Tax Bill Provision Designed To Spur Paid Family Leave To Lower-Wage Workers

Tucked into the new tax law is a provision that offers companies a tax credit if they provide paid family and medical leave for lower-wage workers.
Many people support a national strategy for paid parental and family leave, especially for workers who are not in management and are less likely to get that benefit on the job. But consultants, scholars and consumer advocates alike say the new tax credit will encourage few companies to take the plunge.
The tax credit, proposed by Sen. Deb Fischer (R-Neb.), is available to companies that offer at least two weeks of paid family or medical leave annually to workers, but two key criteria must be met. The workers must earn less than $72,000 a year and the leave must cover at least 50 percent of their wages.
If contributing at the half-wage level, a company receives a tax credit equal to 12.5 percent of the amount it pays to the worker. The tax credit will increase on a sliding scale if the company pays more than 50 percent of wages. It could go up to a maximum credit of 25 percent of the amount the employer paid for up to 12 weeks of leave.
Payments to full- and part-time workers taking family leave who’ve been employed for at least a year would be eligible for the employer’s tax break. But the program, which is designed to test whether this approach works well, is set to last just two years, ending after 2019.
Aparna Mathur, a resident scholar in economic policy studies at the American Enterprise Institute, says the new tax credit sidesteps a pitfall for Republicans. They are wary of any legislation mandating that employers provide paid leave. The tax credit also is appropriately aimed at lower-wage workers who are most likely to lack access to paid leave, said Mathur, who co-authored a recent report on paid family leave.
But it’s not a big enticement.
“Providing this benefit is a huge cost for employers,” Mathur said. “It’s unlikely that any new companies will jump on board just because they have a 12.5 to 25 percent offset.”
That view is shared by Vicki Shabo, vice president for workplace policies and strategies at the National Partnership for Women & Families, an advocacy group, who said it will primarily benefit workers at companies already offering paid family leave. The new tax credit “just perpetuates the boss lottery,” she added.
Heather Whaling said her 22-person public relations company probably qualifies for the new tax credit, but she doesn’t think it’s the right approach. Whaling, the president of Geben Communication in Columbus, Ohio, already offers paid leave. The company provides up to 10 weeks of paid leave at full pay for new parents. Four employees have taken leave, and by divvying up their work to other team members and hiring freelancers they’ve been able to get by.
“It is an expense, but if you plan and budget carefully it’s not cost-prohibitive,” she said.
The tax credit isn’t big enough to provide a strong incentive to provide paid leave, said Whaling, 37. Besides, “having access to paid family leave shouldn’t be luck of the draw, it should be available to every employee in the country.”
Still, the tax credit may be appealing to companies that have been considering adding a paid family and medical leave benefit, said Rich Fuerstenberg, a senior partner at benefits consultant Mercer.
By defraying some of the cost, the tax credit could help “tip them over” into offering paid leave, he said. But “I’m not even sure I’d call it the icing on the cake,” Fuerstenberg said. “It’s like the cherry on the icing.”
Only 15 percent of private-sector and state and local government workers had access to paid family and medical leave in 2017, according to the Bureau of Labor Statistics’ National Compensation Survey. Eighty-eight percent had access to unpaid leave, however.
Under the federal Family and Medical Leave Act, employers with 50 or more workers generally must allow eligible employees to take unpaid leave for up to 12 weeks annually for specified reasons. These include the birth or adoption of a child, caring for your own or a family member’s serious health condition, or leave for military caregiving or deployment. An individual’s job is protected during such leaves.
A tax credit that can be claimed at the end of the year is unlikely to encourage small businesses to offer paid family and medical leave, said Erik Rettig, an expert on family leave policies at the Small Business Majority, which advocates for those firms on national policy.
“It isn’t going to help the family business that has to absorb the costs of this employee while they’re gone,” Rettig said.
A better solution, according to Shabo and others, is to provide a paid family leave benefit that’s funded by employer and/or employee payroll contributions. Sen. Kirsten Gillibrand (D-N.Y.) and Rep. Rosa DeLauro (D-Conn.) last year reintroduced such legislation. Their bill would guarantee workers, including those who are self-employed, up to 12 weeks of family and medical leave with as much as two-thirds of their pay.
