Collaborative Innovation Is Necessary To Advance In Health Care

Shutterstock
As health needs grow, it is imperative that innovation is at the frontier of change, to keep the health needs and requirements of the 21st century scalable. For innovation in health care to be sustained at an economically and fiscally responsible pace, it has to be a collaborative effort, requiring input from diverse stakeholders and key players in the industry. A collaborative health care system that includes information sharing, cross-industry cooperation and open innovation can lead to beneficial industry practices like cost reduction and time efficiency. Together, these practices set a precedent for growth and development at a more rapid pace.
An Efficient Method Of Doing Things
Toeing the line of technology advancements, innovation within the health care system has pioneered the development of cost-efficient, highly-optimized pragmatic solutions to many industry and individual health challenges. Artificial retinas, robotic nurses and gene therapy are just a few examples of plentiful recent innovations. These innovative technologies pose solutions to medical feats that, in the past, have overwhelmed medical practitioners, and thereby are expected to permit better health care delivery to patients and the global population. However, for these new advancements to be successfully implemented and established within the health care system, they must be met with collaboration and cooperation.
Creating A Synergistic Environment
Open, collective innovation like Project Data Sphere, designed to collate big data and bridge the distant segments of the health care industry, markup the necessity of innovation in the sector. In the case of Project Data Sphere, the goal is to facilitate the creation of a connected health care network bereft of the many loopholes characteristic of the system. Interoperability between key segments of the industry has always been a rate limiting factor. A unified platform capable of linking these segments together can have a significant impact on the sector.
Multiple companies are undertaking projects to build "cloud-based, big data platform" solutions that manage data to give the health industry the necessary edge it needs to manage itself. This ranges from cloud-based platforms powered by libraries of clinical, social and behavioral analytics utilized for sharing information across multiple hospitals, to using big data and advanced analytics for clinical improvements, financial analysis and fraud and waste monitoring.
Collaborating To Go Digital
Concurrent with the world’s continued adoption of digital technologies is the rapid expansion of the digital health care market — an expansion fostered by collaboration among global leaders of digital innovation in the health care industry. The partnership between major players in both the private and public sectors has engineered a growing list of innovative digital health care solutions.
Just last year an Israeli-based pharmaceutical company joined forces with Santa Clara, California-based Intel to develop wearables that routinely record and analyze symptoms of Huntington’s disease. The data collected is processed to help grade motor symptom severity associated with the disease.
Most times, singular organizations lack the human and financial resources to orchestrate grand schemes of innovation alone — but collaboration presents a practical route to overcoming the limitations that hinder novelty, leading to quicker turnarounds and advancements.
Scaling The Barriers To Innovation
If the push for innovation in the health care system is to thrive, then the complexities and obstacles that have continually stifled progress must be confronted. Aside from collaboration, other notable barriers to innovation include:
• The immediate return mentality: By default, most leaders show a preference for innovative solutions that offer immediate financial rewards. Innovative solutions with brighter prospects but long term financial incentives are in most instances placed on a back burner.
• Bureaucracy in the distributive network:Innovators have to wade through multiple third parties if they are to stand any chance of getting their products to the end user, a process that is not only daunting but financially implicative.
• Stringent regulatory practices: In addition to scaling through the bureaucracy, innovative solutions looking to make a market appearance have to pass several screenings, some of which have been tagged redundant by experts.
Innovation is a necessary tool in the health care sector that gives an essential boost to scale insurmountable obstacles and limitations. For health care to evolve into a more sophisticated and efficient system, cross-industry collaboration and inter-professional cooperation must become the norm.
You can read the original article here.
Source:
Pando A. (19 September 2017). "Collaborative Innovation Is Necessary To Advance In Health Care" [Web blog post]. Retrieved from address https://www.forbes.com/sites/forbestechcouncil/2017/09/19/collaborative-innovation-is-necessary-to-advance-in-health-care/2/#6743d07669c9
CenterStage...Open Season for Open Enrollment
In this month’s CenterStage, we interviewed Rich Arnold for some in-depth information on Medicare plans and health coverage. Read the full article below.

Open Season for Open Enrollment: What does it mean for you?
There are 10,000 people turning 65 every single day. Medicare has a lot of options, causing the process to be extremely confusing. Rich – a Senior Solutions Advisor – works hard to provide you with the various options available to seniors in Ohio, Kentucky and Indiana and reduce them to an ideal, simple, and easy-to-follow plan.

“For me, this is all about helping people.”
– Rich Arnold, Senior Solutions Advisor
What does this call for?
To provide clients with top-notch Medicare guidance, Rich must analyze their current doctors and drugs for the best plan option and properly educate them to choose the best program for their situation and health. It’s a simple, free process of evaluation, education, and enrollment.
For this month’s CenterStage article, we asked Rich to break down Medicare for the senior population who are in desperate need of a break from the confusion.
Medicare Break Down
Part A. Hospitalization, Skilled Nursing, etc.
If you’ve worked for 40 quarters, you automatically obtain Part A coverage.
Part B. Medical Services: Doctors, Surgeries, Outpatient visits, etc.…
You must enroll and pay a monthly premium.
Part C. Medicare Advantage Plans:
Provides most of your hospital and medical expenses.
Part D.
Prescription drug plans available with Medicare.
Under Parts A & B there are two types of plans…
Supplement Plan or Medigap Plan
A Medicare Supplement Insurance (Medigap) policy can help pay some of the health care costs that Original Medicare doesn’t cover, like copayments, coinsurance, and deductibles, coverage anywhere in the US as well as travel outside of the country, pay a monthly amount, and usually coupled with a prescription drug plan.
Advantage Plan
A type of Medicare health plan that contracts with Medicare to provide you with all your Part A and Part B benefits generally through a HMO or PPO, pay a monthly amount from $0 and up, covers emergency services, and offers prescription drug plans.
How does this effect you?
Medicare starts at 65 years of age, but Rich advises anyone turning 63 or 64 years of age to reach out to an advisor, such as himself, for zero cost, to be put onto their calendar to follow up at the proper time to investigate the Medicare options. Some confusion exists about Medicare and Social Security which are separate entities. Social Security does not pay for the Supplement or Advantage plans.
Medicare Open Enrollment: Open Enrollment occurs between October 15th and December 7 – yes, right around the corner! However, don’t panic, Rich and his services can help you if you are turning 65 or if you haven’t reviewed your current plan in over a year – you should seek his guidance.
Your plan needs to be reviewed every year to best fit your needs. If you’re on the verge of 65, turning 65 in the next few months, or over 65, you should consult your Medicare advisor as soon as possible. For a no cost analysis of your needs contact Rich, Saxon Senior Solutions Advisor, rarnold@gosaxon.com, 513-808-4879.
Health Care Sector Earnings: Major Companies Open The Books On Q3 Results In Weeks Ahead

Photo Credit: Shutterstock
The health care sector has been one of the better-performing sectors in 2017, bouncing back after being the only sector in the S&P 500 to finish last year in the red. So far this year, the S&P Health Care Select Sector Index is outperforming the S&P 500 by 5.75% as of October 6.
