Obesity drives up workers’ comp claims
Originally posted November 21, 2013 by Dan Cook on https://www.benefitspro.com
Obese employees make more workers’ comp claims, and they make costlier ones than non-obese employees.
That conclusion was drawn by Lockton Companies based on its review of several independent studies on employees with high health risks (including obesity, smoking, high blood pressure and limited physical activity) and workers’ comp claims.
The Kansas City, Mo., provider of risk management, insurance, and employee benefits consulting services cites three studies that, when taken together, paint a troubling picture, especially of the impact overweight workers can have on workers’ comp claims.
Lockton says that wellness programs, properly designed and implemented, can address this situation by helping obese workers lose weight. But Lockton doesn’t offer any stats on how effective wellness programs are overall in combating obesity.
Still, the studies cited offer food for thought.
The University of Michigan Health Management Research Center studied Xerox Corp. employees and confirmed that “employees with high health risks tended to have the highest workers’ compensation costs.”
Xerox was an early proponent of wellness plans. The UM followed employees for four years and reported that “workers’ compensation costs increased for those employees whose health risks were increasing or high already (e.g., smoking, physical inactivity, hypertension, high cholesterol, and life/job dissatisfaction).”
Lockton also refers to a 2010 study by the National Council on Compensation Insurance which more closely correlated obesity with workers’ comp claims.
The data “showed that workers’ compensation claims that included the obesity comorbidity diagnosis incurred significantly higher medical costs than comparable claims without the high health risk. NCCI also discovered that claims for employees identified
as “obese” almost tripled from 2000 to 2009 from 2.4 percent to 6.6 percent,” Lockton said.
Lockton then cites a more recent NCCI study testing whether “the lost-time duration of obese claimants is a multiple of non-obese claimants.”
It was.
“According to their findings, obese claimants incurred medical costs 6.8 times higher than non-obese (as defined by body mass index), were twice as likely to file a claim and an indemnity duration that averaged about 13 times higher,” Lockton summarized.
What Lockton suggests is that companies take the following steps to empower their wellness plans to really help employees address chronic health issues:
- Proactively engage HR and employee benefits to better understand the scope and breadth of existing corporate wellness initiatives, as well as how the organization is tracking the effectiveness of those programs.
- Determine how your insurer and/or third party administrator is capturing data on comorbid factors in workers’ compensation claim files and how that information can be incorporated into effective analytics.
- Collaborate with internal safety, health, and environment professionals (if applicable) to discover how best to integrate employee wellness with workplace safety.
“Effective corporate wellness initiatives have shown to be successful in not only reducing the duration of lost-time workers' compensation claims,” said Lockton's Michal Gnatek, author of the report, “but also in promoting healthy behaviors that potentially inhibit unsafe or inattentive workplace behavior.
“Risk managers and claims professionals should be adding employee wellness to the available arsenal of weapons to combat increasing claims.”
Doctors urged to treat obesity like any other ailment; New guidelines say do whatever it takes to get the pounds off
Originally posted November 13, 2013 by Nanci Hellmich on www6.lexisnexis.com
There's no ideal diet that's right for everyone, but that shouldn't stop the nation's doctors from helping their heavy patients battle weight issues as aggressively as things like blood pressure, according to new obesity treatment guidelines released Tuesday.
The guidelines, from three leading health groups, say that doctors need to help obese patients figure out the best plan, whether it's a vegetarian diet, low-sodium plan, commercial weight-loss program or a low-carb diet.
Still, the most effective behavior-change weight-loss programs include two to three in-person meetings a month for at least six months, and most people should consume at least 500 fewer calories a day to lose weight, the recommendations say.
The guidelines are designed to help health care providers aggressively tackle the obesity epidemic. "The overall objective is quite a tall order: to get primary care practitioners to own weight management as they own hypertension management," says obesity researcher Donna Ryan, co-chairwoman of the committee writing these guidelines for the Obesity Society, American Heart Association and American College of Cardiology.