A handful of mostly Democratic states — including California, New Jersey, Rhode Island and New York — have similar laws in place, and a program in the District of Columbia and Washington state will begin in 2020.
“We know from states that this approach works for both employees and their bosses,” Shabo said.
Read the original article.
Source: Andrews M. (23 January 2018). "Tax Bill Provision Designed To Spur Paid Family Leave To Lower-Wage Workers" [Web blog post]. Retrieved from address https://khn.org/news/tax-bill-provision-designed-to-spur-paid-family-leave-to-lower-wage-workers/
SaveSave
Despite Compressed Sign-Up Period, ACA Enrollment Nearly Matches Last Year’s
President Trump decided to take away ACA, but that didn’t stop people from signing up. Read this article for the shocking numbers of enrollment.
A day after President Donald Trump said the Affordable Care Act “has been repealed,” officials reported that 8.8 million Americans have signed up for coverage on the federal insurance exchange in 2018 — nearly reaching 2017’s number in half the sign-up time.
That total is far from complete. Enrollment is still open in parts of seven states, including Florida and Texas, that use the federal healthcare.gov exchange but were affected by hurricanes earlier this year. The numbers released Thursday by the Department of Health and Human Services also did not include those who signed up between midnight Dec. 15 and 3 a.m. ET on Dec. 16, the final deadline for 2018 coverage, as well as those who could not finish enrolling before the deadline and left their phone number for a call back.
And enrollment has not yet closed in 11 states — including California and New York — plus Washington, D.C., that run their own insurance exchanges. Those states are expected to add several million more enrollees.
The robust numbers for sign-ups on the federal exchange — 96 percent of last year’s total — surprised both supporters and opponents of the health law, who almost universally thought the numbers would be lower. Not only was the sign-up period reduced by half, but the Trump administration dramatically cut funding for advertising and enrollment aid. Republicans in Congress spent much of the year trying to repeal and replace the law, while Trump repeatedly declared the health law dead, leading to widespread confusion.
On the other hand, a Trump decision aimed at hurting the exchanges may have backfired. When he canceled federal subsidies to help insurers offer discounts to their lowest-income customers, it produced some surprising bargains for those who qualify for federal premium help. That may have boosted enrollment.
“Enrollment defied expectations and the Trump administration’s efforts to undermine it,” said Lori Lodes, a former Obama administration health official who joined with other Obama alumni to try to promote enrollment in the absence of federal outreach efforts. “The demand for affordable coverage speaks volumes — proving, yet again, the staying power of the marketplaces.”
“The ACA is not repealed and not going away,” tweeted Andy Slavitt, who oversaw the ACA under President Barack Obama.
The tax bill passed by Congress this week repeals the fines for those who fail to obtain health coverage, but those fines do not go away until 2019. Still, that has added to the confusion for 2018 coverage.
And it remains unclear whether Congress will make another attempt to repeal the law in 2018.
“I think we’ll probably move on to other issues,” Senate Majority Leader Mitch McConnell (R-Ky.) said in an interview Friday with NPR.
Read further.
Source: Rovner J. (21 December 2017). "Despite Compressed Sign-Up Period, ACA Enrollment Nearly Matches Last Year’s" [Web Blog Post]. Retrieved from address https://khn.org/news/despite-compressed-sign-up-period-aca-enrollment-nearly-matches-last-years/view/republish/
HHS Nominee Vows To Tackle High Drug Costs, Despite His Ties To Industry
What is President Trump’s solution for fighting high drug prices? From Kaiser Health News, check out this article on the new Department of Health and Human Services (HHS) nominee.
Senate Democrats on Tuesday pressed President Donald Trump’s nominee for the top health post to explain how he would fight skyrocketing drug prices — demanding to know why they should trust him to lower costs since he did not do so while running a major pharmaceutical company.
Alex M. Azar II, the former president of the U.S. division of Eli Lilly and Trump’s pick to run the Department of Health and Human Services, presented himself as a “problem solver” eager to fix a poorly structured health care system during his confirmation hearing before the Senate Finance Committee. Azar said addressing drug costs would be among his top priorities.
But armed with charts showing how some of Eli Lilly’s drug prices had doubled on Azar’s watch, Democrats argued Azar was part of the problem. Sen. Ron Wyden of Oregon, the committee’s top Democrat, said Azar had never authorized a decrease in a drug price as a pharmaceutical executive.
