U.S. employers eye cutting wasteful drugs worth $6 billion
A group of researchers has found that there are medications that could be less expensive alternatives that could be covered by employers based on the benefits provided to employees. Read this blog post to learn more.
A health plan covering thousands of California teachers stopped paying for a diabetes drug that cost $352 per prescription. In its place, the plan now pays less than $13.
The difference? Instead of getting a 1,000-milligram dose of metformin, members got two 500-milligram pills.
It’s just one example of what some employers call “wasteful drugs,” and a coalition of West Coast employers says there are hundreds more. At a time when U.S. President Donald Trump is pushing to trim drug costs for Medicare by tying them to prices in other countries, the coalition is on a crusade to cut company spending on drugs nationwide by simply noting the cheaper choices already available, drawing the ire of drugmakers.
A guidebook produced by the Pacific Business Group on Health and researchers from Johns Hopkins University identifies 49 medications with less expensive alternatives that could be cut from the lists of drugs covered by employers. The group has pushed its approach to large employers for two years. Now it’s focusing on mid-sized companies at conferences, with webinars and through an online Excel sheet designed to help any company identify savings.
Lauren Vela, senior director of member value at the coalition, said it all comes down to who gains in the end. “There are so many folks making so much money on the existing system that the folks who really know how the system works don’t have an interest in changing it,” Vela said by telephone.
Vela presented at three online conferences this summer, and has at least two scheduled for the early fall, she said.
The medications outlined in the guidebook accounted for more than $6 billion in U.S. retail drug spending in 2019, according to data compiled by Bloomberg from Symphony Health. Drugmakers have long been under attack for how they price medications sold in the U.S., and for their efforts to undermine rules on when their products can be sold generically for less.
On Sunday, just weeks before the presidential election, Trump announced he had signed a presidential order on the “most favored nation” plan, which would try to link Medicare Part B and Part D prices to lower prices paid by other countries. In response, groups representing drugmakers said this could hurt their ability to find and test for new medications, while House Speaker Nancy Pelosi said Trump’s action took “no real action” to lower prices.
Researchers aligned with the Pacific Business Group, meanwhile, have analyzed six months of drug use and more than 2.5 million scripts for 15 large self-insured companies. They found that 6% of all claims were for what the report termed “wasteful drugs.”
In the case of just one, the leukemia drug Gleevec, use of generic imatinib could cut the average wholesale price 96%, a savings of $108.28 per pill, according to the report. The group says hundreds of other drugs could be replaced similarly.
“Generic drugs are an important part of the full spectrum of health-care solutions,” said Julie Masow, a spokeswoman for Novartis, the Swiss-based maker of Gleevec.
But the drug, which lost patent protection in the U.S. in 2016, “will remain on the U.S. market to maximize choice for health-care professionals and patients,” Masow said, “and Novartis plans to continue financial support for eligible patients.”
The Pacific Business Group also calls out therapies that combine two existing, cheaper pills into a more expensive single dose. And they urge removing pricey drugs that offer only small changes for the consumer, such as certain extended-release formulations or different dosage concentrations.
Drugmaker pushback
While the Pacific Business Group’s guidebook is gaining support among companies, PBMs — which administer drug plans — and pharmaceutical companies are pushing back.
Drugmakers are taking issue with characterizing drugs as “wasteful.”
“Decision-making power on what medicines patients should take should rest with doctors,” Katie Koziara, a spokeswoman for the Pharmaceutical Research and Manufacturers of America, said in an email.
Koziara said her group favors reforming the rebate system “to help correct PBMs and payers’ misaligned incentives,” boost transparency and share rebates directly with patients.
A trade group for PBMs, meanwhile, disputed the Pacific Business Group’s guidebook, saying it was based on limited data.
Greg Lopes, a spokesman for the Pharmaceutical Care Management Association, called the reports “dated” and said, “PBMs are the only entity in the supply chain reducing drug costs for consumers.”
Pharmacy benefit managers negotiate with drug manufacturers on behalf of employers, determining which drugs should be covered. But the employers say that the way PBMs’ services are sold makes it tough to tell whether they’re really saving money.
PBMs and consultants will typically present a spreadsheet that shows administrative fees, discount off-list prices, and rebate payments. The rebates flow from drugmakers to PBMs and ultimately back to plan sponsors, like employers or unions.
But Vela says employers often can’t easily tell if PBMs retain a portion of the rebates or other payments that incentivize them to keep expensive drugs on the formulary. “You’re hiring an entity to negotiate on your behalf, and the party with whom they’re negotiating is giving them money you don’t know about,” Vela said.
As the PBM business model has come under more scrutiny, benefit managers have pledged to be more transparent with rebates and pass them back to employers.
After recent mergers, the three largest PBMs are now part of companies that also own health insurers, pharmacies and other medical providers: UnitedHealth Group’s OptumRx; CVS Health Caremark; and Cigna Express Scripts.