The sector got a bump recently when Republicans’ released an initial framework for tax reform, with CNBC pointing out that some of the largest companies in the health care sector could be primary beneficiaries of the proposed repatriation tax break. For the sector’s upcoming earnings, analyst estimates are calling for low to mid-single-digit growth for both earnings and revenue.
Within the S&P 500, the health care sector is expected to report year-over-year revenue growth of 4.8% and earnings growth of 2.5%, according to FactSet, with profit margins estimated to decline from 10.3% to 10.1% across the sector. Those estimates are slightly below the sector’s estimated revenue and earnings growth rates expected for the full year.
Beyond the proposed tax reform, below we’ll take a look at what’s been happening in the sector as companies prepare to report earnings in the upcoming weeks.
 thinkorswim
thinkorswimAfter underperforming by a large margin in 2016, the health care sector has been recovering in 2017. The S&P Health Care Select Sector Index, charted above, is up 18.49% year-to-date, compared to a 12.74% increase in the S&P 500, the teal line. The Nasdaq Biotechnology Index, the purple line, has outperformed both and climbed 25.6% year-to-date. Chart source: thinkorswim® by TD Ameritrade. Data source: Standard & Poor’s. Not a recommendation. For illustrative purposes only. Past performance does not guarantee future results.
Biotech Industry Outperforming
So far this year, the biotechnology industry has outpaced the broader health care sector, with the Nasdaq Biotechnology Index up 25.6% versus a 18.49% increase in the S&P Health Care Select Sector Index. However, looking at 2016, the Nasdaq Biotechnology Index fared far worse than the S&P Health Care Select Sector Index, declining 22.01% when the latter only declined 4.37%.
Stocks in the biotech industry are notoriously volatile and it can take many years, even decades, for a company to undergo research and development, and the clinical trial process. A 2014 study by Tufts University’s Center for the Study of Drug Development found that only 11.8% of drugs that enter clinical trials end up being approved by the FDA.
Washington on Health Care
Drug pricing scrutiny has been an ongoing focus in Congress, but there’s yet to be concrete legislation pushed forward to address the issue. Dr. Scott Gottlieb, the head of the Food and Drug Administration (FDA), recently said high drug prices are a “public health concern” and in a post on the FDA’s official blog, outlined several steps the agency is taking to make the generic approval process for complex drugs easier.
On October 17, the Senate Health Committee is scheduled to hold a second hearing as part of its investigation into high drug prices. Representatives from drug company and pharmacy benefit managers—essentially middle men between pharmacies and drug companies—have been invited to speak before the panel. Depending on how that hearing goes, there could be heightened volatility in healthcare stocks.
Due to the costly process of developing drugs, companies often go to great lengths to protect patents. Those practices have also started to come into scrutiny in Congress as well. Allergan announced last month it had transferred the patent rights for its drug Restasis to the St. Regis Mohawk Indian Nation, which would license them back to Allergan in exchange for ongoing payments to the tribe.
The tribe’s sovereign immunity would potentially shield the drug from certain patent reviews. “Allergan has argued that the legal maneuver is aimed at removing administrative patent challenges through inter partes review by the U.S. Patent Trial and Appeal Board, and not challenges in federal court”, according to Reuters.Shortly after Allergan transferred the patent rights, U.S. Senator Claire McCaskill quickly announced she had drafted a bill to prevent tribal sovereign immunity from being used to block U.S. Patent and Trademark Office review of a patent in response to the move.
Aging Demographics and More Disease as Population Grows
There are some trends that analysts anticipate to be tailwinds for the sector for years to come. One of them is aging demographics and the other is growth of certain diseases. Approximately 10,000 baby boomers turn 65 every day, according to Pew Research, and that trend is expected to continue until 2030, when the last of the boomers reach retirement age and roughly 18% of the U.S. population is projected to be 65 and older.
As world populations grow and age, certain diseases are expected to have a greater prevalence than others and a large portion of health care spending is likely to go towards them. By 2020, Deloitte projects that 50% of global health care expenditures, about $4 trillion, will be spent on cardiovascular diseases, cancer and respiratory diseases.
These trends could be a tailwind for healthcare companies, but at the same time a lot could change in the regulatory environment as well as with the treatments available in the years ahead.
Looking Ahead to Earnings
The first major company in the sector to report earnings is Johnson & Johnson, which will release results before market open on Tuesday, October 17. The following companies report later in the month: Eli Lilly & Co. before market open on Tuesday, October 24, Gilead Sciences after market close on Thursday, October 26, Merck before market open on Friday, October 27 and Pfizer before market open on Tuesday, October 31.
You can read the original article here.
Source:
Kinahan J. (10 October 2017). "Health Care Sector Earnings: Major Companies Open The Books On Q3 Results In Weeks Ahead" [Web Blog Post]. Retrieved from address https://www.forbes.com/sites/jjkinahan/2017/10/10/health-care-sector-earnings-major-companies-open-the-books-on-q3-results-in-weeks-ahead/#417bef6a44bb
Self funded health care – a big business advantage
Check out this article from Business Insurance by one of their staff writers. In this article, Business Insurance dives into the awesome advantages of self-funding for big businesses.
You can read the original article here.
Health insurance benefits are expensive. The rising costs of health care has driven up insurance premiums to levels where many businesses have been forced to reduce these benefits or drop them altogether. There is, however another option that is less regulated, taxed less and typically results in cost savings: self funded health insurance. The problem is, it's not always the best option for all employers, particularly the smaller ones. And there's a number of reasons for this:
What is self funded health care a.k.a. self-insurance?
Self-insurance is a method of providing health care to employees by taking on the financial liabilities of the care instead of paying premiums to an insurance agency to do the same. In other words: when a person covered under a self-funded plan needs medical care, the company is financially responsible for paying the medical bill (minus deductibles). It's an alternative risk transfer strategy that assumes the risk and liability of medical bills for those covered instead of outsourcing it to a third party. It's a surprisingly common practice:
In 2008, 55% of workers with health benefits were covered by a self-insured plan….and 89% of workers in firms of 5,000 or more employees.
Most (but not all) self-insurance plans are administered by a third party, usually a health insurance company, in order to process claims. The bills are simply paid for by the employer. Health insurance companies act as a third party administrators in what are called ASO contracts (Administrative Services Only)
Another common component of self insurance plans is stop-loss insurance. This is a separate insurance plan that the employer can purchase to reduce the overall liability of claims. With this type of insurance, if claims exceed a certain dollar amount, stop-loss kicks in paying the rest. There are two kinds of stop-loss insurance:
Specific – covers the excess costs from larger claims made by individuals in the group
Aggregate – kicks in when total claims by the group exceed a set amount
For example, a company who self-insures their $1000 employees projects $100,000 in medical care claims for the year. If they purchase aggregate stop-loss insurance for claims that exceed 120% of the expected amount or $120,000, the insurance will pick up the bill for the remaining claims. If the company purchases specific stop-loss insurance at 200%, if any single claim exceeds $2,000, the stop-loss pays the remainder.
Typically, self-funded insurance providers will purchase both specific and aggregate stop-loss insurance unless the conditions are such that specific stop-loss provides enough financial protection.
