick up your group life insurance certificate and confirm that the entire employer-paid benefit is guaranteed issue. If it is not, negotiate, change carriers, or lower the benefit.
Double-check that you haven’t unintentionally disqualified participant health savings accounts (HSAs).
As we discussed last December, unintentional disqualification is not difficult.
First, ensure that the deductibles are equal to or greater than the 2020 IRS HSA statutory minimums and the out-of-pocket maximums are equal to or less than the 2020 IRS HSA statutory maximums. Remember that the IRS HSA maximum out-of-pocket limits are not the same as the Affordable Care Act (ACA) out-of-pocket maximum limits. (Note to Congress – can we please align these limits?)
Also, remember that in order for a family deductible to have a compliantly embedded single deductible, the embedded single deductible must be equal to or greater than the statutory minimum family deductible.
Complicating matters, also ensure that no individual in the family plan can be subject to an out-of-pocket maximum greater than the ACA statutory individual out-of-pocket maximum.
Finally, did you generously introduce any new standalone benefits for 2020, like a telemedicine program, that Treasury would consider “other health coverage”? If yes, there’s still time to reverse course before 2020. Talk with your tax advisor, attorney, and benefits consultant.
Once all decisions are made, spend some time with your existing Wrap Document and Wrap Summary Plan Description.
For employers using these documents, it’s easy to forget to make annual amendments. And, it’s easy to forget, depending on the preparer, how much detail is often in these documents. For example, if your vision vendor changes or even if your vision vendor’s address changes, an amendment is likely in order. Ask your attorney, benefits consultant, and third party administrators for help.
SOURCE: Pace, Z. (Accessed 9 September 2019) "8 renewal considerations for 2020" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/healthcare-renewal-considerations-for-2020
Putting Humanity into HR Compliance: Stop Tolerating Toxicity
HR departments who have a detox mission and address toxic workplace relationships can prove incredibly valuable to their organizations. Not only are employees and their well-being impacted by toxic workplace relationships, but also the organizational success and the well-being of employees' family members. Continue reading this blog post to learn more.
In my prior career as an employment attorney and in my current one as an organizational consultant and coach, I have encountered numerous toxic workplace relationships. The cost of these relationships—to organizational success, employee well-being and the well-being of employees' family members—is astronomical.
And the greatest tragedy is this: Almost all of this loss, pain and suffering is preventable.
Why are toxic workplace relationships so common? And why are they tolerated?
The answer to the first question is that good people make bad decisions. Typically, employee relationships start out fine. Employees cooperate and collaborate in their relationships with their bosses and peers.
But then something goes awry. A trust gap opens. The employee does not address the problem promptly, directly and constructively, but the employees' avoidance instinct kicks in. Nothing constructive is done to close the trust gap. As a result, the problem festers and grows. Eventually, any remaining trust evaporates, and the relationship degenerates into aggression, passive aggression or both.
Note that I'm not talking about the incorrigible "work jerk," whose behavior should never be tolerated. Rather, I'm talking about people stuck in toxic work relationships producing jerkish and other negative behavior.
Managers and HR practitioners succumb to the avoidance instinct, too. Although aware of the toxicity, they don't intervene and are wary of wading into others' dysfunctional relationships.
What are the costs of tolerating toxicity?
- Personal suffering. The immediate parties may think they have nothing in common, but they do: They're equally disengaged and miserable.
- Work loss. Toxic relationships do nothing to improve the quantity or quality of work, customer service or on-the-job innovation. There is increased absenteeism and what Colleen McManus, SHRM-SCP, an HR executive with the state of Arizona, calls "presenteeism," in which people are at work but not focused on work, dwelling on negativity instead of doing their jobs properly.
- Secondhand anxiety. Co-workers who witness the toxic behavior suffer, as does their contribution to the organization. They are the truly innocent victims.
- Collateral damage. Employees affected by workplace toxicity typically bring their stress home. This doesn't reduce their stress; rather, it elevates their loved ones' stress. "So true! In the most serious situations," McManus said, "I have seen greater instances of alcoholism and domestic violence due to problems at work."
How HR Can Help
HR departments with a detox mission can prove incredibly valuable to their organizations and the people in them. It's not hard to identify toxic relationships. The challenge is taking action.
I can say with confidence that intervention is always better than tolerating toxicity. You'd be surprised how easily many toxic relationships can be reset when a skilled third party steps in. HR professionals are ideally positioned to help employees stuck in toxic relationships get back on track. Or, if there's too much baggage, HR professionals can facilitate a respectful relocation of the parties to different positions in the organization. This method is a good way to start.
