Employers can help in cancer prevention, treatment
Originally posted November 20, 2013 by Andy Stonehouse on https://ebn.benefitnews.com
A cancer diagnosis is not just a life-changing event for an employee and his or her family, it’s also increasingly become a gigantic consideration in the overall costs of employer-sponsored insurance plans.
Learning to cope with treatment – or even the time or alternative work arrangements required for an employee helping a loved one dealing with cancer – can be a challenge for any HR professional, but a new guide hopes to provide better understanding and also offer some broader cancer prevention suggestions for America’s workers.
The National Business Group on Health’s An Employer’s Guide to Cancer Treatment and Prevention, released Nov. 20, represents three years of work with the National Comprehensive Cancer Network on strategies and standards to help cope with the ever-increasing social and financial cost of cancer treatment.
NBGH notes that cancer treatment, one of the top three conditions dealt with on a national level, ends up consuming approximately 12% of total medical expenses, across the board; as well, nearly a quarter of employees end up taking time in a caregiving role to family members dealing with cancer treatment of their own.
In practical terms, NBGH’s new guide can help employers set up, implement and then measure the success of a variety of cancer-related strategies.
Lynn Zonakis, managing director of health strategy and resources at Delta Air Lines, Inc., says her company has taken similar efforts to more effectively address the reality of cancer issues in the workplace – an important venue for discussing a disease with such a broad impact.
“Employers can play a major role in keeping workers healthy and also supporting cancer patients during treatment and return to work,” Zonakis says. “Large employers, especially, have the ability to specifically design health benefits to their workforce. This three-year project has certainly helped shape Delta’s approach and commitment to addressing cancer in the workplace.”
For Delta, that’s included initiatives such as full coverage for recommended cancer screenings, a Centers of Excellence program and even Delta Health Direct, a specialized concierge service which provides confidential access to coaching, a nurse line, disease support and even suggestions on treatment decision-making.
The Employer’s Guide offers six tools that have been developed based on recommendations from the NCCN’s Clinical Practice Guidelines in Oncology, each coinciding with the entire planning and rollout of a full employer benefit program: plan design, enrollment, plan administration and evaluation.
The guide also offers insight on the broader issues in cancer care, ranging from medical, pharmacy and behavioral benefits to the best utilization of short-term disability, family medical leave and employee assistance programs.
“With significant gains in cancer survival rates and most cancer survivors staying at work during their treatment or returning to work after their treatment, employers need a comprehensive benefits plan to ensure that their current strategies to address cancer in the workplace complement the needs of their employees,” says Helen Darling, president and CEO of the NBGH.
’Tis the Season for a Slice of Wellness Training
Originally posted November 29, 2013 by Chris Kilbourne on https://safetydailyadvisor.blr.com
At the beginning of this year's holiday season, take a moment to remind your employees that good nutrition is important to good health. Use the video in today's Advisor as a concise and fun way to drop nutrition reminders in among the holiday festivities.
In order to get the nutrition they need every day to stay healthy, employees must develop and maintain healthy eating habits. Here's a video that takes a light-hearted approach toward providing facts about nutrition and the important employee wellness topic of having healthy eating habits.
https://www.youtube.com/watch?v=Hv66ItR_F24&feature=player_embedded
I'm sure you’ve heard that good nutrition is important to good health. But how?
Well, good nutrition helps you in many important ways. For example, eating healthy food helps to prevent diseases like heart disease, diabetes, and high blood pressure and maintain a healthy weight.
In order to get the nutrition you need every day to stay healthy, you must develop and maintain healthy eating habits. Unfortunately, many Americans have very unhealthy eating habits.
Healthy eating means eating three nutritious meals a day, consuming reasonable portion sizes, limiting intake of fat, sugar, and salt, snacking sensibly between meals, avoiding fad diets, and balancing calorie intake with physical activity.
Proper nutrition depends on a well-balanced diet that includes carbohydrates, fiber, protein, and some unsaturated fat. Carbohydrates give your body the energy it needs to function effectively all day. Carbohydrates are found in fruits, vegetables, bread, cereal, pasta, rice, and milk and milk products. In fact, 45 percent to 65 percent of your daily calorie intake should come from carbohydrates. You also need about 14 grams of dietary fiber for every 1,000 calories you eat. Protein is another essential nutrient, and you should get 10 percent to 35 percent of daily calories from proteins.