None of the three leading PBMs would comment on the guidebook analysis.
The array of discounts and rebates PBMs tout to their clients often obscures the fact that employers are paying for high-priced drugs when lower-cost alternatives exist, according to Thomas Cordeiro, a co-author of the guidebook and president of consultant Integrity Pharmaceutical Advisors.
“Just because you have a high rebate doesn’t mean your cost is going to be low,” Cordeiro said.
SOURCE: Bloomberg News. (14 September 2020) "U.S. employers eye cutting wasteful drugs worth $6 billion" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/articles/u-s-employers-eye-cutting-wasteful-drugs-worth-6-billion
Improving your employee experience during open enrollment
Is your company open enrollment hosted on an online platform? Employers often struggle with employee participation during the open enrollment season. Hosting enrollments online is one way to increase employee participation this year. Read on for more tips to help ease this open enrollment season.d
For HR professionals, open enrollment is one of the most stressful and demanding times of the year. Many employers struggle with employee participation and expensive, time-consuming roll-outs. They also have to provide resources to help employees make the right plan selections for themselves and their families. As we head into another open enrollment season, consider these tips to ease the process.
Switch your open enrollments to online platforms.
If you’re still relying on paper enrollment forms, you are likely spending more money and time than you need to in pursuit of your manual work process and its many inconsistencies. Online platforms provide optimum efficiency, accuracy and convenience for your workforce, offering employee self-service options that encourage employees to take initiative in selecting the best plan for their situation. Not only will members of your workforce benefit from the convenience of being able to explore their options on their own time, but you’ll be able to offer them multi-lingual enrollment materials and have more time to assist them than ever before.
Prioritize and diversify communication.
One of the top ways to ensure a smooth open enrollment period is to use multiple communication channels, including frequent reminders regarding open enrollment deadlines. Without consistent outreach on the part of your HR officers and general managers, you will likely find yourself hunting people down to meet your enrollment and extension deadlines. Using an online self-service portal as well as traditional in-person meetings allow you to remind your employees of critical dates and changes as enrollment closes in.
The robust benefits administration system you choose should offer enrollment tracking and reporting features so you can see at a glance who still needs to begin open enrollment, who has left enrollment documents incomplete, who has made changes to their benefits (such as adding a dependent) and more. You can arrange for the system to send automatic reminders to signal the employee that further actions are needed. Providing multiple reminders will improve participation and the completion of on-time enrollments.
Help employees choose the best health plan for their situation.
In order to have the most successful open enrollment period possible, educating your employees on the different plan options available will go a long towards ensuring employee satisfaction. Studies have shown that most employees don’t have the necessary understanding of terms like “deductible” and “coinsurance,” let alone the tools to know which plan is best for their individual needs. Incorporating at-a-glance comparison tools and charts into your online or print enrollment materials can help employees make the most informed decision possible. It can also be helpful to provide educational materials like videos and simplified plan charts or cost calculators.
Keep Up with Benefit Trends and Voluntary Offerings.
Given the current labor shortage and competitive talent market, you’ll want to make sure your company is up to speed on which new benefits your competitors are looking to add, as well as which ones are appealing to specific roles, locations or generations within potential candidates from your hiring pool.
Voluntary benefits, for example, are playing an increasingly important role in employee benefits portfolios and they don’t cost you anything. Some of the most popular voluntary benefits right now include identity theft protection, pet insurance, long term care insurance and critical illness protection. If you aren’t currently offering these types of additional benefits, they could be a cost-effective way to boost employee morale, increase participation in enrollment and attract more workers to your business.
SOURCE: Smith, M. (2 December 2019) "Improving your employee experience during open enrollment" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/improving-your-employee-experience-during-open-enrollment
Key factors in choosing your benefits during open enrollment
Employers are now realizing that in order to attract and retain talent, they have to provide the best benefits. But, how do employees select the right benefits out of all the available options? Read the following blog post from Employee Benefit News for a few key factors to consider when choosing your benefits during open enrollment.
Even if you are a veteran in choosing employer-sponsored benefits, the landscape is shifting. Over the past years, we’ve seen changes to mental health counseling stipends, extended maternity/paternity leave and family building. Companies across industries are realizing that in order to attract and retain talent, they need to provide best in class benefits that save employers unforeseen costs in the long run, and shows employees that their employers are invested in their wellbeing — in and out of the office.
With all these available options and only a short window to select what’s right for you, here’s what should you look out for during open enrollment.
Which benefits matter to me?
The beauty of a diverse workforce is that employees may represent various walks of life. However, this means that not all benefits make sense for every person. Perhaps your boss is prioritizing childcare for his toddler while your colleague is looking to refinance student loans. Whatever your life circumstance, ask yourself, “Which benefits are most pertinent to my life and life goals in the coming year?”