Benefits of self-insurance
There are a number of financial and administrative advantages to using self-funded health insurance plans for employers. According to the Self-Insurance Institute of America (SIIA) these include:
- The employer can customize the plan to meet the specific health care needs of its workforce, as opposed to purchasing a 'one-size-fits-all' insurance policy.
- The employer maintains control over the health plan reserves, enabling maximization of interest income – income that would be otherwise generated by an insurance carrier through the investment of premium dollars.
- The employer does not have to pre-pay for coverage, thereby providing for improved cash flow.
- The employer is not subject to conflicting state health insurance regulations/benefit mandates, as self-insured health plans are regulated under federal law (ERISA).
- The employer is not subject to state health insurance premium taxes, which are generally 2-3 percent of the premium's dollar value.
- The employer is free to contract with the providers or provider network best suited to meet the health care needs of its employees.
There are, however, some drawbacks to self-insurance policies:
Health care can be costly, so heavy claims years can be extremely expensive
Self insurance isn't tax deductible the same way the costs of providing health insurance is.
Financial benefits are long-term, particularly with an investment component.
Small businesses at a disadvantage
Self insurance is much more prevalent for larger companies mostly because it is easier to predict health care costs from a larger group. The more people in the group, the less potentially damaging a single expensive claim will be to the plan overall. That's why less than 10% of companies with less than 50 employees use self-insurance.
Because risk is more difficult to predict with smaller groups, stop-loss insurance is also more expensive for smaller businesses. The practice of “lasering”, or increasing deductibles for specific higher risk employees can also be much tougher on small firms. As a result, self-insurance tends to be a less cost effective option than it is for larger companies.
Another roadblock for small businesses is a lack of cash-flow that is necessary to finance self-insurance. This doesn't mean, however, that small businesses can't benefit from a self-insurance plan. In fact, an increasing number of small businesses still are. But fully understanding the risks and rewards for doing so can sometimes be difficult.
Regulations
Because the only 3rd party administration of insurance (stop-loss) is between the employer and the insurance company directly, it is not subject to state level regulation the way traditional insurance policies are. Instead, they're regulated by the department of labor under the Employee Retirement Income Security Act – ERISA. Benefit administrators must still comply with federal standards despite the lack of state regulation.
California SB 1431
California is considering a proposed legislation to regulate the sale of stop-loss policies to smaller businesses. On the surface, the regulation looks as though it is an attempt to prevent small businesses from taking on too much risk. But the true intentions of the legislation may be to prevent cherry-picking of generally healthier small businesses (effectively removing them from the health insurance pool). This cherry-picking would theoretically cause traditional insurance premiums to become more expensive.
According to the SIIA, SB 1431 would prohibit the sale of stop-loss policies to employers with fewer than 50 employees that does any of the following:
- Contains a specific attachment point that is lower than $95,000;
- Contains an aggregate attachment point that is lower than the greater of one of the following:
- $19,000 times the total number of covered employees and dependents;
- 120% of expected claims;
- $95,000
This legislation would effectively limit the options of small businesses as it would force them to purchase a more expensive low deductible stop-loss policies. And according to the SIIA, with this legislation, almost no small business under 50 employees would (nor should they) consider self-insurance as an option.
If the legislation is passed in California, it has been suggested that it is only time before other states follow suit and/or enact even stricter regulations on small businesses. The SIIA even has a facebook page dedicated to defeating the bill they say is:
“…unnecessary and will only exasperate the problem that small employers in California face in being able to afford the rising cost of providing quality health benefits to their employees.”
So while self insurance can be a relatively risky option for small businesses, with legislation like this, it could no longer be a realistic option at all… And, in effect: another competitive advantage big businesses will have over their smaller counterparts.
You can read the original article here.
Source:
Staff Writer. (Date Unlisted). "Self funded health care – a big business advantage" [Web Blog Post]. Retrieved from address https://www.businessinsurance.org/self-funded-health-care-a-big-business-advantage/
The Medicare Part D Prescription Drug Benefit
Below we have an article from the Kaiser Family Foundation providing detailed information and graphics on the benefit of the Medicare Prescription Drug Plan.
You can read the original article here.
Medicare Part D is a voluntary outpatient prescription drug benefit for people on Medicare that went into effect in 2006. All 59 million people on Medicare, including those ages 65 and older and those under age 65 with permanent disabilities, have access to the Part D drug benefit through private plans approved by the federal government; in 2017, more than 42 million Medicare beneficiaries are enrolled in Medicare Part D plans. During the Medicare Part D open enrollment period, which runs from October 15 to December 7 each year, beneficiaries can choose to enroll in either stand-alone prescription drug plans (PDPs) to supplement traditional Medicare or Medicare Advantage prescription drug (MA-PD) plans (mainly HMOs and PPOs) that cover all Medicare benefits including drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing. This fact sheet provides an overview of the Medicare Part D program and information about 2018 plan offerings, based on data from the Centers for Medicare & Medicaid Services (CMS) and other sources.
Medicare Prescription Drug Plan Availability in 2018
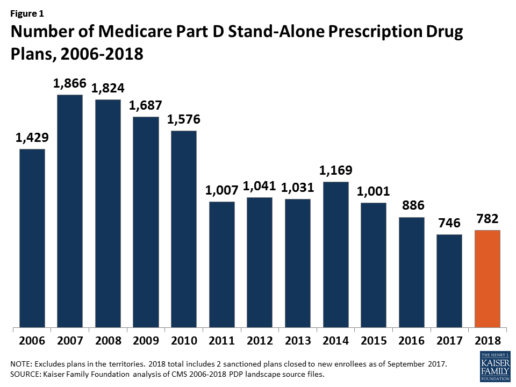
In 2018, 782 PDPs will be offered across the 34 PDP regions nationwide (excluding the territories). This represents an increase of 36 PDPs, or 5%, since 2017, but a reduction of 104 plans, or 12%, since 2016 (Figure 1).
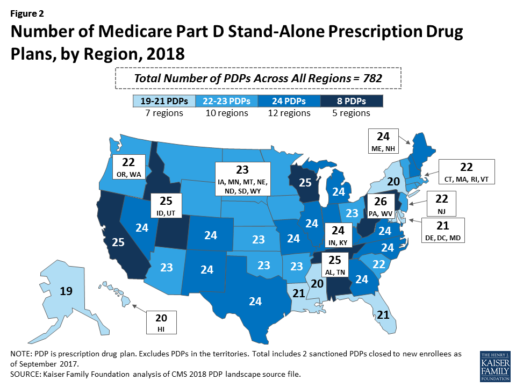
Beneficiaries in each state will continue to have a choice of multiple stand-alone PDPs in 2018, ranging from 19 PDPs in Alaska to 26 PDPs in Pennsylvania/West Virginia (in addition to multiple MA-PD plans offered at the local level) (Figure 2).