Most Americans eat more protein than they really need to stay healthy. Protein is found in meat, poultry, fish, eggs, nuts, milk and milk products, grains, and some vegetables and fruits.
Some protein-rich foods such as meat are also high in fat and cholesterol. To keep healthy, you should consume less than 10 percent of your daily calorie intake as fat. Most of your fat intake should be unsaturated, as opposed to saturated, fat. Saturated fat is found in foods such as high-fat cheese, high-fat meat, butter, and ice cream.
Nuts, vegetable oil, and fish are good sources of poly- and monounsaturated fats.
Health experts also say you should consume less than 300 milligrams of cholesterol a day. Cholesterol is a fatty substance found in animal-based foods such as meat, eggs, and whole milk.
Sugar is found naturally in foods such as fruits, vegetables, and milk and milk products. Some foods include added sugar, and these foods are less nutritious than foods containing only natural sugar. To keep healthy, try to avoid added sugar, which provides no nutritional value and also contributes to tooth decay.
Also, remember that fluids, vitamins, and minerals are part of good nutrition, too. You need about eight glasses of water or other low-sugar fluids a day.
Finally, even though you've got a lot of great choices here in your fridge, I'm sure you eat out sometimes. When you do, remember to make healthy choices. Restaurant or takeout food can be high in fat, sugar, and salt, and low in required nutrients. When you eat food prepared outside your home, try to pick lower-fat foods, choose smaller portions, go broiled or baked instead of fried, order a vegetables or salad, and skip dessert.
For more information on nutrition, visit www.blr.com. Here you’ll find lots of information on wellness. BLR® specializes in employee training, so be sure to check out all of their employee wellness training resources as well as other training topics.
Why It Matters
- Giving your employees nutrition information can help keep them healthy and on the job.
- Healthy employees will cut down on your sick leave costs and your healthcare insurance expenses.
- Healthy employees who are eating the right balance of nutritious foods are more likely to be more productive as well.
- The bottom line is that a healthy amount of wellness training can provide a healthy return on investment for your organization.
Nuts for longevity: Daily handful is linked to longer life
Originally published November 21, 2013 by Allison Aubrey on https://www.npr.org
Nuts might be loaded with fat but evidence suggests they could help you live longer. A diet study found earlier this year that a diet with daily portions of nuts and olive oil reduced the risks of heart attacks and strokes. Recent evidence found that nuts can help control appetite, which could reduce weight gain.
Americans have not always been in love with nuts.
Think about it: They're loaded with calories and fat. Plus, they can be expensive.
But Americans' views — and eating habits — when it comes to nuts are changing. Fast.
There's a growing body of scientific evidence that's putting a health halo over supermarkets' expanding nut aisles.
Earlier this year, a large diet study concluded that people who eat a Mediterranean-style diet supplemented with daily portions of nuts and olive oil have significantly lower risks of heart attacks and strokes.
And just last month, more evidence emerged that snacking on nuts helps control our appetites, which may stave off weight gain.
Now, a new study published in the New England Journal of Medicine finds that people in the habit of eating a daily handful (a 1-ounce serving) of nuts are more likely to live longer compared with people who rarely consume nuts.
"The preponderance of evidence suggests a health benefit [from eating nuts]," says researcher Charles Fuchs of the Dana-Farber Cancer Institute and Harvard Medical School.
To isolate the association between nut consumption and lifespan, Fuchs and his colleagues combined data from two long-term studies that include about 76,000 women and 42,000 men.
The participants in the study completed food frequency surveys every two to four years over several decades. They answered all kinds of questions about dozens of different kinds of foods, including how many servings of nuts they consumed.
"What we find is that regular nut consumers have about a 20 percent reduction in all-cause mortality" over the course of the study, Fuchs says. This includes lower death rates from heart disease and cancer.
Now, since death is inevitable for all of us, here's another way to think about the findings: Men and women who were regularly munching on peanuts or tree nuts like almonds, pecans and walnuts in their 30s and 40s when the study began were significantly more likely to reach their 70s, compared with folks who didn't eat nuts.
