Are Your Workers Sleeping on the Job?
A recent survey by Accountemps revealed that approximately three-quarters of American adults surveyed reported feeling tired at work often. Consistent tiredness can be a big risk for companies even if employees aren’t actually falling asleep on the job. Continue reading to learn more.
The occasional Monday-morning yawn is a common sight at most offices—but, according to new research, a staggering number of employees report being tired at work. Even if workers aren’t actually sleeping on the job, consistent tiredness could spell big trouble for productivity and retention.
Staffing firm Accountemps surveyed 2,800 American adults working in office environments, finding that nearly three-quarters report being tired at work often (specifically, 31 percent said very often, and 43 perfect reported feeling tired somewhat often). Twenty-four percent said it’s not very often that they’re yawning on the job, while just 2 percent said they never feel tired at work.
The report also ranked the top 15 “sleepiest” cities based on survey responses, with Nashville, Tenn. claiming the No. 1 spot, followed by a three-way tie between Denver, Indianapolis and Austin, Texas.
Michael Steinitz, executive director of Accountemps, noted that on-the-job errors would naturally follow if you have a workforce of tired employees. And, he says, “Consider the underlying causes of why employees are sleepy: If it’s because they’re stretched too thin, retention issues could soon follow.”
Those ideas are bolstered by research from Hult International Business School, which found that the 1,000 workers in its study average about 6.5 hours of sleep per night, lower than the seven to eight hours recommended by the American Academy of Sleep Medicine. Even a half-hour less than the optimal sleep time, researchers found, led to poorer workplace performance. Tired workers reported a lack of focus, needing more time to complete tasks, struggling with creativity, lacking motivation to learn and challenges to multitasking. Many of those side effects of being tired at work, the researchers wrote, are often mistakenly attributed to poor training or work culture when, in reality, they may stem from sleeplessness.
Lack of sleep has a well-documented impact on physical health, and Hult also noted its effects on mental wellness. A vast majority of respondents (84 percent) said they feel irritable at work when they’re tired, and more than half reported feelings of frustration and stress—all of which, researchers noted, can impact teamwork and collaboration.
Accountemps suggested a number of ways employees can guard against being tired at work: physical exercise, being more communicative with managers and leaving work at the office, such as by not bringing a phone or laptop to bed to decrease the chances of letting work communications keep them up at night. On the employer side, the firm recommended managers set reasonable office hours, increase face-to-face meetings with subordinates to see where support is needed and encourage workers to unplug when they leave the office.
SOURCE: Colletta, J. (26 October 2018) "Are Your Workers Sleeping on the Job?" (Web Blog Post). Retrieved from https://hrexecutive.com/are-your-workers-sleeping-on-the-job/
Healthcare waste is costing billions — and employers aren’t doing anything about it
Providing your employees with healthcare insurance is expensive. A large chunk of healthcare costs is being wasted by the healthcare industry, according to a new survey. Read on to learn more.
Providing the workforce with healthcare coverage is expensive, but a new survey of 126 employers suggests a large chunk of that cost is being wasted by the healthcare industry on treatments patients don’t need.
The healthcare industry wastes $750 billion per year on unnecessary tests and treatments, according to a survey from the National Alliance of Healthcare Purchaser Coalitions and Benfield, a market research, strategy and communications consulting firm. Some 60% of employers don’t take steps to manage their healthcare plan’s wasteful spending, despite the fact that the same percentage of employers view it as a problem, the survey says.
“While waste has long been identified as a key concern and cost contributor, employers are operating blind and need to look at a more disciplined approach to address top drivers that influence waste,” says Michael Thompson, National Alliance president and CEO.

Employers are under the impression that prescription drugs are the culprit behind the spending waste, and they are, just not as much as other services. Around 54% of health spending waste is caused by unnecessary medical imaging tests, such as MRIs and X-rays, the survey says. Specialty drugs, unnecessary lab tests and specialists referrals are also major money pits.
However, the survey data isn’t suggesting these procedures and treatments shouldn’t be covered by employer health plans. The tests and treatments are potentially life-saving, they’re just used more than they should be. Sometimes previous test results can help with a current diagnosis, but medical staff don’t always check patient files before ordering new tests.
Most employers don’t monitor unnecessary healthcare spending. The 34% of employers who do rely entirely on their healthcare vendors to do it for them, trusting that it’s being taken care of.
“The idea of reducing waste in the healthcare system can be overwhelming,” says Laura Rudder Huff, senior consultant for Benfield. “While employers ask themselves: ‘Where to start?’ this is an issue where even small steps matter. Employers can begin by collecting data to identify where the inefficiencies are in their workforce and community and use assets such as vendors and organizations like coalitions to realize market improvements.”
The survey also recommends employers enlist the services of Choosing Wisely, an organization that counsels patients and employers on healthcare plans and medical treatments.
This article originally appeared in Employee Benefit Adviser.
SOURCE: Webster, K. (7 November 2018) "Healthcare waste is costing billions — and employers aren’t doing anything about it" (Web Blog Post). Retrieved from https://www.benefitnews.com/news/healthcare-waste-is-costing-billions-and-employers-arent-doing-anything-about-it
HR’s recurring headache: Convincing employees to get a flu shot
According to The National Institute for Occupational Safety and Health, the flu cost U.S. companies billions of dollars in medical fees and lost earnings. Read this blog post to learn how HR departments are convincing their employees to get a flu shot.
Elizabeth Frenzel and her team are the Ford assembly line of flu shots: They can administer about 1,800 flu shots in four hours.