Low-Income Subsidy Plan Availability in 2018
Through the Part D Low-Income Subsidy (LIS) program, additional premium and cost-sharing assistance is available for Part D enrollees with low incomes (less than 150% of poverty, or $18,090 for individuals/$24,360 for married couples in 2017) and modest assets (less than $13,820 for individuals/$27,600 for couples in 2017).1
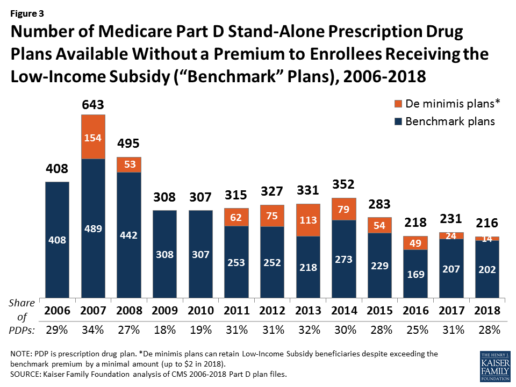
In 2018, 216 plans will be available for enrollment of LIS beneficiaries for no premium, a 6% decrease in premium-free (“benchmark”) plans from 2017 and the lowest number of benchmark plans available since the start of the Part D program in 2006. Roughly 3 in 10 PDPs in 2018 (28%) are benchmark plans (Figure 3).
Low-Income Subsidy Plan Availability in 2018
Through the Part D Low-Income Subsidy (LIS) program, additional premium and cost-sharing assistance is available for Part D enrollees with low incomes (less than 150% of poverty, or $18,090 for individuals/$24,360 for married couples in 2017) and modest assets (less than $13,820 for individuals/$27,600 for couples in 2017).1
In 2018, 216 plans will be available for enrollment of LIS beneficiaries for no premium, a 6% decrease in premium-free (“benchmark”) plans from 2017 and the lowest number of benchmark plans available since the start of the Part D program in 2006. Roughly 3 in 10 PDPs in 2018 (28%) are benchmark plans (Figure 3).
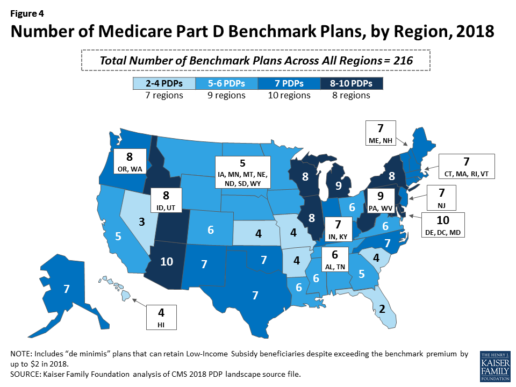
Benchmark plan availability varies at the Part D region level, with most regions seeing a reduction of 1 benchmark plan for 2018 (Figure 4). The number of premium-free plans in 2018 ranges from a low of 2 plans in Florida to 10 plans in Arizona and Delaware/Maryland/Washington D.C.
Part D Plan Premiums and Benefits in 2018
Premiums. According to CMS, the 2018 Part D base beneficiary premium is $35.02, a modest decline of 2% from 2017.2 Actual (unweighted) PDP monthly premiums for 2018 vary across plans and regions, ranging from a low of $12.60 for a PDP available in 12 out of 34 regions to a high of $197 for a PDP in Texas.
Part D enrollees with higher incomes ($85,000/individual; $170,000/couple) pay an income-related monthly premium surcharge, ranging from $13.00 to $74.80 in 2018 (depending on their income level), in addition to the monthly premium for their specific plan.3 According to CMS projections, an estimated 3.3 million Part D enrollees (7%) will pay income-related Part D premiums in 2018.
Benefits. In 2018, the Part D standard benefit has a $405 deductible and 25% coinsurance up to an initial coverage limit of $3,750 in total drug costs, followed by a coverage gap. During the gap, enrollees are responsible for a larger share of their total drug costs than in the initial coverage period, until their total out-of-pocket spending in 2018 reaches $5,000 (Figure 5).
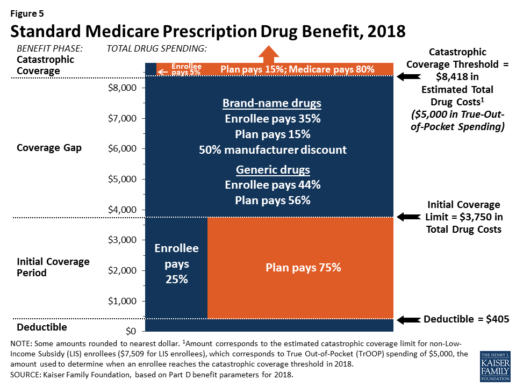
After enrollees reach the catastrophic coverage threshold, Medicare pays for most (80%) of their drug costs, plans pay 15%, and enrollees pay either 5% of total drug costs or $3.35/$8.35 for each generic and brand-name drug, respectively.
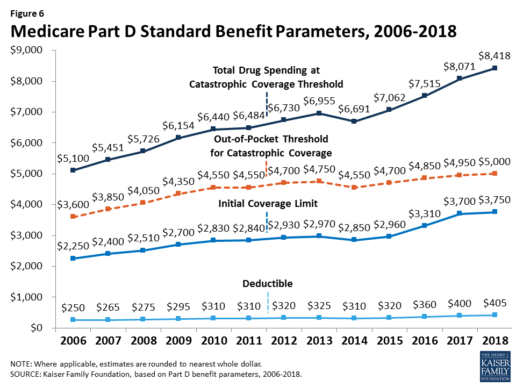
The standard benefit amounts are indexed to change annually by rate of Part D per capita spending growth, and, with the exception of 2014, have increased each year since 2006 (Figure 6).
Part D plans must offer either the defined standard benefit or an alternative equal in value (“actuarially equivalent”), and can also provide enhanced benefits. But plans can (and do) vary in terms of their specific benefit design, cost-sharing amounts, utilization management tools (i.e., prior authorization, quantity limits, and step therapy), and formularies (i.e., covered drugs). Plan formularies must include drug classes covering all disease states, and a minimum of two chemically distinct drugs in each class. Part D plans are required to cover all drugs in six so-called “protected” classes: immunosuppressants, antidepressants, antipsychotics, anticonvulsants, antiretrovirals, and antineoplastics.
In 2018, almost half (46%) of plans will offer basic Part D benefits (although no plans will offer the defined standard benefit), while 54% will offer enhanced benefits, similar to 2017. Most PDPs (63%) will charge a deductible, with 52% of all PDPs charging the full amount ($405). Most plans have shifted to charging tiered copayments or varying coinsurance amounts for covered drugs rather than a uniform 25% coinsurance rate, and a substantial majority of PDPs use specialty tiers for high-cost medications. Two-thirds of PDPs (65%) will not offer additional gap coverage in 2018 beyond what is required under the standard benefit. Additional gap coverage, when offered, has been typically limited to generic drugs only (not brands).
The 2010 Affordable Care Act gradually lowers out-of-pocket costs in the coverage gap by providing enrollees with a 50% manufacturer discount on the total cost of their brand-name drugs filled in the gap and additional plan payments for brands and generics. In 2018, Part D enrollees in plans with no additional gap coverage will pay 35% of the total cost of brands and 44% of the total cost of generics in the gap until they reach the catastrophic coverage threshold. Medicare will phase in additional subsidies for brands and generic drugs, ultimately reducing the beneficiary coinsurance rate in the gap to 25% by 2020.