For instance, fertility benefits may not be immediately attractive at first glance, even if you’re actively thinking about starting a family. But 1 in 8 couples will be impacted by infertility and treatment without coverage can be wildly expensive. It’s important to make sure you’re thinking critically and getting all the necessary information when browsing for your benefits. Rule of thumb: if this could impact you in the coming year, even if you’re not 100% sure, opt-in for coverage.
What’s actually covered?
During open enrollment, be sure to ask your benefits team about how robust each offering is and what’s included. A particular benefit may look like it has a lot to offer, but after further investigation, you may uncover restrictions, unforeseen out of pocket costs and other obstacles that may make it harder for you to utilize the benefit.
With fertility benefits, many conventional carriers offer coverage with a dollar maximum, meaning you’d max out on coverage before completing a full IVF cycle. Plus, there are additional costs outside of the basic IVF procedure, like diagnostic testing, medications, and genetic testing which may come with a hefty price tag you’d have to pay for. Without adequate coverage, many people have to make cost-based decisions, forgoing the technology they need to reach a successful outcome.
As an alternative, Progyny’s coverage is bundled, meaning your entire treatment event is covered and you do not have to worry about what is or is not included, or fear running out of coverage mid-way through. Many vendors have similar disruptive solutions to ensure they’re not leaving their members high and dry during difficult times.
When sifting through options, be sure you’re asking what’s covered and not covered under your plan. A lot of benefits may seem expansive, but make sure you’re getting the most out of the coverage that’s available to you. Ask: Are the best clinics in your area included in your plan as “in-network”? Do you have to meet medical necessity requirements before being allowed to access your benefits?
Which benefits are supported?
Once you’ve opted in for benefits during open enrollment, how do you access your benefit? How do you move forward with treatment? Does your benefit provide access to the doctors in your area? Since many of these offerings are complex and without proper onboarding, how can you be expected to understand the next steps?
With the growing emphasis on mental health and concierge member experience, companies like Progyny try to eliminate some of the member’s burden and create an easy to use benefit model that provides member support. For example, our dedicated Patient Care Advocates — a concierge-style fertility coach — helps members navigate the clinical and emotional aspects of your fertility treatment, making a difficult process a bit easier.
Another important factor to consider when shopping for benefits is access to care where you live — are the doctors that your insurance covers close by and easy to get to? When choosing your benefits, look out for any information about access to support. The goal of a benefit is to make your life easier, not leave you feeling confused and stressed in times of need.
What do I do if I’m unhappy with the benefits offered during open enrollment?
Often times, employers are unaware of what an employee wants until it’s brought to their attention. If you are unhappy with the benefits offered, raise the issue with your HR team! You are your own best advocate and change begins with you.
Not sure where to start? If you are comfortable, speak with your colleagues. Seek out a company resource group to see if others have similar needs. This way you can help form a plan or a way to approach HR. Once you have an idea of what you need, talk to HR to explain why the proposed benefit would be pertinent to you and your colleagues. Employers understand that the key to keeping good talent is making sure they’re happy.
Open enrollment can be overwhelming but take advantage of the resources you have. Ask questions, do your research, and discuss the options with experts in your office. With an arsenal of helpful information at your disposal, open enrollment should be stress-free and get you excited for all of the incredible employer-sponsored benefits in your future.
SOURCE: Ajmani, K. (25 November 2019) "Key factors in choosing your benefits during open enrollment" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/how-to-choose-benefits-during-open-enrollment
DOL’s new fluctuating workweek rule may pave road for worker bonuses
The Department of Labor’s new fluctuating workweek rule could give employers additional flexibility when calculating employee overtime pay and could potentially make it easier for workers to get bonuses. Read the following blog post to learn more about this newly proposed rule.
The Department of Labor’s new proposal would give employers additional flexibility when calculating overtime pay for salaried, non-exempt employees who work irregular hours — and may make it easier for some workers to get bonuses.
The new proposal, released this week, clarifies for employers that bonuses paid on top of fixed salaries are compatible with the so-called “fluctuating workweek” method of compensation, or a way of calculating overtime pay for workers whose hours vary week-to-week. Supplemental payments, such as bonuses or overtime pay, must be included when calculating the regular rate of pay under the Fair Labor Standards Act, according to the DOL.
"For far too long, job creators have faced uncertainty regarding their ability to provide bonus pay for workers with fluctuating workweeks," says Cheryl Stanton, wage and hour division administrator, at the DOL in a statement. "This proposed rule will provide much-needed clarity for job creators who are looking for new ways to better compensate their workers."
Paul DeCamp, an attorney with the law firm Epstein Becker Green’s labor and workforce management practice, says the DOL rule clears up ambiguity surrounding when employers can use the fluctuating workweek rule. A preamble in a 2011 Obama-era regulation suggested that bonuses were contrary to a flexible workweek, DeCamp says.