Frenzel is the director of employee health and wellbeing at the University of Texas MD Anderson Cancer Center, and with 20,000 employees, she is no stranger to spearheading large flu shot programs. The center where Frenzel administers flu shots has roughly a 96% employee vaccination rate. Back in 2006, only about 56% of employees got their shots.
“When you run these large clinics, safety is critically important,” she says.
Problems like Frenzel’s are not unique. Every fall, HR departments send mass emails encouraging employees to get vaccinated. The flu affects workforces across the country, costing U.S. companies billions of dollars in medical fees and lost earnings, according toThe National Institute for Occupational Safety and Health. It is not only a cause of absenteeism but a sick employee can put their coworkers at risk. Last year the flu killed roughly 80,000 people, according to the Centers for Disease Control.
Even if an employer offers a flu shot benefit, the push to get employees to sign up for the vaccine can be a two-month slough, with reminder emails going unanswered. Moreover, companies often contend with misconceptions about the shot, such as the popular fallacy that shots will make you sick, running out of the vaccine, and sometimes just plain employee laziness.
In Frenzel’s case, increasing the number of employees who got flu shots weren’t just a good idea, but it was needed to protect the lives of the cancer patients they interact with every day. The most startling fact, she says, was that healthcare workers who interact with patients daily were less likely to get vaccinated.
“So that’s how we started down the path,” she says. “Really targeting these people who had the closest patient contact.”
Frenzel credits the significant increase in employee participation in the flu shot program to several factors. They made the program mandatory — a common move in the healthcare industry — but Frenzel says their improvement also was related to flu shot education. The center made it a priority to explain to staff members exactly why they should get vaccinated. Frenzel made it more convenient, offering the vaccine at different hours of the day, so all employees could fit it into their schedule. They also made it fun, offering stickers for employees to put on their badge once they got a shot. Every year, she says, they pick a new color.
Employers outside of the medical industry are focused on improving their flu shot programs, including Edward Yost, manager of employee relations and development at the Society for Human Resource Management, who helped organize a health fair and flu shot program for 380 employees.
Yost says onsite flu shot programs are more effective than vouchers that allow employees to get vaccinated at a primary care doctor or pharmacy. The more convenient you make the program, he says, the more likely employees will use it.
“There’s no guarantee that those vouchers are going to be used,” he says. “Most people aren’t running out to a Walgreens or a CVS saying, please stab me in the arm.”
Besides the convenience, employees are more likely to sign up for a shot when they see co-workers getting vaccinated, Yost says. If a company decides to offer an onsite program, planning ahead is key. Sometimes employees will not sign up in advance for the vaccine but then decide they want to get one once the vendor arrives onsite. Yost recommends companies order extra vaccines.
“Make sure that you’re building in the expectation that there's going to be at least a handful of folks who are more or less what you call walk-ins in that circumstance,” he says.
Incentivizing employees to get the flu shot is also important, Yost says. Some firms will offer a gym membership or discounted medical premiums if they attend regular checkups and get a biometric screening in addition to a flu shot. He recommends explaining to employees how a vaccine can help reduce the number of sick days they may use.
“Employees need to see that there’s something in it for them,” Yost says. “And quite honestly, being sick is a miserable thing to experience.”
Affiliated Physicians is one of the vendors that can come in and administer flu shots in the office. The company has provided various employers with vaccines for more than 30 years, including SourceMedia, the parent company of Employee Benefit News andEmployee Benefit Adviser. In the past 15 years, Ari Cukier, chief operating officer of the company, says there’s been an increase in the amount of smaller companies signing up for onsite vaccines. HR executives should be aware of the number of employees signing up for vaccinations when scheduling an onsite visit.
“We can’t go onsite for five shots, but 20-25 shots and up, we’ll go,” Cukier says.
Cukier agrees communication between human resources departments and employees is crucial in getting people to sign up for shots. Over the years, he’s noticed that more people tend to sign up for shots based on the severity of the previous flu season.
“Last year, as bad as it was, we have seen a higher participation this year,” he says.
Brett Perkison, assistant professor of occupational medicine at the University of Texas School of Public Health in Houston, says providing a good flu shot program starts from the top down. The company executives, including the CEO and HR executives, should set an example by getting and promoting the shots themselves, he says.
It’s also important to listen to employee concerns. Before implementing a program, if workers are taking issue with the shot, it’s best to hold focus groups to alleviate any worries before the shots are even being administered, he says.
Some employees may even believe misconceptions like the flu shot will make one sick or lead to long-term illnesses, he says. Others may question the effectiveness of the shot. Having open lines of communication with employees to address these concerns will ensure that more will sign up, Perkison says.
Regardless of the type of flu shot program, the most important part is preventing illness, SHRM’s Yost says. While missing work and losing money are important consequences of a flu outbreak, having long-term health issues is even more serious, he says. Plus, no one likes being sick.
“Who’s going to argue about that?” he says.
This article originally appeared in Employee Benefit News.
SOURCE: Hroncich, C (24 October 2018) "HR’s recurring headache: Convincing employees to get a flu shot" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/news/hrs-recurring-headache-convincing-employees-to-get-a-flu-shot
Ready for the sounds of office sniffles?
