Why employee performance management needs an HR tech overhaul
Are annual performance reviews necessary? A recent survey by Adobe reveals that 58 percent of people feel that performance reviews are not necessary. Continue reading to learn more.
According to a recent survey conducted by Adobe, 58% of people feel that performance reviews “are a needless HR requirement.” Adobe, in fact, no longer has an annual performance review process and instead has adopted an approach involving ongoing discussions between managers and employees that emphasize talent development and future productivity instead of formal ratings and rankings based on past performance.
Still, the vast majority of companies continue to persist with a backward-looking evaluation process that is time-consuming for managers, demotivating for employees and of negligible benefit to the business as a whole. They do this because, as Adobe’s survey respondents suspected, performance reviews are more about “compliance than customer service.”
Focusing on past performance is an industrial-era hangover from when employees were mainly required to hit targets in easily measurable, repetitive tasks. Although most people’s jobs have evolved to be more complex and creative since then, the process and the tools used to manage their efficacy and performance in those roles have not.
In many respects, HR is still a defensive function whose role is to protect the business from its own employees. This is reflected by HR technology that is built for compliance, rather than helping managers and employees become more productive.
HR’s on-premise or enterprise resource planning systems can track performance reviews to prove a dismissal was not unfair, rank employees to justify compensation distribution and demonstrate effective people management to the board or shareholders. What they can’t do is react positively to the ever-changing demands of the modern business world and help employees and managers meaningfully improve their skills to meet the challenges of tomorrow.
Performance management is changing — but HR tech is not
These days, a company’s and individual employee’s goals can change dramatically in the time between end-of-year reviews. Individual roles are more specialized and require frequent skill updates, while cross-functional teams have long since replaced the siloed departments that were standard just 10 years ago. In this environment, HR’s focus on past compliance is detrimental to future development.
Forward-thinking companies are changing the performance process to focus on development and continuous feedback that makes managers and employees more productive and engaged. The success of these trailblazers will encourage other businesses from a wide range of industries to follow suit.
This new model of performance management needs help from technology, but existing HR tech vendors are not keeping up. Their services are so embedded in the world of compliance, they cannot change to support the development needs of managers and employees. Fortunately, the solution already exists.
Creating a connected system of productivity
One of the key issues with performance reviews is that so much of the process involves looking back to gather the data. For managers, it is a huge time investment. For employees, end-of-year feedback about an issue that occurred months beforehand is too late to be useful.
The process seems doubly inefficient when you realize that real-time, instantly-actionable performance data is already available in productivity systems like JIRA and Salesforce that are used by different teams. The problem is HR’s defensive mindset has made it difficult to integrate existing internal or ERP systems with these tools.
Dedicated performance management services that connect to both HR systems and the departmental productivity tools can take HR technology out of its silo. This will create a connected system of productivity that uses real-time data alongside transparent and flexible goal-tracking to drive ongoing development conversations between managers and employees.
It’s time for HR to evolve from a defensive function to make a positive contribution to key business goals and become what HR analyst Josh Bersin calls the “chief of productivity.” This demands a shift from a performance review process based on compliance to a human-centered, development-focused experience.
Adopting new performance technology that integrates with widely-used productivity tools is a key step to ensuring everyone from employees to managers to HR can work on what matters most in order to meet today’s goals and tomorrow’s challenges.
SOURCE: Dennerline, D. (15 October 2018) "Why employee performance management needs an HR tech overhaul" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/why-employee-performance-management-needs-an-hr-tech-overhaul?brief=00000152-14a7-d1cc-a5fa-7cffccf00000
5 ways employers can leverage tech during open enrollment
Are you leveraging technology advancements during open enrollment? Advances in technology are creating a more seamless and interactive healthcare experience for employees. Read on for five ways employers can leverage technology during 2019 open enrollment.
Technology continues to reshape how employers select and offer healthcare benefits to employees, putting access to information at our fingertips and creating a more seamless and interactive healthcare experience. At the same time, these advances may help employees become savvier users of healthcare, helping simplify and personalize their journey toward health and, in the process, help curb costs for employers.
The revolution can be important to remember during open enrollment, which occurs during the fall when millions of Americans select or switch their health benefits for 2019. With that in mind, here are five tips employers should be aware of during open enrollment and year-round.