“The system is broken,” Wyden said. “Mr. Azar was a part of that system.”
Azar countered that the nation’s pharmaceutical drug system is structured to encourage companies to raise prices, a problem he said he would work to fix as head of HHS.
“I don’t know that there is any drug price of a brand-new product that has ever gone down from any company on any drug in the United States, because every incentive in this system is towards higher prices, and that is where we can do things together, working as the government to get at this,” he said. “No one company is going to fix that system.”
Azar’s confirmation hearing Tuesday was his second appearance before senators as the nominee to lead HHS. In November, he faced similar questions from the Senate Health, Education, Labor and Pensions Committee during a courtesy hearing.
If confirmed, Azar would succeed Tom Price, Trump’s first health secretary, who resigned in September amid criticism over his frequent use of taxpayer-paid charter flights. A former Republican congressman who was a dedicated opponent of President Barack Obama’s signature health care law, Price had a frosty relationship with Democrats in Congress as he worked with Republicans to try to undo the law.
Price and the Trump administration often turned to regulations and executive orders to undermine the Affordable Care Act, since Republicans in Congress repeatedly failed to enact a repeal. “Repeal and replace” has been the president’s mantra.
But at the hearing, Azar was circumspect about his approach, noting that his job would be to work under existing law. “The Affordable Care Act is there,” he said, adding that it would fall to him to make it work “as best as it possibly can.”
Senate Republicans touted Azar’s nearly six years working for the department under President George W. Bush, including two years as a deputy secretary. Committee Chairman Orrin Hatch (R-Utah) praised Azar’s “extraordinary résumé,” adding that, among HHS nominees, he was “probably the most qualified I’ve seen in my whole term in the United States Senate.” Hatch, who is the longest-serving Republican senator in history, has been a senator for more than 40 years.
In addition to drug costs, Azar vowed to focus on the nation’s growing opioid crisis, calling for “aggressive prevention, education, regulatory and enforcement efforts to stop overprescribing and overuse,” as well as “compassionate treatment” for those suffering from addiction.
Pressed about Republican plans to cut entitlement spending to compensate for budget shortfalls, Azar said he was “not aware” of support within the Trump administration for such cuts.
“The president has stated his opposition to cuts to Medicaid, Medicare or Social Security,” Azar said. “He said that in the campaign, and I believe he has remained steadfast in his views on that.”
But Democrats pushed back, pointing out that Trump had proposed Medicaid cuts in his budget request last year. Sen. Sherrod Brown (D-Ohio) said such cuts would hurt those receiving treatment for opioid addiction.
“What happens to these people?” he said.
Despite such Democratic criticism, Azar is likely to be confirmed when the full Senate votes on his nomination. An HHS spokesman Tuesday pointed reporters to an editorial in STAT supporting Azar, written by former Senate majority leaders Bill Frist and Tom Daschle — a Republican and a Democrat. “We need a person of integrity and competence at the helm of the Department of Health and Human Services,” they wrote. “The good news is that President Trump has nominated just such a person, Alex Azar.”
Read further.
Source:
Huetteman E. (9 January 2018). "HHS Nominee Vows To Tackle High Drug Costs, Despite His Ties To Industry" [Web blog post]. Retrieved from address https://khn.org/news/hhs-nominee-vows-to-tackle-high-drug-costs-despite-his-ties-to-industry/view/republish/
Level-funded plan uptake trickling down market
What are level-funded plans, and why are they becoming so popular? Allow this article to break down the facts for you.
A brighter light is being cast on level-funded group health plans as benefits decision-makers tackle open-enrollment season. Several industry observers say the trend is more pronounced given that the Affordable Care Act remains largely intact — for now.
There has been an ebb and flow to these self-insured underwritten plans over the past 18 months, says Michael Levin, CEO and co-founder of the healthcare data services firm Vericred. But with a fixed monthly rate for more predictability, he says they can drive 25% to 35% savings relative to fully-insured ACA plans that must comply with the medical loss ratio for a certain segment of the market.
Level funding typically leverages an aggregate and/or specific stop-loss product to cap exposure to catastrophic claims. These plans are offered by an independent third-party administrator or health insurance carrier through an administrative-services-only contract.