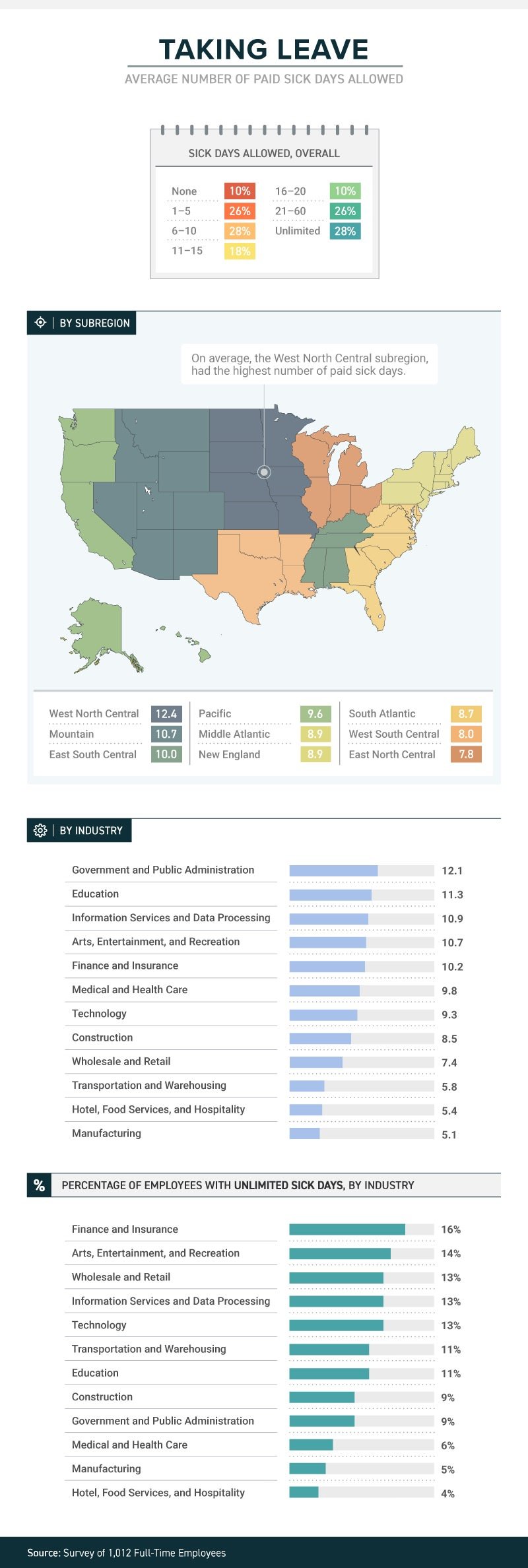
A recent study by law firm, Farah and Farah, states that one in four full-time workers receive between 1 and 5 sick days. Continue reading to learn more.
It’s not just a matter of whether they feel well enough to work, or whether they have sick days. The boss’s attitude about whether workers should take sick days or not can determine whether they actually do stay home when they’re sick, or instead come to work to spread their germs to all and sundry.
A new study from law firm Farah & Farah finds that even though it can take a person some 10 days to fully recover from a cold, approximately 10 percent of full-time workers in the U.S. get no sick days at all (part-timers don’t usually get them either), while more than 1 in 4 have to make do with between 1 and 5 sick days. Just 18 percent get enough sick time to actually recover from that cold—between 11 and 15 days.
The amount (or presence) of sick time varies from industry to industry, with government and public administration providing the most (an average of 12.1) and both hotel, food services and hospitality and manufacturing providing the least (an average of 5.4 for the hospitality industry and 5.1 for manufacturing). Some lucky souls actually get unlimited sick days, although even then they don’t always use them.
Regardless of industry, or quantity, just because workers get sick days it doesn’t mean they use them. Workers often worry that they’ll be discouraged from using them, with employers who may provide them but not encourage employees to stay home when ill. In fact, 38 percent of workers show up to work whether they’re contagious or not. Sadly for the people they encounter at work, the most likely to do so are in hospitality, medical and healthcare and transportation. Plenty of germ-spreading to be done in those professions!
And their employers’ attitudes play a role in how satisfied they are with their jobs. Among those who work for the 34 percent of bosses who encourage sick employees to stay home, 43 percent said they’re satisfied with their jobs in general. Among those who work for the 47 percent of bosses who are neutral about the use of sick days, that drops to 21 percent—and among the unfortunate workers who work for the 19 percent of bosses who actually discourage workers from staying home while ill, just 12 percent were satisfied with their jobs.
When it comes to mental health days (no, not that kind; the ones people really need to deal with diagnosed mental health conditions), fewer than 1 in 10 men and women were willing to call in sick. Taking “mental health days” when physically healthy, however, either to play hooky or simply have a vacation from the office, is something that 15 percent of respondents admitted to.
SOURCE: Satter, M (5 October 2018) "Ready for the sounds of office sniffles?" (Web Blog Post). Retrieved from https://www.benefitspro.com/2018/10/05/ready-for-the-sounds-of-office-sniffles/
Original report retrieved from https://farahandfarah.com/studies/sick-days-in-america
How employers can support employees during cancer treatment
Many people with cancer are choosing to continue working during their treatment. Read this blog post to learn how employers can support their employees during their cancer treatment.
Thanks to more sensitive diagnostic testing, earlier diagnosis and new treatments, the number of cancer survivors in the U.S. has grown to 15.5 million, and that number is projected to increase to 20.3 million by 2026. In addition, about 1.7 million Americans are projected to be diagnosed with cancer this year. A large percentage of these cancer patients and survivors are still active members of the workforce and the numbers have the potential to increase even more as people remain in the workforce beyond age 65.
Some people with cancer choose to continue working during treatment. Reasons for continuing to work can be psychological as well as financial. For some, their job or career is a big part of the foundation of their identity. A survey conducted by the non-profit Cancer and Careers found that 48% of those surveyed said they continued to work during treatment because they wanted to keep their lives as normal as possible, and 38% said they worked so that they felt productive. Being in the workforce also provides a connection to a supportive social system for many people and boosts their self-esteem and quality of life.