Make sense of big data
Help people understand their options
Encourage your people to move more
Offer incentives to employees who comparison shop for care
Integrate medical and ancillary benefits
5 things small business owners should know about this year's open enrollment
For small business owners, the benefits they offer are crucial to the way they attract and retain employees. Read this blog post for five things small business owners should know for 2019 open enrollment.
As a small business owner, offering competitive employee benefits is a crucial way to attract and retain strong talent. Whether you currently provide them and are planning next year’s renewal, or you are thinking of offering them for the first time, here are five things you should consider before your employees enter the open enrollment period for next year on November 1st:
1. Small businesses don’t have to wait until open enrollment to offer benefits to their employees
While your employees won’t be able to enroll in health insurance plans until November comes along, small business owners don’t have to wait at all to secure health insurance for their employees. The sooner you act, the better, to guarantee that you and your employees are protected. According to recent studies, healthier employees are happier employees, and as a result, will contribute to a more productive workplace. And a more positive and constructive work environment is better for you, your employees, and your business as a whole.
2. Health literacy is important
Whether you’ve provided health insurance to your employees before, or you’re looking into doing so for the first time, it is always worthwhile to prioritize health insurance literacy. There is a host of terminology and acronyms, not to mention rules and regulations that can be overwhelming to wrap your head around.
Thankfully, the internet is full of relevant information, ranging from articles to explainer videos, that should have you up to speed in no time. Having a good understanding of insurance concepts such as essential health benefits, employer contributions, out-of-pocket maximums, coinsurance, provider networks, co-pays, premiums, and deductibles is a necessary step to being better equipped to view and compare health plan options side-by-side. A thorough familiarization with health insurance practices and terms will allow you to make the most knowledgeable decisions for your employees and your business.
3. Offering health insurance increases employee retention
Employees want to feel like their health is a priority, and are more likely to join a company and stay for longer if their health care needs are being met. A current survey shows that 56 percent of Americans whose employers were sponsoring their health care considered whether or not they were happy with their benefits to be a significant factor in choosing to stay with a particular job. The Employee Benefit Research Institute released a survey in 2016 which showed a powerful connection between decent workplace health benefits and overall employee happiness and team spirit—59 percent percent of employees who were pleased with their benefits were also pleased with their jobs. And only 8 percent of employees who were dissatisfied with their benefits were satisfied with their jobs.
4. Alleviate health insurance costs
High insurance costs can be an obstacle for small business owners. A new survey suggests that 53 percent of American small business owners stress over the costs of providing health care to their employees. The 2017 eHealth report reveals that nearly 80 percent of small businesses owners are concerned about health insurance costs, and 62 percent would consider a 15 percent increase in premiums to make small group health insurance impossible to afford. However, there are resources in place to help reduce these costs, so they aren’t too much of a barrier. One helpful way to cut down on health insurance costs is to take advantage of potential tax breaks available to small business owners. All of the financial contributions that employers make to their employees’ premiums are tax-deductible, and employees’ financial contributions are made pre-tax, which will successfully decrease a small business’ payroll taxes.
Additionally, if your small business consists of fewer than 25 employees, you may be eligible for tax credits if the average yearly income for your employees is below $53,000. It is also beneficial to note that for small business owners, the biggest driver on insurance cost will be the type of plan chosen in addition to the average age of your employees. Your employees’ health is not a relevant factor.
5. Utilize digital resources
You don’t have to be an insurance industry expert to shop for medical plans. There are resources and tools available that make buying medical plans as easy as purchasing a plane ticket or buying a pair of shoes online – Simple, transparent. Insurance is a very complex industry that can easily be simplified with the use of the advanced technology and design of online marketplaces. These platforms are great tools for small business owners to compare prices and benefits of different plans side-by-side. Be confident while shopping for insurance because all of the information is laid out on the table. Technological solutions such as digital marketplaces serve as useful tools to modernize the insurance shopping process and ensure that you and your team are covered without going over your budget.
SOURCE: Poblete, S. (15 October 2018) "5 things small business owners should know about this year's open enrollment" (Web Blog Post). Retrieved from https://www.benefitspro.com/2018/10/15/5-things-small-business-owners-should-know-about-t/
What employers can do to combat risks of workplace opioid abuse
How can employers combat the risks associated with workplace opioid abuse? With an increase in opioid use, employers are now tasked with the challenge of addressing opioid misuse in the workplace. Continue reading to learn more.