The recommendations are part of a set of heart disease prevention guidelines released Tuesday.
Nearly 155 million U.S. adults are overweight or obese, which is roughly 35 pounds over a healthy weight. Extra pounds put people at a higher risk of heart disease, stroke, many types of cancer, type 2 diabetes and a host of other health problems.
Health care providers should encourage obese and overweight patients who need to drop pounds for health reasons to lose at least 5% to 10% of their weight by following a moderately reduced-calorie diet suited to their food tastes and health status, while being physically active and learning behavioral strategies.
"The gold standard is an intervention delivered by trained interventionists (not just registered dietitians or doctors) for at least 14 sessions in the first six months and then continue therapy for a year," says Ryan, a professor emeritus at the Pennington Biomedical Research Center in Baton Rouge. If this kind of intensive therapy is not available, then other types of treatment, such as commercial weight-loss programs or telephone and Web-based programs, are good "second choices," she says.
Medicare began covering behavioral counseling for obese patients last year, and under the Affordable Care Act, most private insurance companies are expected to cover behavioral counseling and other obesity treatments by next year.
"There is no ideal diet for weight loss, and there is no superiority between the many diets we looked at," Ryan says. "We examined about 17 different weight-loss diets."
Pat O'Neil, director of the Weight Management Center at Medical University of South Carolina, says, "The diet you follow is the one that's going to work for you. That's good information for the public to have."
The report advises health care providers to calculate body mass index (a number that takes into account height and weight) at annual visits or more frequently, and use it to identify adults who may be at a higher risk of heart disease and stroke. Evidence shows that the greater the BMI, the higher the risk of coronary heart disease, stroke, type 2 diabetes and death from any cause, the report says. "BMI is a quick and easy first step," Ryan says.
The guidelines are being published simultaneously in Circulation, a journal of the American Heart Association; the Journal of the American College of Cardiology; and Obesity: Journal of the Obesity Society.
U.S. Obesity Rate Climbing in 2013
Originally posted November 1, 2013 by Lindsey Sharpe on https://www.gallup.com
WASHINGTON, D.C. -- The adult obesity rate so far in 2013 is 27.2%, up from 26.2% in 2012, and is on pace to surpass all annual average obesity rates since Gallup-Healthways began tracking in 2008.
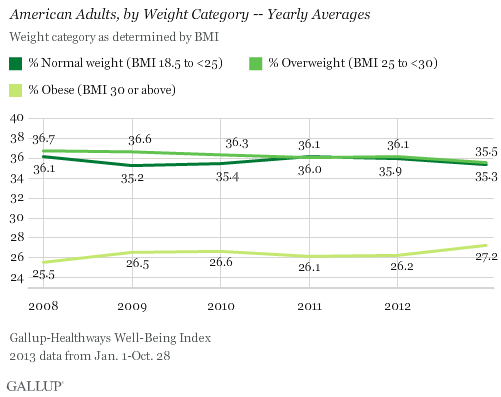
The one-percentage-point uptick in the obesity rate so far in 2013 is statistically significant and is the largest year-over-year increase since 2009. The higher rate thus far in 2013 reverses the lower levels recorded in 2011 and 2012, and is much higher than the 25.5% who were obese in 2008.
The increase in obesity rate is accompanied by a slight decline in the percentage of Americans classified as normal weight or as overweight but not obese. The percentage of normal weight adults fell to 35.3% from 35.9% in 2012, while the percentage of adults who are overweight declined to 35.5% from 36.1% in 2012. An additional 1.9% of Americans are classified as underweight in 2013 so far.
Since 2011, U.S. adults have been about as likely to be classified as overweight as normal weight. Prior to that, Americans were most commonly classified as overweight.