“The department’s past rulemakings have created ambiguity — paying employees a bonus makes the fluctuating workweek calculation unavailable,” DeCamp says. “During the last administration, some people with DOL took the position that the fluctuating workweek was only available when the compensation the employee received was in the form of salary.”
This new update may make it easier for employers to pay out bonuses or other kinds of compensation to a specific group of workers. Labor Secretary Eugene Scalia says the proposal will remove burdens on American workers and make it easier for them to get extra pay.
"At a time when there are more job openings than job seekers, this proposal would allow America's workers to reap even more benefits from the competitive labor market,” Scalia says.
DeCamp adds that the update will make it easier for employers to provide bonuses to these workers, without being concerned they are going to impact their overtime calculation.
“What this does is it makes it possible for employers who have salaried non-exempt employees to pay other types of compensation too — without worrying that in paying that bonus or other type of compensation they’re going to screw up their overtime calculation,” DeCamp says.
But DeCamp warns that employers should not confuse this regulation with the overtime rule that the DOL finalized in September, which raised the minimum salary threshold for overtime eligibility to $35,568 per year.
“These two regulations are not interlocking. They don’t really deal with the same subject,” he says. “They’re both talking about very different employee groups.”
SOURCE: Hroncich, C. (6 November 2019) "DOL’s new fluctuating workweek rule may pave road for worker bonuses" (Web Blog Post). Retrieved from https://www.benefitnews.com/news/dols-fluctuating-workweek-rule-helps-with-worker-bonuses
IRS updates rules on retirement plan hardship distributions
Recently, the Internal Revenue Service (IRS) finalized updates to the hardship distribution regulations. These new regulations make the requirements more flexible and participant friendly. Read this blog post to learn more about these updated regulations.
Employers who allow for hardship distributions from their 401(k) or 403(b) plans should be aware that the Internal Revenue Service recently finalized updates to the hardship distribution regulations to reflect legislative changes. The new rules make the hardship distribution requirements more flexible and participant-friendly.
Hardship distributions are in-service distributions from 401(k) or 403(b) plans that are available only to participants with an immediate and heavy financial need. Plans are not required to offer hardship distributions. But there are certain requirements if a plan does offer hardship distributions. Generally, a hardship distribution may be made to a participant only if the participant has an immediate and heavy financial need, and the distribution is necessary and not in excess of the amount needed (plus related taxes or penalties) to satisfy that financial need.
An administrator of a 401(k) or 403(b) plan can determine whether a participant satisfies these requirements based on all of the facts and circumstances, or the administrator may rely on certain tests that the IRS has established, called safe harbors.
Over the last fifteen years, Congress has changed the laws that apply to hardship distributions. The new rules align existing IRS regulations with Congress’s legislative changes. Some of the changes are mandatory and some are optional. The new rules make the following changes. The following changes are required.
Elimination of six-month suspension.
Employers may no longer impose a six-month suspension of employee elective deferrals following the receipt of a hardship distribution.
Required certification of financial need.
Employers must now require participants to certify in writing or by other electronic means that they do not have sufficient cash or liquid assets reasonably available, in order to satisfy the financial need and qualify for a hardship distribution.
There were also some optional changes made to hardship distributions.
Removal of the requirement to take a plan loan.
Employers have the option, but are not mandated, to eliminate the requirement that participants take a plan loan before qualifying for a hardship distribution. In order to qualify for a hardship distribution, participants are still required to first take all available distributions from all of the employer’s tax-qualified and nonqualified deferred compensation plans to satisfy the participant’s immediate and heavy financial need. The optional elimination of the plan loan requirement may first apply beginning January 1, 2019.
Expanded safe harbor expenses to qualify for hardship.
The new hardship distribution regulations expand the existing list of pre-approved expenses that are deemed to be an immediate and heavy financial need. Prior to the new regulations, the list included the following expenses:
- Expenses for deductible medical care under Section 213(d) of the Internal Revenue Code;
- Costs related to the purchase of a principal residence;
- Payment of tuition and related expenses for a spouse, child, or dependent;
- Payment of amounts to prevent eviction or foreclosure related to the participant’s principal residence;
- Payments for burial or funeral expenses for a spouse, child, or dependent; and
- Expenses for repair of damage to a principal residence that would qualify for a casualty loss deduction under Section 165 of the Internal Revenue Code.
The new regulations expand this list of permissible expenses by adding a participant’s primary beneficiary under the plan as a person for whom medical, tuition and burial expenses can be incurred. The new regulations also clarify that the immediate and heavy financial need for principal residence repair and casualty loss expenses is not affected by recent changes to Section 165 of the Internal Revenue Code, which allows for a deduction of such expenses only if the principal residence is located in a federally declared disaster zone. Finally, the new regulations add an additional permissible financial need to the list above for expenses incurred due to federally declared disasters.