So how could a daily handful of nuts possibly be so beneficial? Fuchs says it's not entirely clear.
"What we think nuts do is that they affect metabolism," he explains. Prior research has shown that nuts help us feel fuller, faster. And nuts also help control blood sugar.
Fuchs says if nuts lead to a sense of satiety and help people eat less, many of the other benefits may follow. This could "reduce the risk of diabetes and also reduce the risk of cardiovascular disease," he says.
Of course, this study does not prove a cause and effect between eating nuts and living longer. The design of this type of long-term, observational study only enables researchers to establish an association — a link.
Going forward, researchers want to try to better understand what might explain this link. They want to know more about how the combination of beneficial plant compounds and minerals — such as magnesium, fiber and protein — found in nuts may be influencing the body.
With all the good news about nuts in the news, experts who track food trends say more Americans are eating them.
"Nuts are in the perfect spot right now," says John Frank of Mintel. The market research firm estimates that sales of nuts and dried fruit in the U.S. will grow from about $7 billion in annual sales in 2012 to over $9 billion by 2017.
Nuts check a lot of boxes that young adults are looking for: They're high in protein, they're easy to grab and eat on the go, and they're a natural, plant-based food.
"I'm a vegetarian, so nuts are an important part of my diet, for added protein," shopper Emily Williams told me as she added nuts to her shopping cart at a Trader Joe's in Washington, D.C.
Many grocery stores' expanding nut aisles now include lots of variety — everything from dark-chocolate-covered almonds to spicy, Asian-flavor-infused nuts.
And Frank says millennials love the variety. Young adults aren't just snacking on nuts — increasingly, they're tossing them in salads and sprinkling them in yogurt and cereal.
One note about the NEJM study on nuts: The major part of the study was funded by the National Institutes of Health. The researchers also accepted a grant from the International Tree Nut Council Nutrition Research and Education Foundation to cover the cost of analyzing the data.
"The [nut] council approved the grant without any knowledge of the results," says Fuchs. And there was an agreement that the researchers would have reported the findings no matter what the results showed.
The Great American Smokeout Day is Today
Originally posted on https://www.cancer.org
The American Cancer Society marks the Great American Smokeout on the third Thursday of November each year by encouraging smokers to use the date to make a plan to quit, or to plan in advance and quit smoking that day. By quitting — even for one day — smokers will be taking an important step towards a healthier life – one that can lead to reducing cancer risk.
This year, we’re celebrating quitters and their supporters with a series of fun characters designed for social sharing on Facebook, Twitter and Pinterest. We’ve also got lots of other resources and information to help you quit for good.
Have a question about how to quit smoking? Want to know how lawmakers can help in the fight against tobacco use? Sharecare & the American Cancer Society team up to host a Great American Smokeout Twitter Chat. On Wednesday, Nov. 20 and Thurs. Nov 21, ask your question on Twitter and Facebook using the hashtag #quitforgood. Go online Thurs, Nov 21, 11 am to 4 pm EST to see the answers roll in from the American Cancer Society and other experts!
Get tips on how to kick your smoking habit during the American Cancer Society’s Great American Smokeout on Thursday, Nov. 21st from 1-2pm ET during Everyday Health’s #HealthTalk: https://www.everydayhealth.com/healthtalk/great-american-smokeout.aspx
Tobacco use remains the single largest preventable cause of disease and premature death in the US, yet about 43.8 million Americans still smoke cigarettes — Nearly 1 in every 5 adults. As of 2010, there were also 13.2 million cigar smokers in the US, and 2.2 million who smoke tobacco in pipes — other dangerous and addictive forms of tobacco.
Why Quit?
The health benefits of quitting start immediately from the moment of smoking cessation. Quitting while you are younger will reduce your health risks more, but quitting at any age can give back years of life that would be lost by continuing to smoke. View sources.
More Information About Quitting
Quitting is hard, but you can increase your chances of success with help. The American Cancer Society can tell you about the steps you can take to quit smoking and provide quit-smoking programs, resources and support that can increase your chances of quitting successfully. To learn about the available tools, call us at 1-800-227-2345. You can also find free tips and tools below.
- Guide to Quitting Smoking
- What are the Benefits of Quitting?