Gallup and Healthways began tracking Americans' weight in 2008. The 2013 data are based on more than 141,000 interviews conducted from Jan. 1 through Oct. 28 as part of the Gallup-Healthways Well-Being Index. Gallup uses respondents' self-reported height and weight to calculate body mass index (BMI) scores. Individual BMI values of 30 or above are classified as "obese," 25 to 29.9 are "overweight," 18.5 to 24.9 are "normal weight," and 18.4 or less are "underweight."
Obesity Rates Increase Across Almost All Demographic Groups
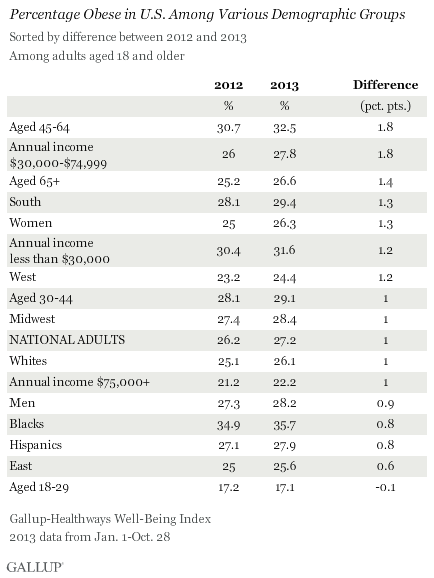
Obesity rates have increased at least slightly so far in 2013 across almost all major demographic and socioeconomic groups. One exception is 18- to 29-year-olds, among whom the percentage who are obese has remained stable. The largest upticks between 2012 and 2013 were among those aged 45 to 64 and those who earn between $30,000 and $74,999 annually. The obesity rate within both groups increased by 1.8 points, which exceeds the one-point increase in the national average.
At 35.7%, blacks continue to be the demographic group most likely to be obese, while those aged 18 to 29 and those who earn over $75,000 annually continue to be the least likely to be obese.
Bottom Line
The U.S. obesity rate thus far in 2013 is trending upward and will likely surpass all annual obesity levels since 2008, when Gallup and Healthways began tracking. It is unclear why the obesity rate is up this year, and the trend since 2008 shows a pattern of some fluctuation. This underscores the possibility that that the recent uptick is shorter-term, rather than a more permanent change. Still, if the current trend continues for the next several years, the implications for the health of Americans and the increased burden on the healthcare system could be significant.
Blacks, those who are middle-aged, and lower-income adults continue to be the groups with the highest obesity rates. The healthcare law could help reduce obesity among low-income Americans if the uninsuredsign up for coverage and take advantage of the free obesity screening and counseling that most insurance companies are required to provide under the law.
Employers can also take an active role to help lower obesity rates. Gallup has found that the annual cost for lost productivity due to workers being above normal weight or having a history of chronic conditions ranges from $160 million among agricultural workers to $24.2 billion among professionals. Thus, employers can cut healthcare costs by developing and implementing strategies to help workers maintain or reach a healthy weight.
Gallup has also found that employees who are engaged in their work eat healthier and exercise more. Therefore, employers who actively focus on improving engagement may see healthier and more productive workers, in addition to lower healthcare costs.
About the Gallup-Healthways Well-Being Index
The Gallup-Healthways Well-Being Index tracks well-being in the U.S. and provides best-in-class solutions for a healthier world. To learn more, please visit well-beingindex.com.
Results are based on telephone interviews conducted as part of the Gallup-Healthways Well-Being Index survey Jan. 1-Oct. 28, 2013, with a random sample of 141,935 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
For results based on the total sample of national adults, one can say with 95% confidence that the margin of sampling error is ±0.5 percentage points.
Interviews are conducted with respondents on landline telephones and cellular phones, with interviews conducted in Spanish for respondents who are primarily Spanish-speaking. Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by region. Landline and cellphone numbers are selected using random-digit-dial methods. Landline respondents are chosen at random within each household on the basis of which member had the most recent birthday.