See also:
There also are financial benefits to the employer when employees continue to work during cancer treatment. Turnover costs, including hiring temporary employees and training replacement employees, are high. The cost of turnover for employees who earn $50,000 per year or less (which is approximately 75% of U.S. workers) average 20% of salary. For senior and executive level employees, that cost can reach 213% of salary. In addition, it can be costly to lose the experience, expertise, contacts and customer relationships employees have built.
This raises the question for employers: How can I support employees who choose to work while undergoing cancer treatment? Providing that support can be complex as employers work to balance their legal responsibilities under the Americans with Disabilities and Family and Medical Leave Acts with the privacy requirements of the Health Insurance Portability and Accountability Act (HIPAA).
When an employee chooses to share his or her diagnosis with a supervisor or HR representative, employers should view this disclosure as the beginning of a conversation with the employee taking the lead. (It’s up to the employee what information he or she wants to disclose about the diagnosis and treatment and with whom the information can be shared within the organization.) Here are four ways employers can support employees who are getting cancer treatment.
Help employees understand what benefits are available
The first step an employer should take is to refer the employee to the organization’s human resources manager (or someone who handles HR matters if the organization is smaller and does not have a human resources department) so that person can share information about all available benefits and pertinent policies. Provide details on:
- Medical and prescription drug coverages, including deductibles, co-pays, precertification requirements, network healthcare providers and plan and lifetime maximums
- Leave policies
- Flexible scheduling and remote work options, if available
- Employee assistance programs
- Community resources and support groups
See also:
Offer professional guidance
Offering patient navigator or case management services can also be beneficial. Navigators and case managers can provide a range of services including:
- Connecting employees with healthcare providers
- Arranging second opinions
- Providing evidence-based information on the type of cancer the employee has been diagnosed with and options for treatments
- Help filing health insurance claims, reviewing medical bills and handling medical paperwork
- Coordinating communication and medical records among members of the treatment team
- Attending appointments with employees
- Answering employee questions about treatments and managing side effects
Make accommodations
Workplace accommodations are another key pillar of support for employees working during cancer treatment. In addition to flexible scheduling, to accommodate medical appointments and help employees manage side effects like fatigue and nausea, and the option of working from home, workplace accommodations can include:
- Temporary assignment to a less physically taxing job
- Substituting video conferencing or online meetings for travel, which can be difficult for employees dealing with fatigue or a suppressed immune system, and can make it hard to attend needed medical appointments
- Leave sharing for employees who have used all their paid time off and can’t afford to take unpaid leave. Some organizations offer leave banks or pools where employees can “deposit” or donate some of their vacation days for employees dealing with a serious illness to use.
See also:
Employees may continue to need accommodations after treatment ends if they face late side effects such as fatigue, difficulty concentrating, numbness caused by nerve damage or heart or lung problems. Continuing job and schedule modifications can help mitigate the situation.
Ask for employee input
An often overlooked part of supporting employees who are working during cancer treatment is asking the employee what types of support he or she needs and prefers. Employees can share any medical restrictions related to their condition, what types of accommodations or equipment will help them do their job, and what schedule changes will allow them to attend needed appointments and recover from treatment. This should be an ongoing conversation because the employee’s needs are likely to change over the course of treatment and recovery.
SOURCE: Varn, M. (21 September 2018) "How employers can support employees during cancer treatment" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/how-employers-can-support-employees-during-cancer-treatment?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001
3 ways to promote inclusion in your workplace
Are you looking to grow your current inclusion practices or build new ones? Read this blog post to learn three ways employers can promote inclusion in their workplace.
Diversity and inclusion is top of mind for HR practitioners and employees alike. If we think about diversity as who is walking through the door, then inclusion would be the next part of the employee experience. With the recent focus on workplace diversity trends, it’s important to not forget how important it is to create an inclusive working environment.
It’s critical to facilitate relationship building with new hires and their teams. We often focus on the work to be done without taking time to get to know our co-workers as individuals. When we see each other as people and learn to appreciate our similarities and differences, it makes it easier for everyone to thrive.
Whether you’re looking to grow your current inclusion practices or are starting from scratch, try these three action items:
1. Don’t be afraid to ask.
It may sound simple, but a great first step to improving inclusion is to survey employees. By conducting quick and easy “pulse” surveys, you can gauge the level of belonging that employees feel. You can do this by launching survey focused on diversity or add questions around inclusion and belonging into your existing employee engagement surveys. Once you have a baseline on company sentiment, you can begin to improve areas that may be lacking. Start to put in place mechanisms to support individuals from different backgrounds and don’t forget to conduct these surveys on an ongoing basis.
2. New Hire Buddies
Whether you’re an introvert, extrovert, or somewhere in between, it can be hard to meet new people when you start a new job. Consider creating a “buddy” program to encourage new hires to bond with their co-workers. Companies hit roadblocks when they put the onus on new employees to reach out and engage with their teams. Having the support of a “buddy” at work helps create a feeling of security, which leads to greater engagement. The more engaged your employees are, the longer they will want to stay with your company.
3. Resource Groups
Employee resource groups (ERGs), sometimes also called affinity groups, serve as a platform that employees can use to build a culture of inclusion and belonging. Not only do they foster a sense of community within your organization, they also help new hires transition into their new working environment. These groups create opportunities for education and understanding between diverse individuals across your company. They can also be a great launchpad for new ideas and change in creating more inclusive policies and practices.
Fostering an inclusive company culture helps increase both engagement and retention. The better an employee feels about working at your organization, the greater the likelihood that they will reach their full potential on the job. Measure your current state of inclusion with regular pulse surveys and follow up with making changes as necessary to foster stronger relationships across the organization.