Many times, a toxic relationship is rooted in an unwitting and unaddressed offense one employee gave the other. As a result, the offended party started behaving differently toward the offender, which produced more offensive behavior, and so on. "I'm always surprised," McManus said, "when I ask the parties to the conflict what a resolution looks like. Often, it's simply an opportunity to be heard."
She adds that a sincere apology goes a long way toward rebuilding trust. "They feel validated, which is important to them."
Sometimes there's a structural misfit in the workers' roles that needs to be clarified, or how the jobs interact needs to be modified. HR can help figure out how the jobs can function without recurrent friction. "This is our profession's bread and butter!" McManus said.
There may be a personality conflict, in which case the parties need better understanding of how to interact with people whose styles differ from theirs. If that can't be achieved, though, there can be an agreement to disagree and respectfully move on—whether to a different position inside or outside the organization.
An HR team that makes a commitment to identify and resolve toxic relationships is empowered by the CEO, and is supported by the leadership team will prove to be incredibly valuable to its organization and the people in it. HR team members can directly coach others to resolve conflicts and show managers how to coach their employees who are stuck in toxic relationships.
There's also a risk management, compliance and claim-prevention component. In my employment lawyer days, most of my billable hours arose from conflict caused by toxic workplace relationships. An HR profession with a detox mission will become painfully costly to my former profession.
SOURCE: Janove, J. (Sept 06, 2019) "Putting Humanity into HR Compliance: Stop Tolerating Toxicity" (Web Blog Post) Retrieved from https://www.shrm.org/resourcesandtools/hr-topics/employee-relations/pages/putting-humanity-into-hr-compliance-stop-tolerating-toxicity-.aspx
5 Questions Expecting Moms Have About Life Insurance
Are you considering life insurance? If this is your first time looking for coverage, you most likely have questions. Read this blog post from Life Happens for five questions expecting mothers typically ask when looking at life insurance.
If you are expecting a child and are considering life insurance, the first thing I have to say is—smart move! But if this is your first time looking for coverage, you may have questions. Here are some typical ones I’ve heard over the years:
1. What type of life insurance coverage is best for new parents—term or permanent?
Before figuring out what kind of coverage you need, you first have to understand how much death benefit you need to protect your family. You can do an easy calculation online to get a working idea of how much you may need with this Life Happens Life Insurance Needs Calculator.
Then you can move on to what kind of coverage—term or permanent—meets your needs. An advantage of term life insurance is that it costs less than permanent, at least initially. This makes it affordable for young families that may not have a lot of disposable income, but have a large need for coverage. Permanent insurance provides both lifelong coverage and a cash accumulation feature, which can be a valuable source of money that you can tap in the future.
Often, the best solution can be a combination of term and permanent life insurance. The term policy can give you extra coverage during the years when the children are at home, with the permanent policy offering lifelong coverage.
2. Should you consider different types of coverage if you are working mom versus a stay-at-home mom?
Both working and stay-at-home moms need protection because what they do for their families is so valuable. While a stay-at-home mom isn’t compensated for her work, if something were to happen to her, it would be expensive to replace all those things she does—from childcare to home care to ensuring the family gets where they need to go when they have to be there.
The difference between the two is that a working mother also contributes an income, which may be critical to the family financially. That means she needs to think about replacing that income when considering how much life insurance coverage she may need.
3. The company where I work offers life insurance, is that enough?
Group insurance is a great benefit to have, but it’s limited in a number of ways. First, the coverage is often a lump sum, such as $50,000, or it may be one to two times your salary. That may sound like a lot of money, but my question to you is: Honestly, how long would that money last? And what would happen to your family financially after that was gone?
Second, when you leave that job, you generally lose that coverage. If you don’t have an individual policy that you own, you’ll be leaving your family at risk. Think of how many times people change jobs, and you’ll quickly realize that group coverage, which is limited in scope and amount, is not a proper life insurance plan.
4. Are there any restrictions I have to consider now that I’m pregnant?
If it’s early in your pregnancy, and there are no medical complications, you should be able to get life insurance. If you’re farther along and there are medical issues, it may difficult to obtain. The life insurance company may want to wait until after your child is born. That’s why I advise those that are planning to have children to get the coverage as soon as possible.