Samples are weighted to correct for unequal selection probability, nonresponse, and double coverage of landline and cell users in the two sampling frames. They are also weighted to match the national demographics of gender, age, race, Hispanic ethnicity, education, region, population density, and phone status (cellphone only/landline only/both, and cellphone mostly). Demographic weighting targets are based on the March 2012 Current Population Survey figures for the aged 18 and older U.S. population. Phone status targets are based on the July-December 2011 National Health Interview Survey. Population density targets are based on the 2010 census. All reported margins of sampling error include the computed design effects for weighting.
In addition to sampling error, question wording and practical difficulties in conducting surveys can introduce error or bias into the findings of public opinion polls.
For more details on Gallup's polling methodology, visit www.gallup.com.
Bike and health expert advocates collaborative approach to wellness
Originally posted September 25, 2013 by Kathleen Koster on https://ebn.benefitnews.com
The workplace strategy for health improvement is easily expressed as a bicycling metaphor where bicyclists struggle with the uphill stretches and use caution to coast on downward slopes. Gary Earl, former vice president of benefits and health care for Caesars Entertainment Corporation, suggested employers could learn from the biking world when improving their wellness strategy, speaking during a panel discussion at the Benefits Forum & Expo in New Orleans on Monday.
“Our job [as HR professionals] is to improve the lives of human beings. We’re responsible for that,” explained Earl, founder and team captain of Journey for Health Tour, for which Earl and his team are riding a bicycle 3,000 miles across America to promote health improvement.
While working for Caesars, Earl transformed the company’s outlook on wellness programs and health benefits from a cost-only perspective to an asset for the workforce and business.
“[My employer’s] vision was the traditional vision: to offer affordable benefit plans to employees and to reduce costs. We turned that upside down. We wanted to move it from an expense to an asset,” he said.
He created an affordable equation to prove his strategy would improve the population’s health by developing a mathematic equation to show company executives the value in this paradigm shift.
That equation illustrated how employees’ positive health experience and positive attitude generates an increase in productivity, sustainability and satisfaction, which would lead to an improvement in company earnings.
“We have to look at health benefits as an opportunity, an asset,” Earl stressed.
Earl believes HR and benefits professionals need to hold themselves accountable to improving population health and always passionately advocate wellness—not simply view this responsibility as part of a dry job description.
Over time, we have created the problems afflicting our health system and it’s our responsibility as a community to fix today’s prevalent issues, said Dr. David Whitehouse, MD, chief medical officer, UST GLOBAL, a fellow panelist at the conference session.
“The ecosystem of health and the obesity endemic exist because of modernization. During World War II there were food shortages and we developed preservatives [to make our food last longer]. We then wanted to make our lives more convenient, so we developed transport and we stopped exercising and walking. We have, in fact, through modernization and our own design for comfort, created the epidemic,” said Whitehouse.
Earl seconded that point, adding that these health issues “can’t be viewed in isolation. They are systematic problems, which means that they are interconnected and interrelated. We need to approach this by connecting all aspects of the community, whether it’s faith, safety, education, business or economic development—there’s a real balance to be able to draw them all together.”
He added that business owners could drive this change. “They don’t own that change but they can be a catalyst. By coming together in uncommon ways but for a common purpose stimulates the change,” he said.
Employers and company leaders must connect with communities to make significant change. Applying the bike metaphor again, Earl said that we need to encourage each other when facing uphill challenges and learn from one another to find solutions. And for those downhill stretches, Earl explained that in biking, “you don’t ever coast downhill; you want to keep that leg-mind momentum going.” Employers must also use caution to stay in control of their initiatives and keep forward momentum, without swerving off the edge of the road.
“You’re not going to improve an individual’s health without understanding what those social and environmental elements are,” Earl said. “You have to put in the energy.”
Employers can align medical groups and local systems by working with the community. They can make a customized approach through patient-centered medical homes, on-site clinics or Accountable Care Organizations. Whatever employers develop with their local groups, they must work together to fix the dramatic health issues Americans face and struggle with.