Source: Li, J. (19 July 2018). "3 ways to promote inclusion in your workplace" (Web Blog Post). Retrieved from https://blog.shrm.org/blog/3-ways-to-promote-inclusion-in-your-workplace
Point-of-sale wellness: How health plans are cashing in
Many health plans are starting to offer preventative approaches to help promote health and reduce skyrocketing healthcare costs. In this article, Vielehr talks about one approach, the point-of-sale wellness method.
Health care costs continue to skyrocket, and payers are constantly looking for ways to keep their populations healthier and to reduce these costs. Payers looking for more effective strategies to improve health and wellness for members should be aware of the new preventative approaches that more health plans are offering.
One such method that health plans are deploying to engage members is point-of-sale wellness, a type of incentive program that encourages members to actively make healthier purchases and lifestyle choices. As point-of-sale wellness becomes more prevalent among health plans, human resource managers and benefits brokers should understand how these programs work to best determine if they would be a valuable option for their employees and clients.
What is point-of-sale wellness?
Point-of-sale wellness is all about helping health plan members make smart, healthy purchasing decisions when they’re in a retail store or pharmacy. According to the Henry J. Kaiser Family Foundation, the average consumer visits their doctor 3.1 times per year. This same consumer will visit his or her favorite retailers multiple times per week. This presents the perfect opportunity for actionable engagement. It is often too easy for individuals to make impulsive decisions that favor cheaper care items or junk food that provides instant gratification but lead to an unhealthy lifestyle in the long run. Empowering consumers in these moments before checking out at the register with the understanding — and more importantly, the financial incentive — to make informed, smarter choices can lead to a healthier lifestyle and reduced health care costs. In short, the goal is to help individuals prioritize health and wellness at retail point of sale.
There are numerous ways that health plans can achieve this goal. One of the most common is by providing members with prepaid cards that are loaded with funds and discounts for the purchase of over-the-counter (OTC) items such as vitamins, diabetes care items and medications for allergies or cold and flu symptoms. The key component of these specialized prepaid cards is that they can be restricted-spend cards. In other words, they cannot be used to purchase any items that the health plan members want; they can only be used to purchase items off a curated list of products.
Under this arrangement, all parties, from the individual to the health plans and retailers, benefit. With a restricted-spend prepaid card in hand, an individual is rewarded for making purchases that contribute to a healthier lifestyle, while reducing health care costs both for themselves and the health plans administering the cards. In the meantime, the retailers partnering with the health plans to make point-of-sale wellness possible enjoy the opportunity to build long-term customer relationships with the health plan members using the cards.
Point-of-sale wellness in action
Point-of-sale wellness can be customized to be as general or specific as a health plan needs. For example, a health plan that supports a high number of new parents on a regular basis may offer a prepaid card designed specifically to assist members with newborn children. The first years of an infant’s life are among the most expensive from a health care perspective. More health plans are starting to offer new parents prepaid cards that are loaded with funds and discounts for items such as OTC medications, baby food and formula, diapers, strollers, car seats or thermometers. This opens an easier path for new parents to do basic at-home diagnostics and keep their babies’ health monitored so costly trips to an emergency room or urgent care center are not needed as often.
Payers that offer health and wellness programs to assist new parents in their populations can consider engaging health plans that offer these types of prepaid cards. Having a healthier child has the added benefit of reducing stress on the parents, which means they are in a better position to continue performing in the workplace.
Financial incentives for healthier choices
Most wellness programs are focused on informing participants of the best ways to support a healthier lifestyle, but that is only half of the equation. Point-of-sale wellness goes one step further to ensure participants are empowered from a financial perspective to make smarter purchasing decisions while shopping for daily care items. Businesses and benefits brokers who want to provide their employees and clients the best opportunities to live a healthier lifestyle should consider engaging health plans that prioritize these prepaid card incentives into their offerings.
Vielehr, D. (19 July 2018). "Point-of-sale wellness: How health plans are cashing in" (Web Blog Post). Retrieved from https://www.benefitspro.com/2018/07/19/point-of-sale-wellness-how-health-plans-are-cashin/
3 questions to ask about paid leave programs
Paid time off policies are offered by employers for numerous reasons, employee wellness being one of them. Continue reading to learn about the 3 key questions to ask about these programs and their costs.
Employers provide paid time away from work policies for a variety of reasons: to attract and retain talent (responding to employee needs and changing demographics); to be compliant with local, state and federal laws (which are proliferating); and to support general employee well-being (recognizing that time away from work improves productivity and engagement).
While offering paid absence policies delivers value to both employees and the employers, employers recognize the need to balance the amount of available time with the organization’s ability to deliver its products and services.
To help employers balance paid time away drivers, here are three key questions to ask to get a handle on the costs and benefits of paid leave.
1. Do you have a complete picture of the costs associated with your employees’ time away from work?
A challenge for many employers is getting a handle on the cost of time away from work and the related benefits. If an employer cannot quantify the costs of absence, it may not be able to define management strategies or to engage leadership to adopt new initiatives, policies or practices related to paid and unpaid time away programs.
Ninety percent of employers participating in the 2017 Aon Absence Pulse Survey reported they hadn’t yet quantified the cost of absence, and 43 percent of participants identified defining the cost of absence as a top challenge and priority. Though intuitively managers and executives recognize there is an impact when employees are absent from work, particularly when an absence is unscheduled, they struggle to develop concrete and focused strategies to address absence utilization without the ability to measure the current cost and collectively the impact of new management initiatives.
Employers struggle to quantify the cost of absence in the context of productivity loss, including replacement worker costs. According to the Bureau of Labor Statistics in 2017, employers’ cost of productivity loss associated with absenteeism was $225.8 billion, and 9.6 percent of compensation was spent on lost time benefits and overtime.