- Desktop Helpers
- Resources and Tools
- Cigarette Cost Calculator
- Expert Voices Blogs on Tobacco and Smoking
- Latest News About Tobacco and Smoking
- QUIZ: Do You Need Help Quitting?
- Fight Back Against Tobacco
- Get the new Quit For Life Mobile app from Alere Wellbeing, available for iPhone and Android
Survey: Employees still under-informed on ACA, wellness
Originally posted November 8, 2013 by Tristan Lejeune on ebn.benefitnews.com
Only 15.1% of workers at large employers say they are “knowledgeable” or “very knowledgeable” about health care reform and the Affordable Care Act’s public exchanges, and nearly one in five can’t say for sure if their company has a wellness program or not, according a recent survey. The poll’s results, released this month, speak to a population that has confidence in the communication efforts of their benefits administrators, and that points out some serious shortfalls in that communication.
The survey, which spoke with 400 employees at companies with north of 2,000 each, found that only 29.5% could correctly identify times when they can make changes to their health plans, like open enrollment, according to the Jellyvison Labs. Jellyvision, which created ALEX, a virtual employee benefits counselor, says all but one of the employers involved in the survey offer health insurance, but employees still demonstrate large education gaps on their own benefits.
More than 90% of surveyed workers say it’s at least “somewhat important” to understand ACA and its implications, but less than a fifth actually consider themselves knowledgeable. The good news is employee confidence in their employers’ ability to communicate the necessary information is high: nearly 80% think their companies can properly bring them up to speed, and more than one in three rate their confidence levels on this point at eight or higher on a 10-point scale.
Some 77.6% of those polled agree that it is at least “somewhat important” for their organizations to offer a wellness program, but almost one-fifth don’t know with any certainty whether or not their company does so.
“One of the most important things we learned from this data,” says Josh Fosburg, vice president of business development for the Jellyvision Lab, “is employees aren’t getting everything they need to know about their employers’ wellness programs and other benefits. For instance, nearly half of employees in our survey think they have to pay something in order to take advantage of the wellness programming that will help them manage their weight, stay on top of their prescribed medications, or cease smoking. That’s bananas.”
Jellyvision says employers need to “up their communications game” in order to help employees take advantage of everything included in their benefits offerings.
Doctors urged to treat obesity like any other ailment; New guidelines say do whatever it takes to get the pounds off
Originally posted November 13, 2013 by Nanci Hellmich on www6.lexisnexis.com
There's no ideal diet that's right for everyone, but that shouldn't stop the nation's doctors from helping their heavy patients battle weight issues as aggressively as things like blood pressure, according to new obesity treatment guidelines released Tuesday.
The guidelines, from three leading health groups, say that doctors need to help obese patients figure out the best plan, whether it's a vegetarian diet, low-sodium plan, commercial weight-loss program or a low-carb diet.
Still, the most effective behavior-change weight-loss programs include two to three in-person meetings a month for at least six months, and most people should consume at least 500 fewer calories a day to lose weight, the recommendations say.
The guidelines are designed to help health care providers aggressively tackle the obesity epidemic. "The overall objective is quite a tall order: to get primary care practitioners to own weight management as they own hypertension management," says obesity researcher Donna Ryan, co-chairwoman of the committee writing these guidelines for the Obesity Society, American Heart Association and American College of Cardiology.
The recommendations are part of a set of heart disease prevention guidelines released Tuesday.
Nearly 155 million U.S. adults are overweight or obese, which is roughly 35 pounds over a healthy weight. Extra pounds put people at a higher risk of heart disease, stroke, many types of cancer, type 2 diabetes and a host of other health problems.
Health care providers should encourage obese and overweight patients who need to drop pounds for health reasons to lose at least 5% to 10% of their weight by following a moderately reduced-calorie diet suited to their food tastes and health status, while being physically active and learning behavioral strategies.
"The gold standard is an intervention delivered by trained interventionists (not just registered dietitians or doctors) for at least 14 sessions in the first six months and then continue therapy for a year," says Ryan, a professor emeritus at the Pennington Biomedical Research Center in Baton Rouge. If this kind of intensive therapy is not available, then other types of treatment, such as commercial weight-loss programs or telephone and Web-based programs, are good "second choices," she says.