“If we don’t overcome our shyness and work collaboratively then we will live with the misfortunes of our unintended consequences,” said Whitehouse.
Obesity’s disease label could spell trouble for employers
Originally posted by Andrea Davis on https://ebn.benefitnews.com
Earlier this year, the American Medical Association deemed obesity a disease. AMA board member Patrice Harris, M.D., said in a statement that “recognizing obesity as a disease will help change the way the medical community tackles this complex issue that affects approximately one in three Americans.”
While there is still debate within the medical community as to whether obesity is a disease — the AMA’s own House of Delegates recommended the body not adopt the resolution declaring it a disease — there is speculation the AMA’s decision could open the door to more discrimination claims under the American with Disabilities Act.
EBN spoke to Jay Starkman, CEO of Engage PEO, about the AMA classification of obesity and how it might affect employer decisions.
What are the implications for employers?
Employers need to treat obese individuals like they would anybody else with a disability. … There was always an issue about whether or not an obese person was disabled under the Equal Employment Opportunity Commission guidelines. [Under the] ADA, “disability” is defined as an impairment that substantially limits a major life activity. … but there was always a question about whether or not obesity was one of those things.
One of the issues that existed for a long time was whether or not there needed to be some type of underlying disorder that caused the obesity, whether psychological or physical. By classifying obesity as a disease, it’s pretty clear that whether or not there’s an underlying disorder isn’t going to be a relevant inquiry any more. So that means that employers can’t make hiring decisions — hiring, firing, promotions, raises, compensation — based upon whether or not someone is obese.
Do employers need to consider any changes to their current employee policies?
The first is make sure you have very clear job descriptions — before hiring — that lay out any physical requirements of a position. The second thing is, if somebody is disabled, [because of] obesity or whatever, if it is possible to make a reasonable accommodation for them, that needs to be done.
What else might be important for employers to know?
The definition of “obese” is really in flux right now. A lot of the EEOC cases that existed prior to the AMA coming out with this defined it as “severely” obese or “morbidly” obese. … So nobody is sure what will constitute a disability, because the number of people that are 20% overweight in America is far different than the one for people that are double the standard weight. So I just think that it needs to be a very serious concern in people’s minds.
Authors expose obesity myths
Source: https://www.benefitspro.com
By Marilyn Marchione
Fact or fiction? Sex burns a lot of calories. Snacking or skipping breakfast is bad. School gym classes make a big difference in kids' weight.
All are myths or at least presumptions that may not be true, say researchers who reviewed the science behind some widely held obesity beliefs and found it lacking.
Their report in Thursday's New England Journal of Medicine says dogma and fallacies are detracting from real solutions to the nation's weight problems.
"The evidence is what matters," and many feel-good ideas repeated by well-meaning health experts just don't have it, said the lead author, David Allison, a biostatistician at the University of Alabama at Birmingham.
Independent researchers say the authors have some valid points. But many of the report's authors also have deep financial ties to food, beverage and weight-loss product makers — the disclosures take up half a page of fine print in the journal.
"It raises questions about what the purpose of this paper is" and whether it's aimed at promoting drugs, meal replacement products and bariatric surgery as solutions, said Marion Nestle, a New York University professor of nutrition and food studies.
"The big issues in weight loss are how you change the food environment in order for people to make healthy choices," such as limits on soda sizes and marketing junk food to children, she said. Some of the myths they cite are "straw men" issues, she said.
But some are pretty interesting.
Sex, for instance. Not that people do it to try to lose weight, but claims that it burns 100 to 300 calories are common, Allison said. Yet the only study that scientifically measured the energy output found that sex lasted six minutes on average — "disappointing, isn't it?" — and burned a mere 21 calories, about as much as walking, he said.
That's for a man. The study was done in 1984 and didn't measure the women's experience.