New contribution sources for hardships.
The law and regulations provide that employers may now elect to allow participants to obtain hardship distributions from safe harbor contributions that employers use to satisfy nondiscrimination requirements, qualified nonelective elective contributions (QNECS), qualified matching contributions (QMACs) and earnings on elective deferral contributions. However, 403(b) plans are not permitted to make hardship distributions from earnings on elective deferrals, and QNECS and QMACs are distributable as hardship distributions only from 403(b) plans not held in a custodial account.
As this list indicates, the new regulations make substantial changes to the hardship distribution rules.
The deadline for adopting this amendment depends on the type of plan the employer maintains and when the employer elects to apply the changes. Plan sponsors should work with their document providers and legal counsel to determine the specific deadlines for making amendments.
SOURCE: Tavares, L. (01 November 2019) "IRS updates rules on retirement plan hardship distributions" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/irs-updates-rules-on-401k-403b-plan-hardship-distributions
‘Eye’ spy a savings opportunity for health and vision benefits
The National Eye Institute reported that 61 million adults are at high risk for serious vision loss. Conventionally, vision benefits were offered as an elective, with coverage is focusing on vision tests or discounts for corrective eyewear. Read the following blog post to learn more about vision benefits.
Sixty-one million adults are at high risk for serious vision loss, according to the National Eye Institute, but most U.S. employers don’t include eye care as part of their benefits package. Vision benefits have traditionally been offered as an elective, where coverage is focused on vision tests or discounts for corrective eyewear.
This often results in inadequate coverage for employees and dependents, which can result in unrecognized and untreated issues that impact employee health and productivity, as well as an employer’s bottom line.
Comprehensive eye exams are recommended for adults under the age of 65 at least every two years, according to the American Optometric Association (AOA). These exams are the only way a doctor can detect signs and symptoms of serious conditions without cutting into or scanning body parts.
The total economic burden of eye disorders and vision loss in the U.S. was $139 billion in 2013, which includes $65 billion in direct medical costs strictly due to eye disorders and low vision. Loss of vision among workers results in $48 billion in lost productivity per year.
When it comes to benefit management priorities employers often focus more on chronic condition management. Yet, eye health is often linked to common chronic conditions including diabetes and hypertension. Without early detection of eye and vision health issues, employees cannot properly manage these conditions. Delaying medical treatment can lead to increased absenteeism and reduced productivity, eventually resulting in treatment that comes too late, and at a much higher price tag for employers, employees and family members.
About 68% of Americans with diabetes have been diagnosed with eye complications, many of which could have been prevented through a comprehensive eye exam. Diabetes is the leading cause of blindness among adults, according to the National Institutes of Health. Its prevalence is increasing as one in 10 people worldwide may be affected by 2040, according to research from the International Diabetes Federation.
Nearly half of Americans don’t know that diabetic eye diseases have visible symptoms, according to a 2018 AOA survey. More than one-third of respondents didn’t know a comprehensive eye exam is the only way to determine if a person’s diabetes will cause blindness. These exams, considered the gold standard in clinical vision care, should be covered under the employees’ medical benefits.
Three years ago the Midwest Business Group on Health began a collaboration with the AOA to better understand how employers think about and implement eye health and vision benefits. As part of this partnership, a no-cost eye care benefits toolkit was developed to support employers in evaluating their current eye health and vision care benefits to:
- Understand the importance of early detection so that employees can effectively manage chronic and more serious conditions
- Recognize how to integrate primary and preventive eye care into an overall medical benefit design
- Educate employees on the importance of periodic eye examinations
It’s important that employers better understand the impact of vision care benefits, including lower costs, better employee health, improved job satisfaction, better employee quality of life, and work productivity.
SOURCE: Larson, C. (20 September 2019) "‘Eye’ spy a savings opportunity for health and vision benefits" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/vision-loss-resulting-in-billions-in-lost-productivity
6 voluntary benefits your employees want
Multigenerational workforces are no longer finding the run-of-the-mill benefits plans adequate. This is making voluntary benefits more important than ever in this age of the multigenerational workforce and a tight labor market. Read this blog post from for six voluntary benefits employees want.
In this age of the multigenerational workforce and a tight labor market, a one-size-fits-all group benefits model with medical, prescription, dental, vision and a retirement plan just doesn’t cut it. A workforce with Baby Boomers, Gen X’ers, Millennials and Generation Z means that employees are going to find the run-of-the-mill benefits plan inadequate. Ditto for job seekers.
What follows is that voluntary benefits are more important than ever. Offering a range of voluntary benefits can help meet the needs of employees at all life stages.