Medicare began covering behavioral counseling for obese patients last year, and under the Affordable Care Act, most private insurance companies are expected to cover behavioral counseling and other obesity treatments by next year.
"There is no ideal diet for weight loss, and there is no superiority between the many diets we looked at," Ryan says. "We examined about 17 different weight-loss diets."
Pat O'Neil, director of the Weight Management Center at Medical University of South Carolina, says, "The diet you follow is the one that's going to work for you. That's good information for the public to have."
The report advises health care providers to calculate body mass index (a number that takes into account height and weight) at annual visits or more frequently, and use it to identify adults who may be at a higher risk of heart disease and stroke. Evidence shows that the greater the BMI, the higher the risk of coronary heart disease, stroke, type 2 diabetes and death from any cause, the report says. "BMI is a quick and easy first step," Ryan says.
The guidelines are being published simultaneously in Circulation, a journal of the American Heart Association; the Journal of the American College of Cardiology; and Obesity: Journal of the Obesity Society.
6 wellness tips for flu prevention
Originally posted on benefitnews.com
The flu costs businesses approximately $10.4 billion in direct costs for hospitalizations and out-patient visits for adults, according to the Centers for Disease Control and Prevention. In addition to encouraging workers to get immunized, employers can further minimize employee sick days and slow the spread of illness by communicating best practices in wellness and nutrition. Share these six preventive tips from Dr. Bruce Underwood, a certified nutrition and preventive care specialist with Healthy Futures, Inc., to keep workers and their families healthy this season.
No matter whether an individual decides to get immunized for influenza, primary prevention should be their priority for avoiding illness. Dr. Underwood explains that a good basis for our immune system is to get a good night’s sleep, generally between six to eight hours every night.
The surgeon general recommends all adults walk at least 10,000 steps or about 4 miles every day. If we over-exercise, then our immune system is weakened for a few days, explains Underwood. However, if we don't exercise at all our immune system is also weak.
As the following three slides prove, we need vitamins, minerals, amino acids, and fatty acids for our bodies to work well. Overall, Underwood recommends eating a wide variety of foods in amounts that allow you to maintain an ideal body weight.
One of the most important vitamins for immune health is vitamin C. The upper safe limit for Vitamin C is 2,000 mg for adults, according to the National Institute of Health. Underwood and other experts recommend 1,000 mg of the vitamin as a good daily dose. Dietary sources of the vitamin come mainly from fruits and vegetables, but can also be found in certain cuts of meat, especially liver. Studies have shown that our bodies expend Vitamin C to mitigate toxins such as cigarette smoke and pollution. The antioxidant has also helps relieve the physical and psychological effects of stress on people.
5. Zinc
The mineral Zinc is also necessary in stressful situations. By ingesting 10 to 40 milligrams of Zinc each day, individuals can also help build up their immune system. Underwood advises people to keep their daily dosage under 100 mg per day, however, as too much of the metal might cause fever, coughing, stomach pain, fatigue, and many other problems. Meats, seafood, dairy products, nuts, legumes, and whole grains offer relatively high levels of zinc.
U.S. Obesity Rate Climbing in 2013
Originally posted November 1, 2013 by Lindsey Sharpe on https://www.gallup.com
WASHINGTON, D.C. -- The adult obesity rate so far in 2013 is 27.2%, up from 26.2% in 2012, and is on pace to surpass all annual average obesity rates since Gallup-Healthways began tracking in 2008.
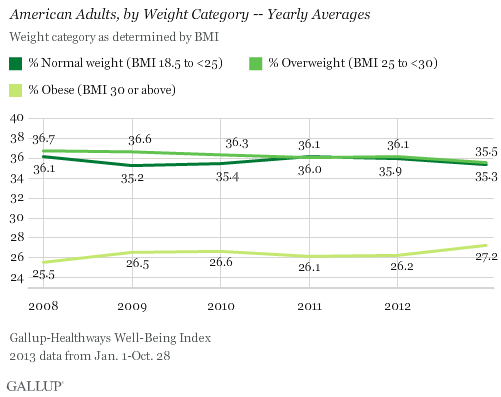
The one-percentage-point uptick in the obesity rate so far in 2013 is statistically significant and is the largest year-over-year increase since 2009. The higher rate thus far in 2013 reverses the lower levels recorded in 2011 and 2012, and is much higher than the 25.5% who were obese in 2008.