The opioid epidemic presents a unique challenge for employers. While opioids can be beneficial for employees suffering from pain, they also pose grave risks and dangers for companies as even appropriate use of the drugs can cause impairment and lead to accidents.
For example, if an employee had an accident and suffers an injury, you may see the physical signs of the injury. However, it’s not as obvious if the employee was prescribed opioids for the pain associated with that injury. If the employee doesn’t disclose the prescription, they could resume their everyday duties, like operating machinery, when they should be restricted while using the drug.
Due to the increasing prevalence of opioid use, employers are likely now challenged with addressing misuse in the workplace. Often, companies may not know the best approach to supporting employees dealing with an opioid addiction. When speaking with employers, it’s important to stress the need for organizations to be well-versed in opioid misuse and ways to proactively identify and address it.
Employers can work to combat opioid use in their organization by providing accommodations and updating their policies, procedures and employee communications. Here are a few ways they can get started.
Short-term accommodations
If an employee is taking prescribed opioids for an injury and has specific limitations or restrictions, an employer can work with a disability carrier to determine potential short-term accommodations that can be made to meet the employee’s needs. Short-term accommodations can help keep an employee comfortable and productive at work during his or her recovery.
Policies and procedures
If an employer hasn’t done so already, it should consider putting a comprehensive drug policy in place to help it address issues that may arise if an employee misuses prescription drugs. The policy should include a description of available assistance options for employees who are struggling with substance abuse and clearly state consequences for employees who violate the policy, empowering supervisors to take appropriate action in response to employee issues.
Destigmatizing use
It’s easier to help someone if they come forward, but right now, stigma surrounding opioids can cause employees to keep their prescription use to themselves. Encouraging open lines of communication can help companies destigmatize prescription drug use so their employees feel comfortable disclosing the medications they’re taking that could limit them at work.
Fostering transparency, combined with short-term accommodations and clear policies, can help employees feel more comfortable coming forward with their condition. Remind employers that their disability carrier can be a great resource to help with education, recommend proactive ways to address misuse at their organization and create accommodation plans for employees in need. With these steps, employers can help support their employees and, ultimately, make the workplace a safer place for all.
SOURCE: Jolivet, D (16 October 2018) "What employers can do to combat risks of workplace opioid abuse" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/what-employers-can-do-to-combat-workplace-opioid-abuse-risk
Ready for the sounds of office sniffles?
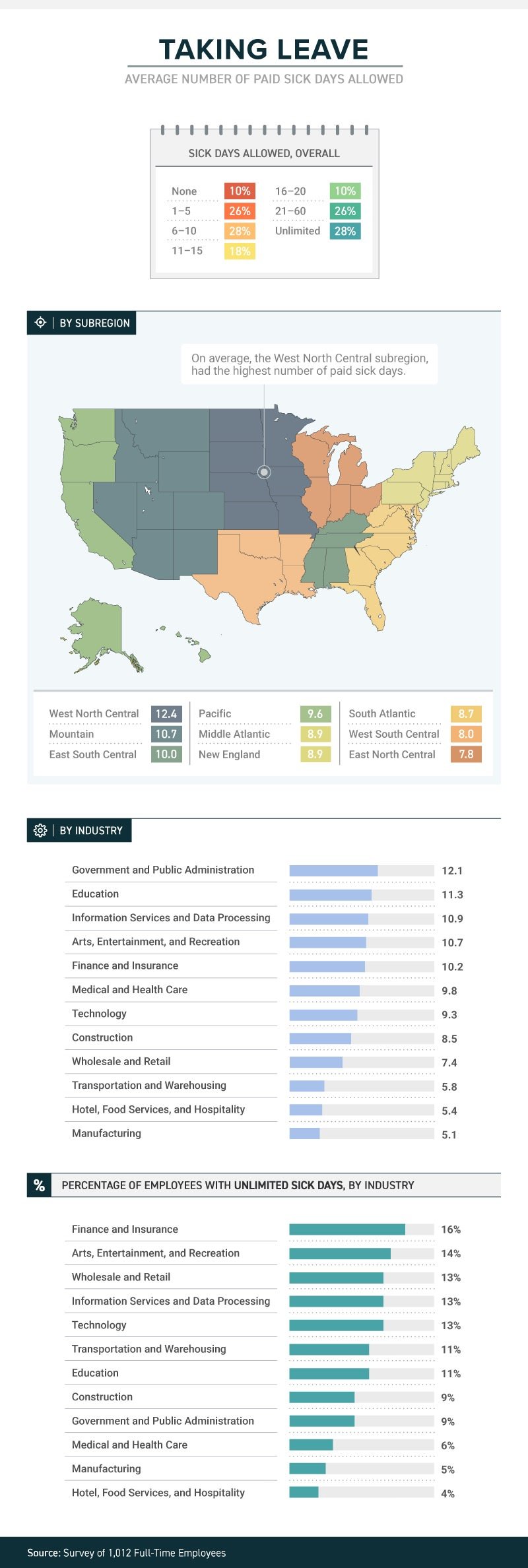
A recent study by law firm, Farah and Farah, states that one in four full-time workers receive between 1 and 5 sick days. Continue reading to learn more.