It’s best suited for companies with a very low risk profile comprised of young or healthy populations, according to Levin. And with low attachment, stop-loss coverage in most states, he explains that the plans have “very little downside risk from the group’s perspective.” Two exceptions are California and New York whose constraints on the stop-loss attachment point “essentially preclude level-funded plans from being offered” there, he adds.
The arrangement is trickling down market. “We’ve heard from carriers that will go down to seven employees, plus dependents, while others cut it off at 20 or 25,” he says.
David Reid, CEO of EaseCentral, sees a “resurgence of level funding” across more than 38,000 employers with less than 500 lives that his SaaS platform targets through about 6,000 health insurance brokers and 1,000 agencies. His average group is about 30 employees.
He’s also seeing more customers using individual-market plans rather than group coverage through Hixme’s digital healthcare benefits consulting platform. Under this approach, health plans are bundled with other specific types of insurance and financing as a line of credit to fill coverage gaps. Employer contributions are earmarked for individual-market plans, which are purchased through payroll deduction.
Read further.
Source: Shutan B. (17 November 2017). "Level-funded plan uptake trickling down market" [Web Blog Post]. Retrieved from address https://www.employeebenefitadviser.com/news/level-funded-plan-uptake-trickling-down-market?feed=00000152-175e-d933-a573-ff5ef1df0000
Two Months After Hurricane Maria, A Growing Majority Of Americans Say Puerto Ricans are Not Yet Getting the Help They Need
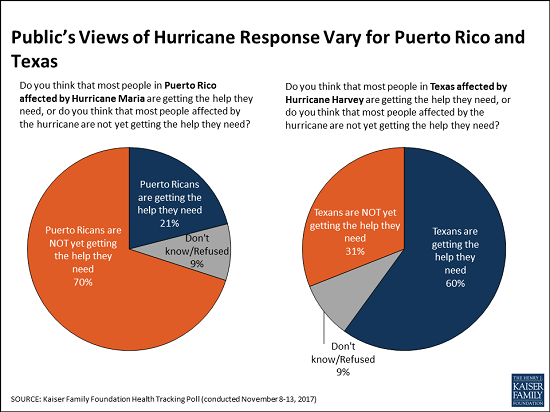
Two months after Hurricane Maria struck Puerto Rico, a growing majority of Americans say that Puerto Ricans affected by the devastating storm are not yet getting the help they need, the November Kaiser Family Foundation Tracking Poll finds.
This month, 70 percent of the public say that people in Puerto Rico are not yet getting the help they need, up from 62 percent in October 2017. These perceptions vary by party, and half of Republicans (52%) now say Puerto Ricans aren’t yet getting needed help, up significantly from October (38%).
When asked whether the federal government is doing enough to restore electricity and access to food and water in Puerto Rico or not, a majority of the public (59%) says the federal government is not doing enough, up from 52 percent in October. Most Democrats (86%) and independents (59%) say the federal government is not doing enough, but most Republicans (63%) say it is doing enough.
In contrast, Americans see the recovery efforts in Texas following Hurricane Harvey in late August progressing more positively. Most (60%) of the public says Texans are getting the help they need, twice the share (31%) who say Texans aren’t yet getting needed help.
The poll finds similar shares of Americans they are closely following news about recovery efforts in Puerto Rico (63%) and in Texas (58%). Democrats are somewhat more likely to report closely following news about the Puerto Rico recovery (75%) than are independents (61%) and Republicans (54%). In contrast, there are no partisan differences for those following news about Texas.
Designed and analyzed by public opinion researchers at the Kaiser Family Foundation, the poll was conducted from November 8 – 13, 2017 among a nationally representative random digit dial telephone sample of 1,201 adults. Interviews were conducted in English and Spanish by landline (415) and cell phone (786). The margin of sampling error is plus or minus 3 percentage points for the full sample. For results based on subgroups, the margin of sampling error may be higher.
You can read the original article here.
Source:
Kaiser Family Foundation (20 November 2017). "Two Months After Hurricane Maria, A Growing Majority Of Americans Say Puerto Ricans are Not Yet Getting the Help They Need" [Web blog post]. Retrieved from address https://www.kff.org/other/press-release/poll-two-months-after-hurricane-maria-a-growing-majority-of-americans-say-puerto-ricans-are-not-ye-getting-the-help-they-need/
SaveSave
Data transparency, debt consolidation and ID protection lead open enrollment wish list
In the thick of open enrollment season, savvy employers and benefit advisers have eased the onslaught of information with complex benefit jargon by spreading out employee sign-up before the mad fall rush. Employee Benefit Adviser spoke with Jeffrey Faber, HUB International Midwest’s chief operating officer, to discuss how employers are urging employees to save with data transparency tools, use interactive services to learn about new benefits and to sign up for identity protection.