The increase in obesity rate is accompanied by a slight decline in the percentage of Americans classified as normal weight or as overweight but not obese. The percentage of normal weight adults fell to 35.3% from 35.9% in 2012, while the percentage of adults who are overweight declined to 35.5% from 36.1% in 2012. An additional 1.9% of Americans are classified as underweight in 2013 so far.
Since 2011, U.S. adults have been about as likely to be classified as overweight as normal weight. Prior to that, Americans were most commonly classified as overweight.
Gallup and Healthways began tracking Americans' weight in 2008. The 2013 data are based on more than 141,000 interviews conducted from Jan. 1 through Oct. 28 as part of the Gallup-Healthways Well-Being Index. Gallup uses respondents' self-reported height and weight to calculate body mass index (BMI) scores. Individual BMI values of 30 or above are classified as "obese," 25 to 29.9 are "overweight," 18.5 to 24.9 are "normal weight," and 18.4 or less are "underweight."
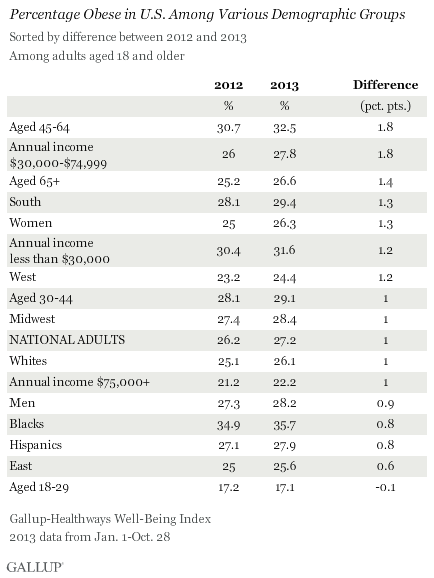
Obesity Rates Increase Across Almost All Demographic Groups
Obesity rates have increased at least slightly so far in 2013 across almost all major demographic and socioeconomic groups. One exception is 18- to 29-year-olds, among whom the percentage who are obese has remained stable. The largest upticks between 2012 and 2013 were among those aged 45 to 64 and those who earn between $30,000 and $74,999 annually. The obesity rate within both groups increased by 1.8 points, which exceeds the one-point increase in the national average.
At 35.7%, blacks continue to be the demographic group most likely to be obese, while those aged 18 to 29 and those who earn over $75,000 annually continue to be the least likely to be obese.
Bottom Line
The U.S. obesity rate thus far in 2013 is trending upward and will likely surpass all annual obesity levels since 2008, when Gallup and Healthways began tracking. It is unclear why the obesity rate is up this year, and the trend since 2008 shows a pattern of some fluctuation. This underscores the possibility that that the recent uptick is shorter-term, rather than a more permanent change. Still, if the current trend continues for the next several years, the implications for the health of Americans and the increased burden on the healthcare system could be significant.
Blacks, those who are middle-aged, and lower-income adults continue to be the groups with the highest obesity rates. The healthcare law could help reduce obesity among low-income Americans if the uninsuredsign up for coverage and take advantage of the free obesity screening and counseling that most insurance companies are required to provide under the law.
Employers can also take an active role to help lower obesity rates. Gallup has found that the annual cost for lost productivity due to workers being above normal weight or having a history of chronic conditions ranges from $160 million among agricultural workers to $24.2 billion among professionals. Thus, employers can cut healthcare costs by developing and implementing strategies to help workers maintain or reach a healthy weight.
Gallup has also found that employees who are engaged in their work eat healthier and exercise more. Therefore, employers who actively focus on improving engagement may see healthier and more productive workers, in addition to lower healthcare costs.
About the Gallup-Healthways Well-Being Index
The Gallup-Healthways Well-Being Index tracks well-being in the U.S. and provides best-in-class solutions for a healthier world. To learn more, please visit well-beingindex.com.