Employers are expanding their view of absence, recognizing that use of paid and unpaid time away programs are often associated with an employee’s health. As a result, combining data across health and absence programs allows an employer to recognize drivers of absence “work-related value” and define strategies to address not just how to manage the absence benefit, but to target engagement to improve well-being and the organization’s bottom-line.
As an example, musculoskeletal conditions are frequently associated with absence, which is not surprising when 11 percent of the workforce has back pain. It is noteworthy that of those with back pain, 34 percent are obese, 26 percent are hypertensive and 14 percent have mood disorders. The Integrated Benefits Institute reported in 2017 that back pain adds 2.5 days and $688 in wages to absence associated with this condition. It is this type of information pairing that provides employers with the insight to develop strategies to address comprehensive absence.
When absence and health costs are quantified, organizations quickly recognize the impact on the business’s bottom line. As the old saying goes, “we can only manage what we can measure.”
2. What is your talent strategy to improve work-life benefits, inclusive of time off to care for family?
The race for talent is on, and every industry recognizes the huge impact the changing workforce demographics currently has, and will continue to have. The current workforce incorporates five generations, though an Ernst and Young report from 2017 estimates that by 2025 millennials will make up 75 percent of the workforce. As a result, the work-life needs of millennials—and their perspectives around benefits—is driving change, including time away from work policies.
It is worth noting that, per a 2015 Ernst and Young survey, millennial households are two times more likely to have both spouses working. The Pew Research Center reported in 2013 that, among all workers, 47 percent of adults who have a parent 65 years or older are raising a minor child or supporting a grown child. Additionally, a 2016 report from the Center for Work Life Law at the University of California Hastings claimed that 50 percent of all employees expect to provide elder care in the next five years.
In response, employers are expanding paid time off programs for care of family members. The paid family leave continuum often begins with a paid parental policy providing time to bond with a new birth or adoption placement. An elder care policy may follow, and the culmination might be a family care policy covering events like those under the job-protected Family Medical Leave Act. An Aon SpecSelect Survey reported that 94 percent of employers offer some form of paid parental leave in 2017; this is a significant change from 2016 when 62 percent offered this benefit. Two weeks of 100 percent paid parental leave was the norm per Aon’s SpecSelect 2016 Survey, but we are finding that many employers are expanding these programs, offering between 4 to 12 weeks.
Offering paid leave programs on their own may meet immediate needs for both time and financial support, but may be incomplete to help the employee address the full spectrum of issues that could affect success at work. In combination with family care needs—even those associated with a happy event such as a birth—there may be other health, social or financial issues. Employers combining their paid leave programs with a broader well-being strategy deliver greater value, improve engagement and increase productivity.
3. If you’re a multi-state employer, how are you ensuring your sick and family leave policies are compliant across all relevant jurisdictions?
Paid leave is a hot legislative topic lately. Last December saw the enactment of a paid FMLA tax credit pilot program as part of the federal Tax Reform The paid sick leave law club now totals 42 states and myriad municipalities. Both Washington state and Washington, D.C. are ramping up to implement paid family leave laws in 2020, joining the four states and one city that already have some form of paid family or parental leave law.
How are multi-state employers keeping up with this high-stakes evolving environment? The 2017 Pulse Survey saw 70 percent of employers report they are aware they have an employee who is subject to a paid sick leave law. Ten percent of respondents said they did not know if they had anyone subject to such a law. If knowledge is the first step in the process of compliance, deciding on a compliance strategy and then successfully implementing it are surely steps two and three.
With respect to paid sick leave, there are three major compliance options: comply on a jurisdiction-by-jurisdiction level, with as many as 42 different designs and no design more generous than it has to be; comply on a national level with one, most generous design, or meet somewhere in the middle, perhaps with one design for each state where a state- or local-level law is in place, or by grouping jurisdictions with similar designs together to strike a balance between being overly generous and being bogged down by dozens of administrative schemes.
Data analytics can be a key driver in designing a successful compliance strategy—compare your employee census to locations with paid sick leave laws. The ability to track and report on available leave is a requirement in all jurisdictions, and at this point, few if any third-party vendors are administering multi-state paid sick leave.
For paid family leave, the primary policy design issue is how an employer’s FMLA, maternity leave and short-term disability benefits will interact with the various paid family leave laws. So, while there may be fewer employer choices to be made with statutory paid family leave, clear employee communications will be critical to success.
Employers may tackle time away from work program issues individually to meet an immediate need, or collectively as a comprehensive strategy. Such a strategy would include data analytics across health and lost-time programs, absence policies that meet today’s needs for the employer and employee, health and wellness programs targeting modifiable health behaviors, and absence program administration that is aligned to operational goals. The expected outcome for time away from work programs isn’t about the programs themselves: it is about an engaged, productive workforce who delivers superior products/services. How do your programs stack up?
SOURCE:
VanderWerf, S and Arnedt, R (13 July 2018) "3 questions to ask about paid leave programs" [Web Blog Post]. Retrieved from https://www.benefitspro.com/2018/07/05/3-questions-to-ask-about-paid-leave-programs/
How faking your feelings at work can be damaging
Putting up a fake smile on Monday morning is sometimes unavoidable. There could be consequences to carrying a heavy emotional labor load to get over the Monday Blues.
Imagine yourself 35,000 feet up, pushing a trolley down a narrow aisle surrounded by restless passengers. A toddler is blocking your path, his parents not immediately visible. A passenger is irritated that he can no longer pay cash for an in-flight meal, another is demanding to be allowed past to use the toilet. And your job is to meet all of their needs with the same show of friendly willingness.