EBA: How is open enrollment going for you and your clients?
Faber: We’re in the middle of open enrollment season and we are trying to lock down the last-minute decisions our clients have. Predominantly our business is a renewal business.
Our large groups have made their decisions already but our smaller groups are just finding out what their renewals are from the major medical carriers. We have our hands full trying to make sense of it all. But open enrollment is the focus. This is absolutely our busiest time of year. From mid-August to Halloween, and even mid-November, it seems to be getting longer and longer every year with all the nuances our clients require.
EBA: How does this enrollment season differ from previous years? Is there confusion over the ACA’s status? Is there a greater emphasis on voluntary benefits?
Faber: On the repeal of Obamacare, a lot of those decisions have been made too late for our employers to really have to pivot and they are unaffected largely by the executive orders and the talk from Congress. Of course, there's the specter that Congress will act and make a decision in the next couple of weeks, but that impact would probably be a 2019 event instead of a 2018 event.
On the voluntary benefits side, our clients are asking for financial and holistic tools to meet the employees where they live in regard to student loans, tuition assistance and debt consolidation services. ID theft has been a big conversation point in the last three or four months and has been heightened by the Equifax breach, but it started three years ago with the Target breach. A lot of employers want to understand their role in their employee’s lives,

And for voluntary benefits, most of our customers are moving to the consumer-driven model with higher deductibles, so accident insurance, critical injury insurance, and hospitalization – those are all nice bolt-on benefits for the medical benefits they have. It almost allows the employee to self-insure their own health. And HSAs and HRAs are still popular. We see a large uptick year over year over year.
EBA: Any other trends for this year’s open enrollment?
Faber: A few years ago, we joked that overall enrollment was the HR Super Bowl. It happened once a year, it was a three hour event with a bunch of commercials and no one really talked about it a week or two later.
Our clients have asked, what can we do the other 11 months a year? We have seen an increase in requests for interactive PDFs, on-demand video, and interactive guides directing folks to microsites or apps on their phone. We introduce these in April, May or June and if the employee needs this, they don't have to go back into their memory bank and access it, they can get it online. It is that year round learning that engages the customer.
EBA: Is this because employees are bombarded with information during open enrollment?
Faber: Yes and no. There is a lot of information that is required and that is distributed this time of year and there are a lot of decision points that they have to make for themselves and the benefit of their families. We put in place decision helping tools like Jellyvision’s ALEX and some other proprietary tools, that can help employees better make decisions.
But I think it is more toward trying to be a circuit breaker in an employee's head when they are accessing healthcare. That makes them stop and check, “Is this in network, do I have to get pre-authorization? How do I check for a lower cost across the street from a benefit provider?”
These things come out of the workshops this time of year, but if you are not hitting employees where they live at the time of use, you are missing those opportunities for significant cost savings. And not on just on the employer side but the employee side especially with high-deductible plans.
EBA: Is data transparency a big push for this open enrollment season?
Faber: Yes, especially when you consider that standalone imaging facilities are three to eight times less expensive than an in-house hospital facility. Employees need to understand that they will pay 100% of that cost until they meet that deductible in that consumer-driven plan, so there is every effort being made to make sure the employee is checking those transparency tools.
At open enrolment time, we make every effort to employees in the room to ID the nearest urgent care and ER facility, to write those down on a note card and put it in the visor of their car. So, they know at the moment of crisis to know where those places are and make decisions ahead of time.
EBA: Accountants say that from January to April 15, they don't see their families. Is it the same for you during open enrollment?
Faber: (Laughs) I grew up in an accounting family and I can attest to that. It is all hands on deck but our goal is to help clients get their decisions out of the way in Q1 and Q2. We try to help them with decisions that don't require immediacy and don’t have to be made right away, like life and disability insurance, and voluntary and wellness benefits. You can make a lot of those decisions in April, May and June.