5. What can I expect to pay for life insurance?
How much you pay for life insurance is based on a number of things but most importantly age and health. So, it depends on how old and how healthy you are! But here’s an example: A healthy 30-year-old woman could get $250,000 in life insurance coverage (for a 20-year level term policy for a nonsmoker) for about $13 a month. That’s certainly a lot of peace of mind for $13.
And don’t forget about your spouse or partner. The two of you could get $500,000 of combined coverage (using the example of two 30-year-olds that each get a $250,000 20-year level term policy) for right around $26 a month.
And my last piece of advice: talking with a life insurance agent at this stage can be very valuable. They can do a needs assessment and come up with the right type and amount of life insurance that works for your family budget. And what many people don’t realize is that an agent will sit down and offer this advice free of charge, with no strings attached. If you’d like help finding a life insurance professional, you can start here.
SOURCE: Feldman, M. (23 August 2019) "5 Questions Expecting Moms Have About Life Insurance" (Web Blog Post). Retrieved from https://lifehappens.org/blog/5-questions-expecting-moms-have-about-life-insurance/
A 401(k) plan administrators’ guide to the recent IRS revenue ruling
The IRS recently released a new revenue ruling that provides 401(k) plan administrators with helpful guidance on reporting and withholding from 401(k) plan distributions. Read the blog post below to learn more about this new ruling.
The IRS recently issued revenue ruling 2019-19. The revenue ruling provides 401(k) plan administrators with helpful guidance on how to report and withhold from 401(k) plan distributions when a plan participant actually receives the distribution but for some reason, does not cash the check.
Unfortunately, this new guidance does not provide answers to the complex issues that 401(k) plan administrators face when the plan must make a distribution, but the plan participant is missing.
Let’s hope revenue ruling 2019-19 is just the first in a series of much-needed guidance from the IRS and the Department of Labor about how 401(k) plan administrators should handle the increasingly common administrative issues related to uncashed checks and missing plan participants.
There are many situations in which a 401(k) plan must make a distribution to a plan participant. For example, plans must distribute small benefit cash outs (e.g., account balances that are $1,000 or less) or required minimum distributions to plan participants who reach age 70 and a half. This may come as a surprise, but plan participants fail to actually cash these checks with some regularity.
In the ruling, the IRS confirmed that 401(k) plan administrators should withhold taxes on a 401(k) plan distribution and report the distribution on a Form 1099-R in the year the check is distributed to the participant, even if the participant does not cash the check until a later year.
Similarly, the participant needs to include the plan distribution as taxable income in the year in which the plan makes the distribution even if the participant fails to cash the check until a later year. While this guidance is not surprising, it does provide clarity to 401(k) plan administrators as to how they must withhold and report normal course and required plan distributions. In particular, 401(k) plan administrators should not reverse the tax withholding or reporting of the distribution when the participant receives the distribution and simply does not cash the check until a later year.
Unfortunately, this new IRS guidance has limited use because the ruling uses an example that specifically concedes that the plan participant actually received the plan distribution check, but simply failed to cash it. What should 401(k) plan administrators do when the participant may not have received the distribution check at all (e.g., a check is returned for an invalid address) or the plan itself does not have current contact information for the participant?
Retirement plan administrators have an ERISA fiduciary obligation to implement a diligent and prudent process to find missing plan participants and to take additional steps to make sure participants actually receive plan distributions. Uncashed 401(k) plan distribution checks are still retirement plan assets which means the 401(k) plan administrator is still subject to ERISA fiduciary standards of care, prudence and diligence related to those amounts. As a result, the IRS and DOL have increased their focus on uncashed checks and missing participants in retirement plan audits.
Plan administrators would be well-served by establishing and implementing a consistent process to stay on top of any missing plan participants or uncashed checks and taking steps to locate those participants and properly address uncashed checks. Plan administrators should also carefully document the steps that they take in this regard. The IRS and DOL have currently provided limited guidance on the steps a 401(k) plan administrator can take to locate missing participants, but more guidance is needed — let’s hope revenue ruling 2019-19 is just the beginning.
This article originally appeared on the Foley & Lardner website. The information in this legal alert is for educational purposes only and should not be taken as specific legal advice.
SOURCE: Dreyfus Bardunias, K. (6 September 2019) "A 401(k) plan administrators’ guide to the recent IRS revenue ruling" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/401k-administrators-guide-to-the-irs-revenue-ruling-2019-19