For a cabin crew member, this is when emotional labour kicks in at work.
A term first coined by sociologist Arlie Hochschild, it’s the work we do to regulate our emotions to create “a publicly visible facial and bodily display within the workplace”.
Simply put, it is the effort that goes into expressing something we don’t genuinely feel. It can go both ways – expressing positivity we don’t feel or suppressing our negative emotions.
Unhelpful attitudes such as ‘I’m not good enough’ may lead to thinking patterns in the workplace such as ‘No-one else is working as hard as I seem to be’ or ‘I must do a perfect job’, and can initiate and maintain high levels of workplace anxiety - Leonard
Hochschild’s initial research focused on the airline industry, but it’s not just in-flight staff keeping up appearances. In fact, experts say emotional labour is a feature of nearly all occupations in which we interact with people, whether we work in a customer-facing role or not. The chances are, wherever you work, you spend a fair portion of your working day doing it.
When research into emotional labour first began, it focused on the service industry with the underlying presumption that the more client or customer interaction you had, the more emotional labour was needed.
However, more recently psychologists have expanded their focus to other professions and found burnout can relate more closely to how employees manage their emotions during interactions, rather than the volume of interactions themselves.
Perhaps this morning you turned to a colleague to convey interest in what they said, or had to work hard not to rise to criticism. It may have been that biting your lip rather than expressing feeling hurt was particularly demanding of your inner resource.
But in some cases maintaining the façade can become too much, and the toll is cumulative. Mira W, who preferred not to give her last name, recently left a job with a top airline based in the Middle East because she felt her mental wellbeing was at stake.
In her last position, the “customer was king”, she says. “I once got called 'whore' because a passenger didn't respond when I asked if he wanted coffee. I’d asked him twice and then moved to the next person. I got a tirade of abuse from the man.”
“When I explained what happened to my senior, I was told I must have said or done something to warrant this response… I was then told I should go and apologise.”
“Sometimes I would have to actively choose my facial expression, for example during severe turbulence or an aborted landing,” she says. “Projecting a calm demeanour is essential to keep others calm. So that aspect didn't worry me. It was more the feeling that I had no voice when treated unfairly or extremely rudely.”
During her time with the airline, she encountered abuse and sexism – and was expected to smile through it. “I was constantly having to hide how I felt.
Over the years and particularly in her last role, handling the stress caused by suppressing her emotions became much harder. Small things seemed huge, she dreaded going to work and her anxiety escalated.
“I felt angry all the time and as if I might lose control and hit someone or just explode and throw something at the next passenger to call me a swear word or touch me. So, I quit,” she says.
She is now seeing a therapist to deal with the emotional fallout. She attributes some of the problems to isolation from family and a brutal travel schedule, but has no doubt that if she hadn’t had to suppress her emotions so much, she might still be in the industry.
Mira is not alone. Across the globe, employees in many professions are expected to embrace a work culture that requires the outward display of particular emotions – these can including ambition, aggression and a hunger for success.
The way we handle emotional labour can be categorised in two ways – surface acting and deep acting
A few years ago, the New York Times wrote a “lengthy piece about the “Amazon Way”,describing very specific and exacting behaviour the retail company required of its employees and the effects, both positive and negative, that this had on some of them. While some appeared to thrive in the environment, others struggled with constant pressure to show the correct corporate face.
“How we cope with high levels of emotional labour likely has its origins in childhood experience, which shapes the attitudes we develop about ourselves, others and the world,” says clinical and occupational psychologist Lucy Leonard.
“Unhelpful attitudes such as ‘I’m not good enough’ may lead to thinking patterns in the workplace such as ‘No-one else is working as hard as I seem to be’ or ‘I must do a perfect job”, and can initiate and maintain high levels of workplace anxiety,” says Leonard.
Workers are often expected to provide good service to people expressing anger or anxiety – and may have to do this while feeling frustrated, worried or offended themselves.
“This continuous regulation of their own emotional expression can result in a reduced sense of self-worth and feeling disconnected from others,” she says.
Hochschild suggests that the way we handle emotional labour can be categorised in two ways – surface acting and deep acting – and that the option we choose can affect the toll it takes on us.
Take the example of a particularly tough phone call. If you are surface acting you respond to the caller by altering your outward expression, saying the appropriate things, listening while keeping your actual feelings entirely intact. With deep acting you make a deliberate effort to change your real feelings to tap in to what the person is saying – you may not agree with the manner of it but appreciate the aim.
Both could be thought of as just being polite but the latter approach – trying to emotionally connect with another person’s point of view – is associated with a lower risk of burnout.
Jennifer George’s role as a liaison nurse with a psychiatric specialism in the Accident & Emergency department at Kings College London Hospital puts her at the sharp end of health care. Every day she must determine patients’ needs – do they genuinely need to be admitted, just want to be looked after for a while or are they seeking access to drugs?
“It’s important to me that I test my own initial assumptions,” she says. “As far as I can, I tap into the story and really listen. It’s my job but it also reduces the stress I take on.”
“Sometimes I’ll have an instinctive sense that the person is trying to deceive, or I can become bored with what they’re saying. But I can’t sit there and dismiss something as fabrication and I don’t want to.”
This process can be upsetting, she says. Sometimes she has to say no “in a very direct way”, and the environment can be noisy and threatening. “I stay as much as I can true to myself and my beliefs. Even though I need to be open to what both fellow professionals and would-be and genuine patient cases say to me, I will not say anything I don’t believe and that I don’t believe to be right. And that helps me,” she says.
When things get tough, she talks to colleagues to unload. “It’s the saying it out loud that allows me to test and validate my own reaction. I can then go back to the person concerned,” she says.