Source:
Albinus P. (30 October 2017). "Data transparency, debt consolidation and ID protection lead open enrollment wish list" [Web blog post]. Retrieved from address https://www.employeebenefitadviser.com/news/data-transparency-debt-consolidation-and-id-protection-lead-open-enrollment-wish-list-says-hub-international-midwest-coo-jeffrey-faber?feed=00000152-1387-d1cc-a5fa-7fffaf8f0000
SaveSave
SaveSaveSaveSave
Understanding your Letter 226-J
Letter 226-J is the initial letter issued to Applicable Large Employers (ALEs) to notify them that they may be liable for an Employer Shared Responsibility Payment (ESRP). The determination of whether an ALE may be liable for an ESRP and the amount of the proposed ESRP in Letter 226-J are based on information from Forms 1094-C and 1095-C filed by the ALE and the individual income tax returns filed by the ALE’s employees.
What you need to do
- Read your letter and attachments carefully. These documents explain the ESRP process and how the information received affects the computation.
- The letter fully explains the steps to take if you agree or disagree with the proposed ESRP computation.
- Complete the response form (Form 14764) indicating your agreement or disagreement with the letter.
- If you disagree with the proposed ESRP liability, you must provide a full explanation of your disagreement and/or indicate changes needed on Form 14765 (PTC Listing). Return all documents as instructed in the letter by the response date.
- If you agree with the proposed ESRP liability, follow the instructions to sign the response form and return with full payment in the envelope provided.
You may want to
- Review the information reported on Forms 1094-C and 1095-C for the applicable year to confirm that the information filed with the IRS was accurate because the IRS uses that information to compute the ESRP.
- Keep a copy of the letter and any documents you submit.
- Contact us using the information provided in the letter if you have any questions or need additional time to respond.
- Send us a Form 2848 (Power of Attorney and Declaration of Representative) to allow someone to contact us on your behalf. Note that the Form 2848 must state specifically the year and that it is for the Section 4980H Shared Responsibility Payment.
Answers to Common Questions
Why did I receive this letter?
The IRS used the information you provided on Forms 1094/5-C and determined that you are potentially liable for an ESRP.
Where did the IRS get the information used to compute the ESRP?
The IRS used form 1094/5-C filed by the ALE and the individual income tax returns of your full-time employees to identify if they were allowed a premium tax credit.
Is this letter a bill?
No, the letter is the initial proposal of the ESRP
What do I need to do?
Review the letter and attachments carefully and complete the response form by the date provided.
What do I do if the information is wrong or I disagree?
Follow the instructions in the letter to provide corrected information for consideration by the IRS. The IRS will reply with an acknowledgement letter informing you of their final determination.
Do I have appeal rights?
Yes, the acknowledgement letter that you receive will spell out all your rights, including your right to appeal.
General Information
For more info visit ACA information center for Applicable Large Employers
Here’s an excerpt from the 226J letter, and a link to the official sample.
Source:
IRS (9 November 2017). "Understanding your Letter 226-J" [Web blog post]. Retrieved from address https://www.irs.gov/individuals/understanding-your-letter-226-j
The Latest: House passes sweeping GOP tax overhaul
WASHINGTON (AP) — The Latest on House consideration of the tax overhaul (all times local):
1:50 p.m.
The House has passed a sweeping Republican tax bill cutting taxes for corporations and many people. It puts GOP leaders closer to delivering to President Donald Trump a crucial legislative achievement after nearly a year of failures.
The House voted 227-205 along party lines to approve the bill, which would bring the biggest revamp of the U.S. tax system in three decades.
Most of the House bill’s reductions would go to business. Both the Senate and House would slash the 35 percent corporate tax rate to 20 percent and reduce levies on millions of partnerships and certain corporations, including many small businesses.
Personal income tax rates for many would be reduced through some deductions, and credits would be reduced or eliminated. But projected federal deficits would grow by $1.5 trillion over the coming decade.

___
12:15 p.m.
Democrats are using new projections by Congress’ nonpartisan tax analysts to call the Senate Republican tax bill a boon to the wealthy that boosts middle-income families’ taxes.
The Joint Committee on Taxation estimated that starting in 2021, many families earning less than $30,000 would have tax increases under the bill. By 2027, families earning up to $75,000 would face higher levies, while those earning more would get tax cuts.
Republicans say the new calculations reflect two provisions in the bill.