It’s not just a matter of whether they feel well enough to work, or whether they have sick days. The boss’s attitude about whether workers should take sick days or not can determine whether they actually do stay home when they’re sick, or instead come to work to spread their germs to all and sundry.
A new study from law firm Farah & Farah finds that even though it can take a person some 10 days to fully recover from a cold, approximately 10 percent of full-time workers in the U.S. get no sick days at all (part-timers don’t usually get them either), while more than 1 in 4 have to make do with between 1 and 5 sick days. Just 18 percent get enough sick time to actually recover from that cold—between 11 and 15 days.
The amount (or presence) of sick time varies from industry to industry, with government and public administration providing the most (an average of 12.1) and both hotel, food services and hospitality and manufacturing providing the least (an average of 5.4 for the hospitality industry and 5.1 for manufacturing). Some lucky souls actually get unlimited sick days, although even then they don’t always use them.
Regardless of industry, or quantity, just because workers get sick days it doesn’t mean they use them. Workers often worry that they’ll be discouraged from using them, with employers who may provide them but not encourage employees to stay home when ill. In fact, 38 percent of workers show up to work whether they’re contagious or not. Sadly for the people they encounter at work, the most likely to do so are in hospitality, medical and healthcare and transportation. Plenty of germ-spreading to be done in those professions!
And their employers’ attitudes play a role in how satisfied they are with their jobs. Among those who work for the 34 percent of bosses who encourage sick employees to stay home, 43 percent said they’re satisfied with their jobs in general. Among those who work for the 47 percent of bosses who are neutral about the use of sick days, that drops to 21 percent—and among the unfortunate workers who work for the 19 percent of bosses who actually discourage workers from staying home while ill, just 12 percent were satisfied with their jobs.
When it comes to mental health days (no, not that kind; the ones people really need to deal with diagnosed mental health conditions), fewer than 1 in 10 men and women were willing to call in sick. Taking “mental health days” when physically healthy, however, either to play hooky or simply have a vacation from the office, is something that 15 percent of respondents admitted to.
SOURCE: Satter, M (5 October 2018) "Ready for the sounds of office sniffles?" (Web Blog Post). Retrieved from https://www.benefitspro.com/2018/10/05/ready-for-the-sounds-of-office-sniffles/
Original report retrieved from https://farahandfarah.com/studies/sick-days-in-america
4 best practices for implementing a gamification-based compliance training system
Many employees may dislike and even disengage when their employer mentions implementing training sessions. Continue reading to learn how implementing a gamification-based training system can help improve employee engagement.
For most employees, compliance training is the Brussels sprouts on the kid’s plate of working life. Everyone knows it’s good for you — one mistake could lead to violations, accidents, reputation issues and maybe a not-so-friendly visit from regulatory body officials — but most workers turn up their noses and disengage when it’s time to dig in.
Considering that merely a third of American workers report feeling engaged at work as it stands, anything that makes matters worse is dangerous. Why risk inflaming indifference — not to mention spending money for on-site instructors — with dull-as-dry-toast workshops?
A far better bet is to embrace technology and go virtual. Of course, online-based compliance training won’t guarantee heightened participation or enthusiasm unless they have one specific aspect: gamification.
Gaming elements can turn any virtual compliance training learning management system (LMS) into an immersive experience. ELearning compliance training participants can enjoy customization and flexibility while getting up to speed on the latest rules, guidelines and protocols. With LMS gamification, HR managers and chief learning officers can cultivate and retain top talent. Best of all, it’s far easier to get buy-in for a robust LMS system with badges, bells and whistles than it is to make a pile of Brussels sprouts disappear from a toddler’s tray.