Ruth Hargrove, a former trial lawyer based in California, also faces tricky interactions in her work representing San Diego students pro bono in disciplinary matters. “Pretty much everyone you are dealing with in the system can make you labour emotionally,” she says.
One problem, says Hargrove, is that some lawyers will launch personal attacks based on any perceived weakness – gender, youth – rather than focusing on the actual issues of the case.
“I have dealt with it catastrophically in the past and let it eat at my self-esteem,” she says. “But when I do it right, I realise that I can separate myself out from it and see that [their attack] is evidence of their weakness.”
Rather than refuting specific, personal allegations, she simply sends back a one-line email saying she disagrees. “Not rising to things is huge,” she says. “It’s a disinclination to engage in the emotional battle that someone else wants you to engage in. I keep in sight the real work that needs to be done.”
Those who report regularly having to display emotions at work that conflict with their own feelings are more likely to experience emotional exhaustion
Hargrove also has to deal with the expectations of clients who believe – sometimes unrealistically – that if they have been wronged, justice will prevail. She understands their feelings, even as she has to set them straight.
“I empathise here, as a parent, with their thought that there should be a remedy, even when I know it’s not going to be achievable. It helps me that this feeling is also true to me.”
Remaining true to your feelings appears to be key – numerous studies show those who report regularly having to display emotions at work that conflict with their own feelings are more likely to experience emotional exhaustion.
Of course, everybody needs to be professional at work and handling difficult clients and colleagues is often just part of the job. But what’s clear is that putting yourself in their shoes and trying to understand their position is ultimately of greater benefit to your own well-being than voicing sentiments that, deep down, you don’t believe.
Leonard says there are steps individuals and organisations can take to prevent burnout. Limiting overtime, taking regular breaks and tackling conflict with colleagues through the right channels early on can help, she says, as can staying healthy and having a fulfilling life outside work. A “climate of authenticity” at work can be beneficial.
“Organizations which allow people to take a break from high levels of emotional regulation and acknowledge their true feelings with understanding and non-judgemental colleagues behind the scenes tend to fare better in the face of these demands,” she says.
Such a climate can also foster better empathy, she adds, by allowing workers to maintain emotional separation from those with whom they must interact.
Where it is possible, workers should be truly empathetic, be aware of the impact the interaction is having on them and try to communicate in an authentic way. This, she says, can “protect you from communicating in a disingenuous manner and then feeling exhausted by your efforts and resentful of having to fake it”.
SOURCE:
Levy, K (25 June 2018) "How faking your feelings at work can be damaging" [Web Blog Post]. Retrieved from https://www.bbc.com/capital/story/20180619-why-suppressing-anger-at-work-is-bad
Top 10 health conditions costing employers the most
Conditions that impact plan costs can be problematic. Here is a look into the top 10 health conditions hitting the hardest on employers wallets.
As healthcare costs continue to rise, more employers are looking at ways to target those costs. One step they are taking is looking at what health conditions are hitting their pocketbooks the hardest.
“About half of employers use disease management programs to help manage the costs of these very expensive chronic conditions,” says Julie Stich, associate vice president of content at the International Foundation of Employee Benefits Plans. “In addition, about three in five employers use health screenings and health risk assessments to help employees identify and monitor these conditions so that they can be managed more effectively. Early identification helps the employer and the employee.”
What conditions are costly for employers to cover? In IFEPB’s Workplace Wellness Trends 2017 Survey, more than 500 employers were asked to select the top three conditions impacting plan costs. The following 10 topped the list.
10. High-risk pregnancy
Although high-risk pregnancies have seen a dip of 1% since 2015, they still bottom out the list in 2017; 5.6% of employers report these costs are a leading cost concern for health plans.
9. Smoking
Smoking has remained a consistent concern of employers over the last several years; 8.6% of employers report smoking has significant impact on health plans.
8. High cholesterol
While high cholesterol still has a major impact on health costs- 11.6% say it's a top cause of raising healthcare costs- that number is significantly lower from where it was in 2015 (19.3%).
7. Depression/ mental illness
For 13.9% of employers, mental health has a big influence on healthcare costs. This is down from 22.8% in 2015.
6. Hypertension/ high blood pressure
This is the first condition in IFEBP's report to have dropped a ranking in the last two years. In 2015, hypertension/ high blood pressure ranked 5th with 28.9% of employers reporting it is a high cost condition. In 2017, the condition dropped to 6th with 27.6% of employers noting high costs associated with the disease.
5. Heart disease
This year's study found that 28.4% of employers reported high costs associated with heart disease. In 2015, heart disease was the second highest cost driver with 37.1% of employers citing high costs from the disease.
4. Arthritis/back/musculoskeletal
Nearly three in 10 employers (28.9%) say these conditions are drivers of their health plan costs, compared to 34.5% in 2015.
3. Obesity
Obesity is still a top concern for employers, but slightly less so than it was two years ago. In 2017, 29% of employers found obesity to be a burden on health plans. In 2015, 32.45 cited obesity as a major cost driver.
2. Cancer (all kinds)
Cancer has become more expensive for employers. Now, 35.4% of employers report cancer increasing the costs of health plans, compared to 32% in 2015.
1. Diabetes
The king of raising health costs, diabetes has topped the list both in 2015 and 2017. In the most recent report, 44.3% of employers say diabetes is among the conditions impacting plan costs.
SOURCE:
Otto. N (18 June 2018) "Top 10 health conditions costing employers the most" [Web Blog Post]. Retrieved from https://www.employeebenefitadviser.com/slideshow/top-10-health-conditions-costing-employers-the-most