The Senate measure ends personal income tax cuts beginning in 2026 because Republicans needed to reduce the bill’s costs to obey the chamber’s budget rules.
It also abolishes the requirement under former President Barack Obama’s health care law that people buy insurance. That means fewer people getting federally subsidized coverage — which analysts consider a tax boost.
___
11:35 a.m.
President Donald Trump has arrived at the Capitol to encourage House Republicans who are about to push a $1.5 trillion tax package through their chamber.
The closed-door meeting comes as GOP leaders hope that by Christmas, they will give Trump and themselves their first legislative triumph this year.
House approval was expected later Thursday of the plan to slash corporate tax rates and reduce personal income tax rates while eliminating some deductions and credits.
The Senate Finance Committee is aiming to pass its separate version by week’s end. But some GOP senators want changes.
Republicans say the final measure will bestow lower levies on millions of Americans and spur economic growth by reducing business taxes. Democrats say the measure is disproportionately tilted toward corporations and the wealthy.
___
10:45 a.m.
Republicans drove a $1.5 trillion tax overhaul toward House passage Thursday. But Senate GOP dissenters also emerged in a sign that party leaders have problems to resolve before Congress can give President Donald Trump his first legislative triumph.
Trump was heading to the Capitol for a pep rally with House Republicans, shortly before the chamber was expected to approve the measure over solid Democratic opposition. There were just a handful of GOP opponents in the House, unhappy because the measure sharply curbs deductions for state and local taxes, but all agreed that passage seemed certain.
Like a similar package nearing approval by the GOP-led Senate Finance Committee, most of the House measure’s reductions would go to business. Personal income tax rates for many would be reduced, but some deductions and credits would be reduced or eliminated. Federal deficits would grow by $1.5 trillion over the coming decade.
U.S. President Donald Trump has arrived at the Capitol to encourage House Republicans who are about to push a $1.5 trillion tax package through their chamber. (Nov. 16)
You can read the original article here.
Source:
Associate Press (16 November 2017). "The Latest: House passes sweeping GOP tax overhaul" [Web blog post]. Retrieved from address https://apnews.com/b3297c1e443b40049beebcd832aaadc8?utm_campaign=SocialFlow&utm_source=Twitter&utm_medium=AP
SaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSaveSave
Trump picks former Lilly drug executive as health secretary
We're sure you've seen it trending. Here is the latest on Alex Azar of Eli Lilly & Co - President Trump's nominee for head of the Department of Health and Human Services.
(Bloomberg) – President Donald Trump named former Eli Lilly & Co. executive Alex Azar to lead the Department of Health and Human Services after agency’s past chief resigned amid blowback over his taxpayer-funded private jet travel.
“Happy to announce, I am nominating Alex Azar to be the next HHS Secretary. He will be a star for better healthcare and lower drug prices!” Trump tweeted Monday.
If confirmed, Azar will take over the administration’s management of the Affordable Care Act. Trump and Congressional Republicans have called to repeal the health law, and the administration has taken steps to destabilize it, such as cutting funding for some programs and refusing to pay subsidies to health insurers. He’ll also be a key figure on drug costs.

Bloomberg/file photo
Trump has been highly critical of the drug industry, saying that pharmaceutical companies are “getting away with murder” and threatening to use the federal government’s buying power to bring down prices.
Drug Costs
However he’s taken no concrete action yet to do much on prices, and the former drug executive’s appointment may continue the trend of strong talk but little action, said Spencer Perlman, director of health-care research at Veda Partners, a policy analysis firm.
“It is very unlikely the administration will take aggressive regulatory actions to control prescription drug prices,” Perlman said in a note to clients Monday. “The administration’s tepid response to drug pricing has not matched the president’s heated rhetoric.”
Dan Mendelson, president of Avalere Health, a consulting firm, also didn’t think Azar represented a change in direction on pharmaceutical policy. “His appointment will not change the president’s rhetoric,” Mendelson said in a phone interview.
Before his time at Lilly, Azar served as deputy secretary at HHS under President George W. Bush. One former Obama administration official said that experience could help him at the agency.
“While we certainly differ in a number of important policy areas, I have reason to hope he would make a good HHS secretary,” said Andy Slavitt, who ran the Centers for Medicare and Medicaid Services under the last administration and who has been a frequent critic of efforts to derail Obamacare. Slavitt said he hoped Azar would “avoid repeating this mistakes of his predecessor over-politicizing Americans’ access to health care.”