Voluntary benefits add value to benefit plans and are typically easy to administer. They’re low-to-no-cost because employees pay for them, and maintenance is often handled through a payroll deduction. Many voluntary benefits also offer guaranteed acceptance at a lower rate than medical benefits, so even if a small group within your company chooses a particular benefit, they’ll be covered.
This landscape is changing quickly. Here are six trending voluntary benefits your employees want.
Student loan debt repayment assistance
Debt among college graduates has grown to nearly $1.6 trillion. It’s preventing the largest employee segment at most companies from buying houses or cars, saving for retirement, having kids and getting married. To help employees repay their student loan debt, some employers are helping employees pay down student loan debt through a direct payroll deduction.
Others are offering a new, IRS-allowable retirement plan match swap where an employer can opt to increase its defined contribution match, enabling employees to reduce their retirement match and contribute funds to repaying student loans instead.
Interest in this benefit continues to grow. Employers looking to offer student loan debt repayment should be aware that not all platforms are created equal. Look out for high per-employee, per-month fees.
Individual long-term care
A growing number of people are beginning to understand the value of long-term care insurance because they have taken care of or currently care for a friend or relative who needs round-the-clock care. Long-term care insurance covers home or institutional care if a person is no longer able to perform at least two activities of daily living--eating, bathing, dressing, moving from a bed to a chair or using a toilet.
Employees are interested in buying long-term care insurance through their employer because they can offer better rates for simplified issue plans. If you plan to offer long-term care as an employer-sponsored benefit, I recommended rolling it out with a strategic project plan and a benefit counselor or a technology platform capable of providing decision-making tools for a smooth application process.
Executive reimbursement plans
Employee retention — especially executive retention — is on the minds of many employers in the midst of this thriving economy. Filling gaps in medical and prescription coverage is one way to provide executive teams with premium benefits they may be looking for.
Executive reimbursement plans provide reimbursement for out-of-pocket expenses, access to facilities and level of service not normally covered under most group health plans. Rather than simply increasing compensation to help cover out-of-pocket expenses, premiums for these plans are tax-deductible for the employer, and benefits are non-taxable for employees.
Executive individual disability insurance
Traditional employer-sponsored long-term disability (LTD) is likely not enough coverage for highly-compensated employees or some sales staff who depends heavily on commission and bonuses. Normally, LTD pays employees 50-70% of their salary up to a certain amount.
Employers can carve out additional coverage for employees based on their management level, performance or tenure. Individual disability insurance plans can protect employees until they turn 65; they can also protect job titles or levels until employees are well enough to return to work. Executive individual disability insurance, like executive reimbursement, can be offered as a form of compensation, or a form of financial asset protection for higher incomes.
Telemedicine
The rise of consumer-driven health plans has led to the need for telemedicine. Telemedicine provides a way for employees to see a physician or provider by video and get a diagnosis and/or prescription quickly. The success of telemedicine is leading some carriers to integrate it within their plan. However, standalones still exist and can provide employees with an easy way to get care faster and cheaper than before.
Pet Insurance
Pet parents spend nearly $70 billion on veterinarian costs for their pets, but just 10% of dogs and 5% of cats are covered by medical insurance. As pets begin to play a larger role in our lives, more employers are offering pet insurance to their employees to help defray the cost of unexpected medical expenses.
There are a number of plan options, and setting up a plan for employees’ pets is simple. However, it’s vital that employers do their research to ensure the veterinarian network includes the best vets.
As part of a voluntary benefit offering, be sure to develop a rollout strategy and communications plan so employees are thoroughly educated and you meet group minimums.
SOURCE: Park, N. (25 September 2019) "6 voluntary benefits your employees want" (Web Blog Post). Retrieved from https://www.benefitnews.com/list/6-voluntary-benefits-your-employees-want
Key elements to consider when researching financial wellness programs
With financial wellness programs becoming a staple employee benefit, organizations find themselves implementing programs that only offer a few tools or resources. Read the following blog post from Employee Benefit Advisor for key elements to consider when researching financial wellness programs.
Financial wellness programs are becoming a staple in the employee benefit universe. But what should a successful financial wellness program encompass? As a rapidly growing industry, we often lack a consistent definition for financial wellness. This leads to organizations believing they have implemented a financial wellness program, when they may only be offering a few tools like education or counseling.
I define financial wellness as the process by which an individual can efficiently and accurately assess their financial posture, identify personal goals, and be motivated to gain the necessary knowledge and resources to create behavioral change. Behavioral change will result in improved emotional and mental well-being, along with short- and long-term financial stability.
As the administrator of your company’s benefits, you are responsible for bringing the best possible solution to your employees. That’s a tough ask, given the growing number of service providers. So, what is the most efficient and effective way to assess financial wellness services to determine which solution best fits your organizational needs? Ask yourself these questions:
Does the platform offer a personal assessment of each employee’s current financial situation and help them identify their financial goals? If the answer is yes: Does the assessment return quantifiable and qualifiable data unique to each individual employee?