What exactly is so exciting about game-based learning? In essence, the process prompts active and immediate participation because of extra motivation in the form of rewards. Whether it’s badges or points, these features make eLearning interesting and enjoyable.
In one study, workers who enjoyed themselves retained concepts 40% better than those who weren’t having fun. As you might guess, this is what game-based learning is all about. Engaged employees who rapidly earn rewards are less likely to make errors, so they naturally increase a company’s bottom line and lower the likelihood of compliance fees and penalties. Plus, according to research from TalentLMS, 87% of employees report that gamification makes them more productive.
Merging gamification with training makes plenty of sense. It’s also easy to build a gamification-based compliance training LMS by following a straightforward LMS implementation checklist.
1. Identify your training goals and gaps. Before you can find the best LMS for your needs and move forward with an implementation project plan, you need to spot the inefficiencies of your existing compliance training program. For example, your strategy might not facilitate real-world applications. Knowing this, you would want a compliance training LMS that bridges gaps and imparts practical experience.
2. Discover what motivates and drives employees. Employee gamification only works when employees are properly incentivized, so find out what motivates your team based on their backgrounds and experience levels. Whether a task is challenging or boring, people respond better when they are internally driven to succeed.
Do you need an intuitive LMS with a personalized dashboard? Are the introverts on your team more driven by badges and points than by a sense of competition? Conduct surveys to gauge expectations, and try to follow a 70:20:10 model of training amplified by gaming to foster experimentation and collaboration.
3. Choose the right rewards for desired outcomes. With the plethora of LMS choices on the market, you can select from rewards and mechanics that lead to the exact behaviors and criteria you desire. Want employees to achieve safety online training certifications? Reward “graduates” with points after they have displayed their proficiency. Reinforce favorable behaviors without punishing workers who lag behind. Carrots are far more effective than sticks.
4. Invest in a feature-rich, gamification-supported LMS. Your LMS should not only be user-friendly, but it should also be a portal to game-based learning support and an online asset library. Ideally, your gamified learning platform should include themes and templates that allow you to design visually appealing rewards without reinventing the wheel. Just make sure you have game-based reporting on your side, which makes it simple to track employee performance, completion rates, and other LMS metrics.
Implementing a gamification-based compliance training strategy requires careful budgeting, planning, and analysis. Once you find an LMS platform that delivers the features you need within your price range, you’ll be on your way to mitigating risks and retaining superstar employees. And thanks to gamification, everyone can have a little fun along the way.
SOURCE: Pappas, C. (10 October 2018) "4 best practices for implementing a gamification-based compliance training system" (Web Blog Post). Retrieved from https://www.benefitnews.com/opinion/4-best-practices-for-implementing-a-gamification-based-compliance-training-system?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001
IRS updates required tax notice to address plan loan offsets
The model notices that all plan sponsors are required to send to plan participants before they receive an eligible rollover distribution from qualified plans were recently updated by the IRS. Continue reading to learn more.
The IRS has updated the model notice that is required to be provided to participants before they receive an “eligible rollover distribution” from a qualified 401(a) plan, a 403(b) tax-sheltered annuity, or a governmental 457(b) plan.
Notice 2018-74, which was published on September 18, 2018, modifies the prior safe-harbor explanations (model notices) that were published in 2014. Like the 2014 guidance, the 2018 Notice — sometimes referred to as the “402(f) Notice” or “Special Tax Notice” — includes two separate “model” notices that are deemed to satisfy the requirements of Code Section 402(f): one for distributions that are not from a designated Roth account, and one for distributions from a designated Roth account. The 2018 Notice also includes an appendix that can be used to modify (rather than replace) existing safe-harbor 402(f) notices.
The model notices were updated to take into consideration certain legislation that has been enacted, and other IRS guidance that has been published, since 2014. They include:
- changes related to qualified plan loan offsets under the Tax Cuts and Jobs Act of 2017;
- changes in the rules for phased retirement under the Moving Ahead for Progress in the 21st Century Act (“MAP-21”);
- changes in the exceptions to the 10% penalty for early distributions from governmental plans under the Defending Public Safety Employees’ Retirement Act; and
- IRS guidance (in Revenue Procedure 2016-47) regarding a self-certification procedure for waivers of the 60-day rollover deadline.