Part D and Low-Income Subsidy Enrollment
Enrollment in Medicare drug plans is voluntary, with the exception of beneficiaries who are dually eligible for both Medicare and Medicaid and certain other low-income beneficiaries who are automatically enrolled in a PDP if they do not choose a plan on their own. Unless beneficiaries have drug coverage from another source that is at least as good as standard Part D coverage (“creditable coverage”), they face a penalty equal to 1% of the national average premium for each month they delay enrollment.
In 2017, more than 42 million Medicare beneficiaries are enrolled in Medicare Part D plans, including employer-only group plans.4 Of this total, 6 in 10 (60%) are enrolled in stand-alone PDPs and 4 in 10 (40%) are enrolled in Medicare Advantage drug plans. Medicare’s actuaries estimate that around 2 million other beneficiaries in 2017 have drug coverage through employer-sponsored retiree plans where the employer receives subsidies equal to 28% of drug expenses between $405 and $8,350 per retiree in 2018 (up from $400 and $8,250 in 2017).5 Several million beneficiaries are estimated to have other sources of drug coverage, including employer plans for active workers, FEHBP, TRICARE, and Veterans Affairs (VA). Yet an estimated 12% of Medicare beneficiaries lack creditable drug coverage.
Twelve million Part D enrollees are currently receiving the Low-Income Subsidy. Beneficiaries who are dually eligible, QMBs, SLMBs, QIs, and SSI-onlys automatically qualify for the additional assistance, and Medicare automatically enrolls them into PDPs with premiums at or below the regional average (the Low-Income Subsidy benchmark) if they do not choose a plan on their own. Other beneficiaries are subject to both an income and asset test and need to apply for the Low-Income Subsidy through either the Social Security Administration or Medicaid.
Part D Spending and Financing in 2018
The Congressional Budget Office (CBO) estimates that spending on Part D benefits will total $92 billion in 2018, representing 15.5% of net Medicare outlays in 2018 (net of offsetting receipts from premiums and state transfers). Part D spending depends on several factors, including the number of Part D enrollees, their health status and drug use, the number of enrollees receiving the Low-Income Subsidy, and plans’ ability to negotiate discounts (rebates) with drug companies and preferred pricing arrangements with pharmacies, and manage use (e.g., promoting use of generic drugs, prior authorization, step therapy, quantity limits, and mail order). Federal law prohibits the Secretary of Health and Human Services from interfering in drug price negotiations between Part D plan sponsors and drug manufacturers.6
Financing for Part D comes from general revenues (78%), beneficiary premiums (13%), and state contributions (9%). The monthly premium paid by enrollees is set to cover 25.5% of the cost of standard drug coverage. Medicare subsidizes the remaining 74.5%, based on bids submitted by plans for their expected benefit payments. Part D enrollees with higher incomes ($85,000/individual; $170,000/couple) pay a greater share of standard Part D costs, ranging from 35% to 80%, depending on income.
According to Medicare’s actuaries, in 2018, Part D plans are projected to receive average annual direct subsidy payments of $353 per enrollee overall and $2,353 for enrollees receiving the LIS; employers are expected to receive, on average, $623 for retirees in employer-subsidy plans.7 Part D plans’ potential total losses or gains are limited by risk-sharing arrangements with the federal government (“risk corridors”). Plans also receive additional risk-adjusted payments based on the health status of their enrollees and reinsurance payments for very high-cost enrollees.
Under reinsurance, Medicare subsidizes 80% of drug spending incurred by Part D enrollees above the catastrophic coverage threshold. In 2018, average reinsurance payments per enrollee are estimated to be $941; this represents a 7% increase from 2017. Medicare’s reinsurance payments to plans have represented a growing share of total Part D spending, increasing from 16% in 2007 to an estimated 41% in 2018.8 This is due in part to a growing number of Part D enrollees with spending above the catastrophic threshold, resulting from several factors, including the introduction of high-cost specialty drugs, increases in the cost of prescriptions, and a change made by the ACA to count the 50% manufacturer discount in enrollees’ out-of-pocket spending that qualifies them for catastrophic coverage. Analysis from MedPAC also suggests that in recent years, plans have underestimated their enrollees’ expected costs above the catastrophic coverage threshold, resulting in higher reinsurance payments from Medicare to plans over time.
Issues for the Future
After several years of relatively low growth in prescription drug spending, spending has risen more steeply since 2013. The average annual rate of growth in Part D costs per beneficiary was 2.4% between 2007 and 2013, but it increased to 4.4% between 2013 and 2016, and is projected to increase by 4.7% between 2016 and 2026
(Figure 7).9
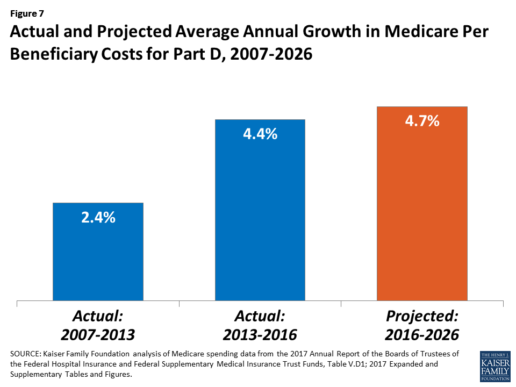
Medicare’s actuaries have projected that the Part D per capita growth rate will be comparatively higher in the coming years than in the program’s initial years due to higher costs associated with expensive specialty drugs, which is expected to be reflected in higher reinsurance payments to plans. Between 2017 and 2027, spending on Part D benefits is projected to increase from 15.9% to 17.5% of total Medicare spending (net of offsetting receipts).10 Understanding whether and to what extent private plans are able to negotiate price discounts and rebates will be an important part of ongoing efforts to assess how well plans are able to contain rising drug costs. However, drug-specific rebate information is not disclosed by CMS.
The Medicare drug benefit helps to reduce out-of-pocket drug spending for enrollees, which is especially important to those with modest incomes or very high drug costs. Closing the coverage gap by 2020 will bring additional relief to millions of enrollees with high costs. But with drug spending on the rise and more plans charging coinsurance rather than flat copayments for covered brand-name drugs, enrollees could face higher out-of-pocket costs for their Part D coverage. These trends highlight the importance of comparing plans during the annual enrollment period. Research shows, however, that relatively few people on Medicare have used the annual opportunity to switch Part D plans voluntarily—even though those who do switch often lower their out-of-pocket costs as a result of changing plans.
Understanding how well Part D is working and how well it is meeting the needs of people on Medicare will be informed by ongoing monitoring of the Part D plan marketplace and plan enrollment; assessing coverage and costs for high-cost biologics and other specialty drugs; exploring the relationship between Part D spending and spending on other Medicare-covered services; and evaluating the impact of the drug benefit on Medicare beneficiaries’ out-of-pocket spending and health outcomes.