Among the other myths or assumptions the authors cite, based on their review of the most rigorous studies on each topic:
—Small changes in diet or exercise lead to large, long-term weight changes. Fact: The body adapts to changes, so small steps to cut calories don't have the same effect over time, studies suggest. At least one outside expert agrees with the authors that the "small changes" concept is based on an "oversimplified" 3,500-calorie rule, that adding or cutting that many calories alters weight by one pound.
—School gym classes have a big impact on kids' weight. Fact: Classes typically are not long, often or intense enough to make much difference.
—Losing a lot of weight quickly is worse than losing a little slowly over the long term. Fact: Although many dieters regain weight, those who lose a lot to start with often end up at a lower weight than people who drop more modest amounts.
—Snacking leads to weight gain. Fact: No high quality studies support that, the authors say.
—Regularly eating breakfast helps prevent obesity. Fact: Two studies found no effect on weight and one suggested that the effect depended on whether people were used to skipping breakfast or not.
—Setting overly ambitious goals leads to frustration and less weight loss. Fact: Some studies suggest people do better with high goals.
Some things may not have the strongest evidence for preventing obesity but are good for other reasons, such as breastfeeding and eating plenty of fruits and vegetables, the authors write. And exercise helps prevent a host of health problems regardless of whether it helps a person shed weight.
"I agree with most of the points" except the authors' conclusions that meal replacement products and diet drugs work for battling obesity, said Dr. David Ludwig, a prominent obesity research with Boston Children's Hospital who has no industry ties. Most weight-loss drugs sold over the last century had to be recalled because of serious side effects, so "there's much more evidence of failure than success," he said.
Obese People Can Be Healthy
BY KATHRYN MAYER
Source: benefitspro.com
Here’s some news to justify having (and not caring about) some extra pounds: Being fat doesn’t necessarily mean you’re unhealthy.
New research finds that people can be obese yet physically healthy, while having no greater risk for heart disease or cancer than people of normal weight.
“It is well known that obesity is linked to a large number of chronic diseases such as cardiovascular problems and cancer. However, there appears to be a sub-set of obese people who seem to be protected from obesity-related metabolic complications,” lead study author Francisco Ortega said in a statement. “They may have greater cardio-respiratory fitness than other obese individuals, but, until now, it was not known the extent to which these metabolically healthy but obese people are at lower risk of diseases or premature death.”
Researchers analyzed data from 43,265 participants in the Aerobics Center Longitudinal Study, which was done between 1979 and 2003.
About 30 percent of the study participants were labeled obese. Of the obese, nearly half were considered “metabolically healthy.” Metabolic health is determined by several factors including high blood pressure, high triglycerides, low HDL cholesterol and high fasting glucose levels.
Researchers found that the metabolically healthy but obese participants had a 38 percent lower risk of dying than their metabolically unhealthy peers. There was also no risk difference between the metabolically healthy obese and the metabolically healthy normal weight participants.
The results were published this week in the European Heart Journal.
"Physicians should take into consideration that not all obese people have the same prognosis,” Ortega said. “Physicians could assess fitness, fatness and metabolic markers to do a better estimation of the risk of cardiovascular disease and cancer of obese patients. Our data support the idea that interventions might be more urgently needed in metabolically unhealthy and unfit obese people, since they are at a higher risk. This research highlights once again the important role of physical fitness as a health marker.”
Learn How Inflammation Can Lead to Chronic Diseases
By Dr. Ann Kulze, M.D.
Inflammation is now widely recognized as a primary driver for most all chronic diseases and it appears that losing even modest amounts of weight can effectively douse the damaging inferno of excess inflammation in the body. For this one year evaluation, 438 women were placed on a weight loss program through diet or diet and exercise. For women in the diet and exercise group, measures of C-reactive protein (a key marker for inflammation in the body) dropped 42%. In the diet only group, levels dropped by 36 percent. For both groups, losing just 5% of their initial body weight provided even larger reductions in C-reactive protein. Because higher levels of C-reactive protein have been linked to a litany of chronic diseases including heart disease, type 2 diabetes, and cancers of the breast, colon, lung and uterus, this study underscores the enormous benefits that can result from losing even small amounts of excess body fat.