The model notices also make some “clarifying” changes to the 2014 notices, including:
- clarification that the 10% additional tax on early distributions applies only to amounts includible in income;
- an explanation of how the rollover rules apply to governmental 457(b) plans that include designated Roth accounts;
- clarification that certain exceptions to the 10% tax on early distributions do not apply to IRAs; and
- recognizing that taxpayers affected by federally declared disasters and other events may have an extended deadline for making rollovers.
The updated model 402(f) notices should be particularly useful in communicating to participants the extension, under the Tax Cuts and Jobs Act, of the time to roll over a “qualified plan loan offset amount.”
Inside the plan load offset
By way of background, Notice 2018-74 reminds us that distribution of a “plan loan offset amount” is an eligible rollover distribution, and that a “plan loan offset” occurs when, under the plan terms governing a plan loan, the participant’s accrued benefit is reduced, or offset, in order to repay the loan. According to the Notice, this can occur when, for example, the terms of the plan loan require that, in the event of an employee’s termination of employment or request for a distribution, the loan is to be repaid immediately or treated as in default.
The Notice also indicates that a plan loan offset may occur when, under the terms of the plan loan, the loan is canceled, accelerated, or treated as if it were in default (for example, when the plan treats a loan as in default upon an employee’s termination of employment or within a specified period thereafter). The Notice also reminds us, however, that a plan loan offset cannot occur prior to a distributable event.
This is helpful guidance for distinguishing between a “deemed distribution” of a defaulted loan (a taxable event which is not eligible for rollover) and a “plan loan offset amount,” which is an eligible rollover distribution.
Generally, if a default occurs before the participant has a distributable event (such as termination of employment, or attainment of age 59½), and the default is not cured by the last day of the cure period, it must be treated as a “deemed distribution” and reported on Form 1099. Such defaulted amounts are not eligible for rollover.
However, if the default occurs at or after a distribution event, and the plan terms require that the participant’s account be offset to pay off the loan, then the reduction of the account may be treated as a plan loan offset, which is an eligible rollover distribution.
Notice 2018-74 (and the new model notices) also reflect that, prior to the Tax Cuts and Jobs Act of 2017, participants who incurred a “plan loan offset” only had 60 days to “roll” an equivalent amount of money to an IRA or another employer plan (to avoid the offset being treated as a taxable distribution). However, for plan loan offsets that occur after December 31, 2017, if the plan loan offset is a “qualified plan loan offset” (meaning it occurs in connection with termination of employment or termination of the plan), then the participant has significantly more time (until the extended due date of the participant’s tax return for the year of the offset) in which to roll an amount equal to the loan offset amount to an IRA or another employer plan.
SOURCE: Browning, R (4 October 2018) "IRS updates required tax notice to address plan loan offsets" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/opinion/irs-updates-required-tax-notice-to-address-plan-loan-offsets?brief=00000152-146e-d1cc-a5fa-7cff8fee0000
Severance plans: How savvy employers can stay ERISA compliant
How can employers’ severance plans stay ERISA compliant? There are significant advantages associated with ERISA severance plans. Continue reading to learn more.
An employer’s promise to provide severance benefits may be written or oral, formal or informal, and individual or group. Determining whether an ERISA plan already exists, or whether an employer wants its severance arrangement to be subject to ERISA, is an important consideration in determining an employer’s obligation and liabilities associated with a severance arrangement.
There are significant advantages associated with a severance arrangement that is an ERISA plan as discussed in detail below. An employer, however, cannot unilaterally decide that the severance arrangement is an ERISA plan. Instead, an employer, when designing and administering a severance arrangement, can take definitive steps to ensure that the arrangement is treated as an ERISA plan.
Employers may assume that the first step to ensure the existence of an ERISA plan is to have a written plan document, which is required by ERISA. Surprisingly, this is not necessarily determinative as to whether an ERISA plan exists. Courts have held that ERISA plans can exist without a written plan document and vice versa.
Case law has provided the broad outlines of the nature of an ERISA-governed severance plan. An essential characteristic of ERISA severance plans is that, by their nature, they necessitate “an ongoing administrative scheme.” Courts have looked at the following indicators when determining what constitutes an ongoing administrative scheme:
- The employer’s discretion in determining (1) eligibility for benefits or (2) available plan benefits
- The form of payment such as lump sums versus periodic payments
- Any ongoing demand on the employer’s assets such that there is an ongoing scheme to coordinate and control the distribution of benefits
- Calculations based on certain factors such as job performance, length of service, reemployment prospects, and so forth.