Endnotes
- Poverty and resource levels for 2018 are not yet available (as of September 2017).
- The base beneficiary premium is equal to the product of the beneficiary premium percentage and the national average monthly bid amount (which is an enrollment-weighted average of bids submitted by both PDPs and MA-PD plans). Centers for Medicare & Medicaid Services, “Annual Release of Part D National Average Bid Amount and Other Part C & D Bid Information,” July 31, 2017, available at https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/PartDandMABenchmarks2018.pdf.
- Higher-income Part D enrollees also pay higher monthly Part B premiums.
- Centers for Medicare & Medicaid Services, Medicare Advantage, Cost, PACE, Demo, and Prescription Drug Plan Contract Report – Monthly Summary Report (Data as of August 2017).
- Board of Trustees, 2017 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, Table IV.B7, available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2017.pdf.
- Social Security Act, Section 1860D-11(i).
- 2017 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds; Table IV.B9.
- Kaiser Family Foundation analysis of aggregate Part D reimbursement amounts from Table IV.B10, 2017 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds.
- Kaiser Family Foundation analysis of Part D average per beneficiary costs from Table V.D1, 2017 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds.
- Kaiser Family Foundation analysis of Part D benefits spending as a share of net Medicare outlays (total mandatory and discretionary outlays minus offsetting receipts) from CBO, Medicare-Congressional Budget Office’s June 2017 Baseline.
Read the full article here.
Source:
Kaiser Family Foundation (2 October 2017). “The Medicare Part D Prescription Drug Benefit” [Web Blog Post]. Retrieved from address https://www.kff.org/medicare/fact-sheet/the-medicare-prescription-drug-benefit-fact-sheet/#26740
Absent federal action, states take the lead on curbing drug costs
What's your state's stance on the cost of prescription drugs? See how Maryland has moved forward in their decision making for drug prices, giving themselves the ability to say "no" in this article from Benefits Pro written by Shefali Luthra.
You can read the original article here.
Lawmakers in Maryland are daring to legislate where their federal counterparts have not: As of Oct. 1, the state will be able to say “no” to some pharmaceutical price spikes.
A new law, which focuses on generic and off-patent drugs, empowers the state’s attorney general to step in if a drug’s price climbs 50 percent or more in a single year. The company must justify the hike. If the attorney general still finds the increase unwarranted, he or she can file suit in state court. Manufacturers face a fine of up to $10,000 for price gouging.
As Congress stalls on what voters say is a top health concern — high pharmaceutical costs — states increasingly are tackling the issue. Despite often-fierce industry opposition, a variety of bills are working their way through state governments. California, Nevada and New York are among those joining Maryland in passing legislation meant to undercut skyrocketing drug prices.
Maryland, though, is the first to penalize drugmakers for price hikes. Its law passed May 26 without the governor’s signature.
The state-level momentum raises the possibility that — as happened with hot-button issues such as gay marriage and smoke-free buildings — a patchwork of bills across the country could pave the way for more comprehensive national action. States feel the squeeze of these steep price tags in Medicaid and state employee benefit programs, and that applies pressure to find solutions.
“There is a noticeable uptick among state legislatures and state governments in terms of what kind of role states can play in addressing the cost of prescription drugs and access,” said Richard Cauchi, health program director at the National Conference of State Legislatures.
Many experts frame Maryland’s law as a test case that could help define what powers states have and what limits they face in doing battle with the pharmaceutical industry.
The generic-drug industry has already filed a lawsuit to block the law, arguing it’s unconstitutionally vague and an overreach of state powers. A district court is expected to rule soon.
The state-level actions focus on a variety of tactics:
“Transparency bills” would require pharmaceutical companies to detail a drug’s production and advertising costs when they raise prices over certain thresholds. Cost-limit measures would cap drug prices charged by drugmakers to Medicaid or other state-run programs, or limit what the state will pay for drugs. Supply-chain restrictions include regulating the roles of pharmacy benefit managers or limiting a consumer’s out-of-pocket costs.
A New York law on the books since spring allows officials to cap what its Medicaid program will pay for medications. If companies don’t sufficiently discount a drug, a state review will assess whether the price is out of step with medical value.
Maryland’s measure goes further — treating price gouging as a civil offense and taking alleged violators to court.
“It’s a really innovative approach. States are looking at how to replicate it, and how to expand on it,” said Ellen Albritton, a senior policy analyst at the left-leaning Families USA, which has consulted with states including Maryland on such policies.
Lawmakers have introduced similar legislation in states such as Massachusetts, Rhode Island, Tennessee and Montana. And in Ohio voters are weighing a ballot initiative in November that would limit what the state pays for prescription drugs in its Medicaid program and other state health plans.
Meanwhile, the California legislature passed a bill earlier in September that would require drugmakers to disclose when they are about to raise a price more than 16 percent over two years and justify the hike. It awaits Democratic Gov. Jerry Brown’s signature.
In June, Nevada lawmakers approved a law similar to California’s but limited to insulin prices. Vermont passed a transparency law in 2016 that would scrutinize up to 15 drugs for which the state spends “significant health care dollars” and prices had climbed by set amounts in recent years.
But states face a steep uphill climb in passing pricing legislation given the deep-pocketed pharmaceutical industry, which can finance strong opposition, whether through lobbying, legal action or advertising campaigns.
Last fall, voters rejected a California initiative that would have capped what the state pays for drugs — much like the Ohio measure under consideration. Industry groups spent more than $100 million to defeat it, putting it among California’s all-time most expensive ballot fights. Ohio’s measure is attracting similar heat, with drug companies outspending opponents about 5-to-1.
States also face policy challenges and limits to their statutory authority, which is why several have focused their efforts on specific parts of the drug-pricing pipeline.
Critics see these tailored initiatives as falling short or opening other loopholes. Requiring companies to report prices past a certain threshold, for example, might encourage them to consistently set prices just below that level.
Maryland’s law is noteworthy because it includes a fine for drugmakers if price increases are deemed excessive — though in the industry that $10,000 fine is likely nominal, suggested Rachel Sachs, an associate law professor at Washington University in St. Louis who researches drug regulations.
This law also doesn’t address the trickier policy question: a drug’s initial price tag, noted Rena Conti, an assistant professor in the University of Chicago who studies pharmaceutical economics.
And its focus on generics means that branded drugs, such as Mylan’s Epi-Pen or Kaleo’s overdose-reversing Evzio, wouldn’t be affected.
Yet there’s a good reason for this, noted Jeremy Greene, a professor of medicine and the history of medicine at Johns Hopkins University who is in favor of Maryland’s law.
Current interpretation of federal patent law suggests that the issues related to the development and affordability of on-patent drugs are under federal jurisdiction, outside the purview of states, he explained.
In Maryland, “the law was drafted narrowly to address specifically a problem we’ve only become aware of in recent years,” he said. That’s the high cost of older, off-patent drugs that face little market competition. “Here’s where the state of Maryland is trying to do something,” he said.
Still, a ruling against the state in the pending court case could have a chilling effect for other states, Sachs said, although it would be unlikely to quash their efforts.
“This is continuing to be a topic of discussion, and a problem for consumers,” said Sachs.