Running Obamacare
Azar, who ran Indianapolis-based Lilly’s U.S. operations until earlier this year, has been an advocate for more state flexibility under Obamacare. That matches up with what Republicans have pushed for, such as in a seemingly stalled bipartisan bill to fund insurer subsidies that help lower-income people with health costs.
As secretary, Azar would have broad authority over the program.
“I’m not one to say many good things about Obamacare, but one of the nice things in it is it does give a tremendous amount authority to the secretary,” Azar said during an interview with Bloomberg TV in June. “There are still changes that can be made to make it work a little better than it has been.”
There are signs that the law is gaining popular support despite the repeal efforts. In recent state elections in Virginia, Democrats won a competitive governors race that saw health care emerge as a top issue. In Maine, residents voted to expand Medicaid under the Affordable Care Act. Early enrollment in Obamacare plans earlier this month was also up considerably compared to last year.
Trump’s first HHS secretary, Tom Price, resigned in September after his extensive use of private and military jets at taxpayer expense was revealed. Azar must be approved by the Senate.
Senate Confirmation
Senator Orrin Hatch, who heads the Senate Finance Committee that will review Azar’s nomination, called on Trump’s pick to help “right the wrongs of this deeply flawed law.”
“For too long, hardworking, middle-class families have been forced to bear the brunt of Obamacare’s failures in the form of higher premiums and fewer choices,” Hatch said in a statement.
Ron Wyden, the senior Democrat on the panel, said he would closely scrutinize Azar’s record.
“At every turn, the president has broken his promises to American families to lower health care costs, expand access, and bring down the high price of prescription drugs,” Wyden said in a statement.
Azar left Lilly in January, several months after another senior executive was named to succeed then-CEO John Lechleiter. A lawyer by training, Azar previously clerked for Antonin Scalia on the Supreme Court.
You can read the original article here.
Source:
Employee Benefit Advisors (13 November 2017). "Trump picks former Lilly drug executive as health secretary" [Web blog post]. Retrieved from address https://www.employeebenefitadviser.com/articles/trump-picks-former-lilly-drug-executive-as-health-secretary?tag=00000151-16d0-def7-a1db-97f024b50000
SaveSave
SaveSave
SaveSave
IRS to reject returns lacking health coverage disclosure
Where does the IRS stand on ACA (Affordable Care Act)? It's time to know. Check out this article from Benefits Pro for more information.
The Internal Revenue Service has announced that for the first time, tax returns filed electronically in 2018 will be rejected if they do not contain the information about whether the filer has coverage, including whether the filer is exempt from the individual mandate or will pay the tax penalty imposed by the law on those who don’t buy coverage.
Tax returns filed on paper could have processing suspended and thus any possible refund delayed.
The New York Times reports that the IRS appears to be acting in contradiction to the first executive order issued by the Trump White House on inauguration day, in which Trump instructed agencies to “scale back” enforcement of regulations governing the ACA.
The move by the IRS reminds people that they can’t just ignore the ACA, despite the EO. Although only those lacking coverage have to pay the penalty, everyone has to indicate their insurance coverage status on their filing.
While the uninsured rate for all Americans dipped to a historic low of 8.6 percent in the first three months...5 states with lowest, highest uninsured rates
According to legal experts cited in the report, the IRS is indicating that although the administration may have leeway in how aggressively it enforces the mandate provision, it’s still in effect unless and until Congress specifically repeals it.
While many people thought they didn’t have to bother with reporting, and many insurers have raised rates anticipating that the lack of a mandate would lead to lower enrollments and higher costs for them, that’s not the case. Initially the IRS did not reject returns because the law was new.
The penalty is pretty steep; for those who don’t have coverage, it can range from $695 for an individual to a maximum of $2,085 for a family or 2.5 percent of AGI, whichever is higher. Not everyone without coverage would be penalized, though; if their income is too low or if the lowest-priced coverage costs more than 8.16 percent of their income, they’ll avoid the penalty.
That said, it’s not known how stringently the IRS will be in enforcing the mandate. But at least taxpayers will know whether they’re exempt from the penalty or whether they’re obligated to buy coverage.