Results are based on telephone interviews conducted as part of the Gallup-Healthways Well-Being Index survey Jan. 1-Oct. 28, 2013, with a random sample of 141,935 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia.
For results based on the total sample of national adults, one can say with 95% confidence that the margin of sampling error is ±0.5 percentage points.
Interviews are conducted with respondents on landline telephones and cellular phones, with interviews conducted in Spanish for respondents who are primarily Spanish-speaking. Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by region. Landline and cellphone numbers are selected using random-digit-dial methods. Landline respondents are chosen at random within each household on the basis of which member had the most recent birthday.
Samples are weighted to correct for unequal selection probability, nonresponse, and double coverage of landline and cell users in the two sampling frames. They are also weighted to match the national demographics of gender, age, race, Hispanic ethnicity, education, region, population density, and phone status (cellphone only/landline only/both, and cellphone mostly). Demographic weighting targets are based on the March 2012 Current Population Survey figures for the aged 18 and older U.S. population. Phone status targets are based on the July-December 2011 National Health Interview Survey. Population density targets are based on the 2010 census. All reported margins of sampling error include the computed design effects for weighting.
In addition to sampling error, question wording and practical difficulties in conducting surveys can introduce error or bias into the findings of public opinion polls.
For more details on Gallup's polling methodology, visit www.gallup.com.
The Evil Presence that Lurks in the Workplace at Halloween
Originally posted by Denise Rand on https://hrdailyadvisor.blr.com
Halloween can be a very scary time of the year for HR pros! An evil presence is out to kill the efforts being put into company wellness programs—Halloween candy. Yes, it seems like Halloween becomes the end of year "kickoff party" for calorie-, sugar-, and fat-filled holiday celebrations in workplaces, sabotaging companies’ health efforts.
And besides candy, it’s a safe bet there will be plenty of orange-colored cakes, cupcakes, donuts, and even orange bagels within easy reach. However, there are some proactive steps the HR department can take to keep your employees from falling victim to a sugar rush and extra holiday pounds.
Health experts Dian Griesel, PhD, and Tom Griesel, authors of the book The TurboCharged Mind (January 2012, BSH), offer the following tips to avoid a crash:
- Make an office resolution to keep out of the office all the extra candy that the kids brought home or that didn’t go to the trick-or-treaters.
- Start the day by brewing a pot of pumpkin-flavored coffee or tea. This should help get coworkers in the spirit of things.
- Bring in a variety of fruit for morning break and colored veggies for enjoyment at lunch or afternoon break.
- Take a lunchtime walk to see the change of foliage and get some fresh autumn air.
- If your “office bakers” must produce Halloween treats, have them try making a gluten-free, low-, or sugar-free pumpkin pie. There are even many recipes for crust-less, no-shortening versions that make things even more healthful—and easy.
To incent or not to incent
Originally posted October 18, 2013 by Rhonda Willingham on lifehealthpro.com
There is a lot of confusion and more than a few questions about the use of incentives in benefits these days.
What do the Health Insurance Portability and Accountability Act’s (HIPAA) new wellness regulations mean? How can we incentivize employees, without risking noncompliance with new regulations?
Incentives are an especially big question mark for employers because so many want to find ways to motivate, encourage and lower the health care costs for the 5 percent to 10 percent of their employee population that is driving 80 percent or more of their costs.
Often these are employees who have chronic conditions such as diabetes or heart disease, or who may be obese – a condition now classified by the American Medical Association as a disease. Often these are also valuable tenured employees who have the skills, knowledge and expertise a company may need; helping them helps the company.
Here’s what you can tell your group health employer clients about the complex issues surrounding incentives today:
1. Offer a health risk assessment
One of the first steps toward getting employees to improve their health is the health risk assessment (HRA), which is the entry point for most wellness programs. Employers frequently offer financial incentives, premium discounts, or even PTO to get people to take the HRA.
Yes, HRAs have come into question of late in benefits circles – but, despite the current controversy, they remain a very smart tool for employers. They provide important information about the health status of employees and what programs (based on aggregate, not individual data) could provide the most value to the organization.
But . . . and here’s where a lot of employers have gotten into trouble . . . you must fully explain their value, including how they work. Include the steps that need to be taken to protect privacy and ensure employees know they can opt out – preferably without penalties - if wanted.