“At some point, some of these laws are going to go into effect — or the federal government is going to do something,” she added.
Kaiser Health News, a nonprofit health newsroom whose stories appear in news outlets nationwide, is an editorially independent part of the Kaiser Family Foundation. KHN’s coverage of prescription drug development, costs and pricing is supported in part by the Laura and John Arnold Foundation.
Source:
Luther S. (29 September 2017). "Absent federal action, states take the lead on curbing drug costs" [Web Blog Post]. Retrieved from address https://www.benefitspro.com/2017/09/29/absent-federal-action-states-take-the-lead-on-curb?page=2
5 Crucial Wellness Strategies for Self-Funded Companies
In the article below from Care ATC, you will learn the importance of health care coverage - self-funded or not - and how to leverage different programs to the benefit of your company and its employees. Explore these five strategies for self-insured companies and find what will work best for you.
You can read the original article here.
Instead of paying pricy premiums to insurers, self-insured companies pay claims filed by employees and health care providers directly and assume most of the financial risk of providing health benefits to employees. To mitigate significant losses, self-funded companies often sign up for a special “stop loss” insurance, hedging against very large or unexpected claims. The result? A stronger position to stabilize health care costs in the long-term. No wonder self-funded plans are on the rise with nearly 81% of employees at large companies covered.
Despite the rise in self-insured companies, employers are uncertain as to whether they’ll even be able to afford coverage in the long-term given ACA regulations. Now more than ever, employers (self-insured or not) must understand that wellness is a business strategy. High-performing companies are able to manage costs by implementing the most effective tactics for improving workforce health.
Here are five wellness strategies for self-insured companies:
Strategy 1: Focus on Disease Management Programs
Corporate wellness offerings generally consist of two types of programs: lifestyle management and disease management. The first focuses on employees with health risks, like smoking or obesity, and supports them in reducing those risks to ultimately prevent the development of chronic conditions. Disease management programs, on the other hand, are designed to help employees who already have chronic disease, encouraging them to take better care of themselves through increased access to low-cost generic prescriptions or closing communication gaps in care through periodic visits to providers who leverage electronic medical records.
According to a 2012 Rand Corporation study, both program types collectively reduced the employer’s average health care costs by about $30 per member per month (PMPM) with disease management responsible for 87% of those savings. You read that right – 87%! Looking deeper into the study, employees participating in the disease management program generated savings of $136 PMPM, driven in large part by a nearly 30% reduction in hospital admissions. Additionally, only 13% of employees participated in the disease management program, compared with 87% for the lifestyle management program. In other words, higher participation in lifestyle management programs marginally contributes to overall short-term savings; ROI was $3.80 for disease management but only $0.50 for lifestyle management for every dollar invested.
This isn’t to say that lifestyle management isn’t a worthy cause – employers still benefit from its long-term savings, reduced absenteeism, and improved retention rates – but it cannot be ignored that short-term ROI is markedly achieved through a robust disease management program.
Strategy 2: Beef Up Value-Based Benefits
Value-Based Benefit Design (VBD) strategies focus on key facets of the health care continuum, including prevention and chronic disease management. Often paired with wellness programs, VBD strategies aim to maximize opportunities for employees make positive changes. The result? Improved employee health and curbed health care costs for both employee and employer. Types of value-based benefits outlined by the National Business Coalition on Health include:
Individual health competency where incentives are presented most often through cash equivalent or premium differential:
Health Risk Assessment
Biometric testing
Wellness programs
Condition management where incentives are presented most often through co-pay/coinsurance differential or cash equivalent:
Adherence to evidence-based guidelines
Adherence to chronic medications
Participation in a disease management program
Provider Guidance
Utilization of a retail clinic versus an emergency room
Care through a “center of excellence”
Tier one high quality physician
There is no silver bullet when it comes to VBD strategies. The first step is to assess your company’s health care utilization and compare it with other benchmarks in your industry or region. The ultimate goal is to provide benefits that meet employee needs and coincide with your company culture.
Strategy 3: Adopt Comprehensive Biometric Screenings
Think Health Risk Assessments (HRAs) and Biometric Screenings are one and the same? Think again. While HRAs include self-reported questions about medical history, health status, and lifestyle, biometric screenings measure objective risk factors, such as body weight, cholesterol, blood pressure, stress, and nutrition. This means that by adopting a comprehensive annual biometric screening, employees can review results with their physician, create an action plan, and see their personal progress year after year. For employers, being able to determine potentially catastrophic claims and quantitatively assess employee health on an aggregate level is gold. With such valuable metrics, its no surprise that nearly 51% of large companies offer biometric screenings to their employees.
Strategy 4: Open or Join an Employer-Sponsored Clinic
Despite a moderate health care cost trend of 4.1% after ACA changes in 2013, costs continue to rise above the rate of inflation, amplifying concerns about the long-term ability for employers to provide health care benefits. In spite of this climate, there are still high-performing companies managing costs by implementing the most effective tactics for improving health. One key tactic? Offer at least one onsite health service to your population.
I know what you’re thinking: employer-sponsored clinics are expensive and only make sense for large companies, right? Not anymore. There are a few innovative models out there tailored to small and mid-size businesses that are self-funded, including multi-employer, multi-site sponsored clinics. Typically a large company anchors the clinic and smaller employers can join or a group of small employers can launch their very own clinic. There are a number of advantages to employer-sponsored clinics and it is worthwhile to explore if this strategy is right for your company.
Strategy 5: Leverage Mobile Technology
With thousands health and wellness apps currently available through iOS and Android, consumers are presented with an array of digital tools to achieve personal goals. So how can self-insured companies possibly leverage this range of mobile technology? From health gamification and digital health coaching, to wearables and apps, employers are inundated with a wealth of digital means that delivering a variation of virtually the same thing: measurable data. A few start-ups, including JIFF and SocialWellth, have entered the field to help employers evaluate and streamline digital wellness offerings.
These companies curate available consumer health and wellness technology to empower employers by simplifying the process of selecting and managing various app and device partners, and even connecting with tools employees are already be using.
Conclusion:
Self-insured companies have a vested interest in improving employee health and understand that wellness is indeed a business strategy. High-performing companies are able to manage costs by implementing the most effective tactics for improving workforce health including an increased focus on Chronic Disease Management programs; strengthening value-based benefit design; adopting comprehensive biometric screening; exploring the option of opening or joining an employer-sponsored clinic; and leveraging mobile technology.
Which strategies or tactics are you considering to implement in 2015?
Source:
Spears, T. (2014 December 19). 5 Crucial Wellness Strategies for Self-Funded Companies[Web blog post]. Retrieved from https://www.careatc.com/ehs/5-wellness-strategies-for-self-funded-companies
Workers Overwhelmed by Health Care Decisions
Employees are feeling the stress of healthcare costs. In the article below by Jack Craver, he provides insight as to the pressures workers are currently dealing with in todays healthcare marketplace.
Original Post from BenefitsPro.com on July 29, 2016
In case you haven’t noticed, Americans are in a tough spot on health care.