Severance plans or arrangements that normally do not require an ongoing administrative scheme, and therefore, do not implicate ERISA, are plans that have lump-sum payments that are calculated under a formula and are mechanically triggered by a single event (such as termination). Where severance payments are made over time (through payroll, for example) and/or additional benefits (such as continuation of benefits or outplacement services) are provided, the severance arrangement is likely subject to ERISA.
As a practical matter, whether severance arrangements are ad hoc or recognized in a formal plan document, they may end up providing ERISA-covered benefits. In a dispute, an employer generally prefers that ERISA applies because of ERISA’s preemption of state laws. Preemption protects employers from state laws that may favor employees and generally limits the dispute to an ERISA claim for benefits, thereby avoiding the potential exposure to punitive, extra-contractual or special damages under state laws. In addition, ERISA’s claim procedure, which provides a pre-litigation administrative process for dispute resolution, will apply if proper plan language is provided. If employees with a severance claim fail to faithfully follow the ERISA claims procedure, their lawsuits may be dismissed for failure to exhaust administrative remedies.
Typically, the plan document gives the employer, in its capacity as plan administrator, the discretionary authority to interpret the plan’s language and make decisions about the plan. If the employee follows the claim procedures and the claim is denied, the decision-making process of the employer (or its designee) if done properly, is given deferential treatment by a reviewing court. Moreover, in many cases, judicial review is limited to only those matters addressed in the administrative record of the claim. In other words, many federal courts would decline to consider factual matters that were not raised by the employee in the claim procedure process.
Another consideration for the savvy employer is that severance benefits are almost always considered to be “welfare” benefits. Welfare benefits, as opposed to pension benefits, are afforded an extremely low level of protection under ERISA. Essentially, the employer’s exposure as to promised severance benefits is only as broad as its express contractual commitment to them. By appropriately documenting the benefits with “best practices” language (such as specifying that the amendment or termination of benefits may be done with or without advance notice), employers can take advantage of the opportunity afforded by the relatively thin protections provided by ERISA. On the other hand, poor or no documentation of a severance arrangement may leave an employer with difficult-to-prove assertions as to what severance commitments were actually made.
In summary, an ERISA-governed plan provides an employer with significant advantages in litigation. In addition, a severance arrangement subject to ERISA will enjoy the powerful benefits of ERISA preemption and the ERISA claims procedures.
SOURCE: Rothman, J.; Ninneman, S. (3 October 2018) "Severance plans, Part 1: How savvy employers can stay ERISA compliant" (Web Blog Post). Retrieved from https://www.employeebenefitadviser.com/opinion/how-employers-can-stay-erisa-compliant-with-severance-plans
Business meal deductions likely here to stay after new IRS guidelines
Business meal deductions are expected to continue to qualify for deductions. After much confusion following the IRS’s decision to end deductions for client entertainment, they are expected to release guidance regarding business meal deductions. Read on to learn more.
Employers wondering whether they can still deduct business meals from their tax returns may soon be getting an answer from the Internal Revenue Service.
The agency is expected to release guidance saying that business meals will continue to be 50% deductible, according to an article in the Wall Street Journal.
The confusion over the deductibility of business meals stems from the IRS’s decision to end deductions for client entertainment, a move that was part of the government’s tax overhaul. Previously, the entertainment-related deduction was 50% of qualified expenses.
The elimination of deductions for client entertainment left many tax professionals wondering whether client meals might be considered entertainment and therefore no longer qualify for deductions.
The anticipated IRS guidance — which comes at the urging of the American Institute of Certified Public Accountants and other groups — is expected to preserve the 50% deduction for the cost of meals with clients and elaborate on how the 50% meal write-off meshes with entertainment expenses, the Wall Street Journal said.
If a business owner or employee, for example, takes a client to a ballgame, the cost of the tickets is not deductible because the expense is for entertainment. Hots dogs and drinks purchased at the event, however, could still be 50% deductible, the IRS is expected to say, according to the Wall Street Journal.
The IRS, which did not respond to a request for comment, is not likely to change the normal requirements corporate executives must meet to take deductions for client meals.