Does the platform address 100% of your employee base, including the least sophisticated employees at various levels of employment? Much of your ROI from a financial wellness program does not come from your top performers. It comes from creating behavioral changes within your employees who need the most financial guidance.
Does the platform integrate the various components to provide a personalized roadmap for each employee? It should connect program elements like personal assessments, educational resources, tools, feedback and solutions to ensure the employee is presented with a cohesive, comprehensive plan to attack and improve their financial situation.
Does the platform offer solutions for short-term financial challenges like cash flow issues, as well as long-term financial challenges associated with saving and planning? A major return on your investment comes from reduced employee stress, which is substantially driven by short-term needs versus long-term objectives. The program must help employees deal with current financial challenges before they can focus on their longer-term vision.
About 78% of U.S. workers live paycheck to paycheck to make ends meet, according to data from CareerBuilder.com. The need for financial wellness is clear, but there are consistent pillars that must be addressed in any successful financial wellness program to affect change: spend, save, borrow and plan. When evaluating financial wellness programs, it’s important that these dots all connect if you are truly going to motivate behavioral change and recognize the ROI of a comprehensive financial wellness program.
SOURCE: Kilby, D. (13 September 2019) "Key elements to consider when researching financial wellness programs" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/opinion/key-considerations-for-employee-financial-wellness-programs
4 pitfalls of paid leave and how clients can avoid them
Employers are using paid leave options to help boost their employee benefits packages in efforts to better attract and retain talent. Read the following blog post from Employee Benefit Advisor for 4 common pitfalls of paid leave and how employers can avoid them.
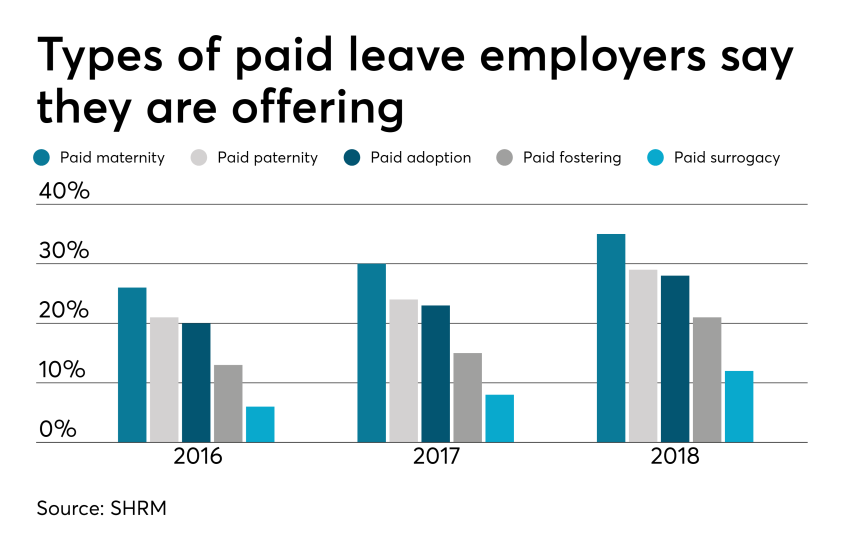 Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
Smart employers are boosting their benefits packages with paid family leave — the most coveted work perk among all generations. In today’s low unemployment environment, paid leave benefits can be a huge differentiator in attracting and retaining talent.
But some employers are getting themselves into trouble in the process, facing accusations of gender discrimination or improper use of leave.
Here are four potential pitfalls of paid leave, and how employers can avoid them.
1. Be careful what you call “maternity leave.”
Employers have long been granting leave for new moms in the form of disability coverage. In fact, the top cause of short term disability is pregnancy. Disability insurance usually grants new moms six to eight weeks of paid leave to recover from childbirth.
Because this coverage applies to the medical condition of recovering from childbirth, it shouldn’t be lumped in with bonding leave.
Guidance from the Equal Employment Opportunity Commission says leave granted for new moms for bonding must also be extended to new dads, so separating disability leave from bonding leave is crucial to avoiding gender discrimination.
2. Don’t make gender assumptions.
The amount of bonding time for new parents after birth, adoption or fostering must be granted equally for men and women. Companies that don’t provide the same amount of paid leave for men and women may find themselves in a discrimination lawsuit.
It’s not just the time away from work that matters, but also the return-to-work support provided. If new moms are granted temporary or modified work schedules to ease the transition back to work, new dads must also have access to this.
Some companies may choose to differentiate the amount of leave and return-to-work support for primary or secondary caregivers. That’s compliant as long as assumptions aren’t made on which gender is the primary or secondary caregiver.
The best way to avoid potential gender discrimination pitfalls is to keep all parental bonding and related return-to-work policies gender neutral.