Joggers Rejoice!
Source: Dr. Ann Kulze
May 2012 Newsletter
Wellness Delivered Pure and Simple
In a stunning affirmation of the profound health-boosting effects of regular physical activity, European Cardiovascular researchers concluded that regular jogging can dramatically increase life expectancy. As part of the Copenhagen City Heart Study, investigators followed 19,329 adult study subjects over a period of up to 35 years. Study subjects who reported regular jogging at a "slow or average" pace were 40% less likely to die over the study period than non-joggers and increased their life expectancy by an average of 6 years. What's more, regular joggers also reported an enhanced sense of overall well-being.
Based on this evaluation, maximum survival benefits were seen in those who jogged between one to two and a half hours a week over two to three sessions. Thankfully, there are numerous types of aerobic activities that get the heart rate into this "jogging zone". According to the lead investigator, the goal is to move to the point of "feeling a little breathless, but not very breathless". (1)
Are Chubby Workers Eating You Out of Profits?
Source: https://safetydailyadvisor.blr.com
OSHA recordkeeping and reporting requirements appear straightforward, but the devil is in the details. Pound for pound, obese workers cost you plenty. Here are some facts that should disturb you.
| Which employee health issue costs employers more, obesity or smoking?
If you guessed obesity, you guessed right. A study in the Journal of Occupational and Environmental Medicine analyzed the additional costs of smoking and obesity among more than 30,000 Mayo Clinic employees and retirees. All had continuous health insurance coverage between 2001 and 2007. Both obesity and smoking were associated with excess health costs. Compared to nonsmokers, average health costs were $1,275 higher for smokers. And obese people averaged an additional $1,850 more than normal-weight individuals. For those with morbid obesity, costs were up to $5,500 per year. Clearly obesity is an issue that most employers will need to deal with in the future. Americans are becoming fatter every year, and that means increasing health problems and increasing health costs. Since many of these obese people work, employers will be impacted by increasing medical costs and lost productivity. Great news! BLR's renowned Safety.BLR.com® website now has even more timesaving features. Take our no-cost site tour! Or better yet, try it at no cost or obligation for a full 2 weeks. Facts and FiguresHere are some other statistics that paint a worrisome picture: • Annual healthcare cost of obesity in the U.S. is estimated to be $147 billion per year. • Annual medical burden of obesity increased to 9.1 percent in 2006 compared to 6.5 percent in 1998. • Medical expenses for an obese employee are estimated to be 42 percent higher than for employees with a healthy weight. • Three major conditions related to obesity (heart disease, diabetes and arthritis) cost employers $220 billion annually in medical cost and lost productivity, according to CDC and MetLife research. • An American Journal of Health Behavior study showed that the annual medical cost increased from $119 for normal-weight employees to $573 for overweight employees and to $620 for obese employees. • A MetLife study found that the average absence for employee who filed an obesity-related short-term disability claim was 45 days. • A 1998 study found obesity resulted in approximately 39 million lost work days, 239 million restricted-activity days, 90 million bed days and 63 million physician visits. • Obese employees have double workers’ compensation claims, 7 times higher medical claims, and lost 10 times more working days from illness or injury compared to non-obese employees, according to the Duke University Medical Center. Who's Obese?Obesity is defined as at least 30 to 40 pounds overweight, severely obese is at least 60 pounds overweight, and morbidly obese is at least 100 pounds overweight. Obesity can increase the risk for many adverse health effects, including: · Type-2 diabetes · Hypertension · Heart failure · High cholesterol · Kidney failure · Degenerative joint disease and arthritis · Gallstones and gall bladder disease · Cancer · Lung and breathing problems (asthma) · Faster aging |