They must discuss business with the client before, during and after the meal, and the meal must not be “lavish or extravagant,” the Wall Street Journal said.
SOURCE: Correia, M. (28 September 2018) "Business meal deductions likely here to stay after new IRS guidelines" (Web Blog Post). Retrieved from https://www.benefitnews.com/news/business-meal-deductions-likely-here-to-stay-after-new-irs-guidelines?brief=00000152-14a5-d1cc-a5fa-7cff48fe0001
5 ways benefits educators can ease the open enrollment process
Are you prepared for open enrollment? HR professionals are responsible for effectively communicating plan options and changes to employees so they make informed decisions regarding their coverage and healthcare. Continue reading to learn more.
Open enrollment season is on its way, which means that HR’s already full plate just got a bit fuller. In addition to developing competitive health plans that attract and retain top talent – talent of all ages and with varying needs – HR pros are also responsible for effectively communicating plan options to employees to ensure that individuals make informed, cost-conscious decisions about their coverage and care.
See also: Here’s how HR pros can breeze through open enrollment
As the healthcare landscape becomes more complex, so do employee questions around their health care benefits. Many healthcare consumers today don’t feel comfortable navigating the health care system – which is why most roll over the same plan year after year. While HR teams want to manage the influx of employee questions around their benefits options, they struggle to provide the necessary guidance given their current bandwidth. Covering health plans in a large townhall meeting won’t provide the personalized information that employees need to make educated decisions. To deliver a more personal, empowering experience, organizations can look to benefits educators to supplement strapped HR teams.
Benefits educators can help individuals better understand the plan options available to them and select the package that offers the coverage they need at the price that best fits their budget. To ensure that benefits educators are aligned with the organization’s strategy, HR teams should arrange for educators well in advance of open enrollment so they are equipped to best explain the employer’s benefits plan options. Once up to speed, benefits educators can hold one-on-one conversations with employees to:
1. Define healthcare terms that employees don’t understand. With low healthcare literacy rampant across the U.S., disturbingly few employees are comfortable defining basic health terms such as “deductible,” “copay” or “coinsurance.” benefits educators cannot only explain these important terms but also help employees understand their significance in their coverage selection process.
2. Compare different plans to suit each employee’s needs. Benefits educators will work to understand the specific needs of each employee they meet. By taking the time to sit and get to know each employee, the benefits educator can recommend options that provide the coverage that best meets the needs of the employee and his or her family.
See also: Avoid these 12 Common Open Enrollment Mistakes
Third-party, independent benefits educators can be particularly valuable for employees who do not feel comfortable posing personal questions to their coworkers. By meeting one-on-one with an outsider who understands both benefits in general and company options in particular, employees are often more inclined to raise specific health or personal details that should guide their benefits selection. In fact, 45 percent of employees say they would prefer to speak to a benefits expert when choosing their coverage.
3. Equip employees with the information they need to choose their coverage. Left to their own devices, 83 percent of employees spend less than an hour reviewing their plan options before open enrollment – a lack of preparation that does not bode well for educated benefits selection. benefits educators can focus on the details that matter – saving the employee time and effort.
4. Explain voluntary benefits. Despite the increasing popularity of voluntary benefits, many employees are still confused about what they are, how they work and why they might be helpful. In reality, certain voluntary benefits can help control health costs and bridge the gap between medical coverage and out-of-pocket costs – added expenses that concern 61 percent of employees. In today’s multigenerational workforce – where employees have very different priorities when it comes to their health and financial wellness – benefits educators can dispel some of the mystery and suggest options that might meet individual needs.
5. Empower employees to make the most of their benefits year-round. Benefits educators can lay the groundwork for more educated health care consumers by directing employees to resources where they can find more information about their coverage and how their plans work after the open enrollment ends.
See also: 5 tips to make this the best open enrollment ever
More informed employees not only make smarter choices about their coverage and care but also better appreciate their employers – which has the potential to help with retention and business productivity. Ultimately, organizations see a win-win-win: happier employees who save on care, happier HR teams who save on time and happier executives, who see a significant return on their health care investments.
SOURCE: Murdock, G (21 September 2018) "5 ways benefits educators can ease the open enrollment process" (Web Blog Post). Retrieved from https://www.benefitspro.com/2018/09/21/5-ways-benefits-educators-can-ease-the-open-enroll/