3. Avoid assuming the length of disability.
Be careful about assuming the length of time a new mom is disabled, or recovering medically, after birth. Typical coverage policies allot six to eight weeks of recovery for a normal pregnancy, so assuming a new mom may be out for 10 weeks might be overestimating the medical recovery time, and under-representing the bonding time, which must be gender neutral.
4. Keep up with federal, state and local laws.
Mandated leave laws are ever-evolving, so employers should consistently cross-check their policies with state and local laws. For instance, do local paid leave laws treat adoption the same as birth? Are multistate employers compliant? What if an employee lives in one state but works in another: Which state’s leave policies take precedence?
Partnering with a paid leave service provider can mitigate the risk of improperly administering leave. Paid leave experts can help answer questions, review guidelines and provide information regarding job-protecting medical or family leave.
They can also help flag potential pitfalls, ensuring leave requests from all areas of your company are managed uniformly and in accordance with state and federal laws, including the EEOC.
SOURCE: Bennett, A. (12 September 2019) "4 pitfalls of paid leave and how clients can avoid them" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/list/4-pitfalls-of-paid-leave-and-how-clients-can-avoid-them
5 Questions Expecting Moms Have About Life Insurance
Are you considering life insurance? If this is your first time looking for coverage, you most likely have questions. Read this blog post from Life Happens for five questions expecting mothers typically ask when looking at life insurance.
If you are expecting a child and are considering life insurance, the first thing I have to say is—smart move! But if this is your first time looking for coverage, you may have questions. Here are some typical ones I’ve heard over the years:
1. What type of life insurance coverage is best for new parents—term or permanent?
Before figuring out what kind of coverage you need, you first have to understand how much death benefit you need to protect your family. You can do an easy calculation online to get a working idea of how much you may need with this Life Happens Life Insurance Needs Calculator.
Then you can move on to what kind of coverage—term or permanent—meets your needs. An advantage of term life insurance is that it costs less than permanent, at least initially. This makes it affordable for young families that may not have a lot of disposable income, but have a large need for coverage. Permanent insurance provides both lifelong coverage and a cash accumulation feature, which can be a valuable source of money that you can tap in the future.
Often, the best solution can be a combination of term and permanent life insurance. The term policy can give you extra coverage during the years when the children are at home, with the permanent policy offering lifelong coverage.
2. Should you consider different types of coverage if you are working mom versus a stay-at-home mom?
Both working and stay-at-home moms need protection because what they do for their families is so valuable. While a stay-at-home mom isn’t compensated for her work, if something were to happen to her, it would be expensive to replace all those things she does—from childcare to home care to ensuring the family gets where they need to go when they have to be there.
The difference between the two is that a working mother also contributes an income, which may be critical to the family financially. That means she needs to think about replacing that income when considering how much life insurance coverage she may need.
3. The company where I work offers life insurance, is that enough?
Group insurance is a great benefit to have, but it’s limited in a number of ways. First, the coverage is often a lump sum, such as $50,000, or it may be one to two times your salary. That may sound like a lot of money, but my question to you is: Honestly, how long would that money last? And what would happen to your family financially after that was gone?
Second, when you leave that job, you generally lose that coverage. If you don’t have an individual policy that you own, you’ll be leaving your family at risk. Think of how many times people change jobs, and you’ll quickly realize that group coverage, which is limited in scope and amount, is not a proper life insurance plan.
4. Are there any restrictions I have to consider now that I’m pregnant?
If it’s early in your pregnancy, and there are no medical complications, you should be able to get life insurance. If you’re farther along and there are medical issues, it may difficult to obtain. The life insurance company may want to wait until after your child is born. That’s why I advise those that are planning to have children to get the coverage as soon as possible.
5. What can I expect to pay for life insurance?
How much you pay for life insurance is based on a number of things but most importantly age and health. So, it depends on how old and how healthy you are! But here’s an example: A healthy 30-year-old woman could get $250,000 in life insurance coverage (for a 20-year level term policy for a nonsmoker) for about $13 a month. That’s certainly a lot of peace of mind for $13.
And don’t forget about your spouse or partner. The two of you could get $500,000 of combined coverage (using the example of two 30-year-olds that each get a $250,000 20-year level term policy) for right around $26 a month.
And my last piece of advice: talking with a life insurance agent at this stage can be very valuable. They can do a needs assessment and come up with the right type and amount of life insurance that works for your family budget. And what many people don’t realize is that an agent will sit down and offer this advice free of charge, with no strings attached. If you’d like help finding a life insurance professional, you can start here.
SOURCE: Feldman, M. (23 August 2019) "5 Questions Expecting Moms Have About Life Insurance" (Web Blog Post). Retrieved from https://lifehappens.org/blog/5-questions-expecting-moms-have-about-life-insurance/