2. Understand what new regulations do and don’t say
What employers can and can’t do with incentives is governed in part by the Patient Protection and Affordable Care Act (PPACA) and HIPAA.
One of the many provisions of PPACA is that it allows employers to link greater financial incentives to the achievement of predetermined health targets, such as smoking cessation or healthy weight. HIPAA also governs what group health plans can do with benefit programs.
Most importantly, HIPAA prohibits employers from charging different premiums based on health status. People can’t be penalized just because someone is overweight or has diabetes or heart disease.
HIPAA’s new wellness regulations, introduced in June of this year, state that:
…a group health plan…may not require any individual (as a condition of enrollment or continued enrollment under the plan) to pay a premium or contribution which is greater than [that] for a similarly situated individual enrolled in the plan on the basis of any health status related factor…
The other major component for HIPAA is guidance on the dollar amount allowed for incentives.
Health plans and insurers will be able to offer higher financial rewards to participants achieving healthy behaviors such as quitting smoking or reducing cholesterol. Specifically, as of Jan. 1, up to 30 percent of the total cost of health plan coverage (employer and employee cost of coverage with no cap) may be tied to an incentive. Tobacco cessation and usage reduction programs allow rewards to be increased to 50 percent. Now, in reality very few employers will go up to that 30 percent, but it is an option.
The real trick to compliance with HIPAA’s wellness regulations is that wellness programs will have to ensure they do not discriminate against people based on health factors. For example, if an employee is extremely obese and unable to participate in a walking program that provides financial incentives, there must be an alternative program for that employee.
3. Determine if you will use a carrot or stick
Employers have developed a range of approaches to incentives over the past few years. Most incentives today are based either on participation, outcomes or progress. Participation-based programs are simple.
You participate, sign a sheet that you came to the stop-smoking class or joined a gym, and you qualify for the incentive. Outcome-based programs usually include financial incentives.
Employers have learned over time that money is a great motivator for participation in either the HRA or a wellness program. The threshold for motivating employees seems to be right around $300 to $500 annually.
The key characteristic of an outcome incentive is that the employee doesn’t get that incentive unless he or she achieves a pre-determined goal or health standard, such as quitting tobacco use, losing 10 percent of body weight within six months, or bringing cholesterol levels within normal limits, etc.
Progress-based incentives are viewed as a “kinder, gentler” approach. They reward employees based on incremental, individually-attainable goals rather than a singular goal for all. In other words, you may need to lose 50 pounds, but the employer says, “We know losing even five pounds helps you and helps us, so you will still get the incentive.” (Studies show even small reductions in risk lower health care costs.)
Here again is where the incentive question gets tough and complicated. A Towers Watson 2012 survey reports that 62 percent of employers plan on switching from incentives for participation – which employees like – to incentives for improvements – which employers like – because it holds employees more accountable and the thought/hope is it will produce more tangible and measurable outcomes.
So what’s an employer to do when it comes to incentives? As we are learning from recent high profile news stories, employees will push back hard if they don’t support a wellness program and its goals (which typically happens if there is poor communication), or if they think non-participation penalties are too punitive. We all understand the need for accountability, but if that comes at the price of an unhappy employee population, what have you really won?
Every organization is different; I think it’s difficult to mandate you must do X, Y or Z. As part of my job with a leading health and wellness company and as a member of a number of key organizations evaluating worksite wellness programs and incentives, my recommendation is to consider a developing and evolving plan with incentives that engage, motivate and encourage all employees.
Start with simply incentivizing participation. Then as the program becomes better accepted with employees experiencing success – and as you do more education and communication – you can always migrate to the incorporation of a program that incentivizes progress.
Again, there is no one-size fits all, but we do know that what truly motivates people are programs that build intrinsic motivation. Program designs with the best chance of fostering such intrinsic motivation are those that use extrinsic tools (e.g., a weight loss program for employees) in a way that doesn’t make employees feel pressured but creates a supportive and empowering environment that promotes individual choice.
The last word on incentives is that the ultimate goal is not to get people to engage in behaviors for a short period of time just to get dollars. The objective is for employees to internalize the goal and learn how to make and sustain better lifestyle choices themselves.