For one, their health care costs far more than that in any other country. Even worse, perhaps, they increasingly have many more decisions to make about how to pay for that care.
A new report demonstrates the frustration and hopelessness that grips so many in the face of health care decisions.
The study by Alegeus, the benefit account platform, surveyed 4,000 adults about their health care choices. It showed that there are seldom health or insurance-related choices that Americans make with relative ease or comfort.
There are no health care finance decisions, for instance, that a majority of Americans don’t find challenging. At the top of the list was “planning for out-of-pocket costs,” which two-thirds of respondents say they found either challenging or very challenging. Fifty-five percent say the same about choosing health care benefits.
Fifty-two percent said they found “maintaining health and wellness” challenging. If respondents are being completely honest with themselves (and the pollster), that figure would probably be much higher, considering that three-quarters of Americans are overweight or obese, and a certain percentage of those who aren’t still engage in unhealthy habits, such as problem drinking, substance abuse, or smoking.
One of the reasons health care is so expensive, many argue, is that for so long, Americans have been shielded from the true cost of care by generous employer-based insurance policies. As employers increasingly shift to high-deductible plans or consumer-driven health plans, millions of Americans are for the first time confronting decisions that in the past were left to higher-ups.
Alegeus CEO Steve Auerbach explained the shifting dynamics of health care shopping to BenefitsPRO.
“In the past, with health plans paying for the majority of health care costs, consumers have been conditioned to be disengaged,” he says. “This shift to consumer directed health care represents a complete paradigm shift in how consumers will need to manage their healthcare going forward — and there is a sizeable percentage of consumers who are resistant to this change. It is definitely going to take time for consumers to acclimate, build confidence, and rise to the occasion.”
He noted, however, that a similar “paradigm shift” took place with retirement benefits two decades ago, as many companies moved from defined-benefit pensions to 401(k)s.
“The infrastructure for education and support had to be built, and consumers had to adapt,” he says. “But now 401(k)s have become ubiquitous.”
See the original article here.
Source:
Craver, J. (2016, July 29). Workers overwhelmed by health care decisions [Web log post]. Retreived from https://www.benefitspro.com/2016/07/29/workers-overwhelmed-by-health-care-decisions?kw=Workers%20overwhelmed%20by%20health%20care%20decisions&cn=20160801&pt=Daily&src=EMC-Email&et=editorial&bu=BenefitsPRO&slreturn=1470060827
Core Benefits Drive Satisfaction More Than Niche Offerings
Original Post from SHRM.org
By: Stephen Miller
Improving traditional core benefits could be the best way to increase employees’ satisfaction with their rewards mix, new research suggests.
The three offerings with the greatest effect on how employees rate their benefits are health insurance, 401(k) retirement plans and vacation/paid time off. Among these, health insurance was by far the biggest driver of employee satisfaction, according to a new study, Which Benefits Drive Employee Satisfaction?, from Glassdoor Economic Research, the research arm of career website Glassdoor.
At organizations where employee ratings of the employer-provided health coverage increased by 1 star (out of 5), there was also a statistically significant increase in average employee satisfaction with the overall benefits package. (See graph above, from Glassdoor Economic Research. *Denotes that the increase in the overall benefits rating was statistically significant.)
Notably, 4 in 5 U.S. workers report they prefer new benefits or perks to a pay raise. This finding supports a recent Glassdoor survey that found health insurance, paid time off and 401(k) plans are among the top benefits employees would prefer over a pay increase.
Benefits with Narrower Appeal
Two benefits that did not seem to have a significant impact on overall employee satisfaction were maternity/paternity leave and employee discounts.
“Though many employers have added generous maternity/paternity leave plans, it is possible benefits that are not used by a large subset of employees do not impact overall benefits package satisfaction,” the researchers suggested.
“We know benefits and perks are an important recruiting tool in today’s challenging hiring landscape, and this study shows that the flashiest or trendy benefits aren’t always better,” said Andrew Chamberlain, chief economist of Glassdoor. “Investing in core benefits programs like health care coverage, retirement plans and paid time off will go far with new and current employees. Other benefits, like maternity/paternity leave, are important to recruit and retain smaller subsets of employees—like new parents—though we saw little impact on overall satisfaction related to benefits that don’t touch a wide variety of employees.”
He advised, “Employers who have well-rounded compensation plans that include core benefits, fair and competitive pay, and desirable perks stand to attract and retain top talent.”
A separate Glassdoor Economic Research study, The Best Industries for Benefits, found that the best benefits packages, according to employees, are found in the finance and technology industries.
Stephen Miller, CEBS, is an online editor/manager for SHRM. Follow him on Twitter @SHRMsmiller.
5 Crucial Wellness Strategies for Self-Funded Companies
Originally posted on CareATC.com
Instead of paying pricy premiums to insurers, self-insured companies pay claims filed by employees and health care providers directly and assume most of the financial risk of providing health benefits to employees. To mitigate significant losses, self-funded companies often sign up for a special “stop loss” insurance, hedging against very large or unexpected claims. The result? A stronger position to stabilize health care costs in the long-term. No wonder self-funded plans are on the rise with nearly 81% of employees at large companies covered.
Despite the rise in self-insured companies, employers are uncertain as to whether they’ll even be able to afford coverage in the long-term given ACA regulations. Now more than ever, employers (self-insured or not) must understand that wellness is a business strategy. High-performing companies are able to manage costs by implementing the most effective tactics for improving workforce health.
Here are five wellness strategies for self-insured companies:
Strategy 1: Focus on Disease Management Programs
Corporate wellness offerings generally consist of two types of programs: lifestyle management and disease management. The first focuses on employees with health risks, like smoking or obesity, and supports them in reducing those risks to ultimately prevent the development of chronic conditions. Disease management programs, on the other hand, are designed to help employees who already have chronic disease, encouraging them to take better care of themselves through increased access to low-cost generic prescriptions or closing communication gaps in care through periodic visits to providers who leverage electronic medical records.
According to a 2012 Rand Corporation study, both program types collectively reduced the employer’s average health care costs by about $30 per member per month (PMPM) with disease management responsible for 87% of those savings. You read that right – 87%! Looking deeper into the study, employees participating in the disease management program generated savings of $136 PMPM, driven in large part by a nearly 30% reduction in hospital admissions. Additionally, only 13% of employees participated in the disease management program, compared with 87% for the lifestyle management program. In other words, higher participation in lifestyle management programs marginally contributes to overall short-term savings; ROI was $3.80 for disease management but only $0.50 for lifestyle management for every dollar invested.
This isn’t to say that lifestyle management isn’t a worthy cause – employers still benefit from its long-term savings, reduced absenteeism, and improved retention rates – but it cannot be ignored that short-term ROI is markedly achieved through a robust disease management program.
Strategy 2: Beef Up Value-Based Benefits
Value-Based Benefit Design (VBD) strategies focus on key facets of the health care continuum, including prevention and chronic disease management. Often paired with wellness programs, VBD strategies aim to maximize opportunities for employees make positive changes. The result? Improved employee health and curbed health care costs for both employee and employer. Types of value-based benefits outlined by the National Business Coalition on Health include:
Individual health competency where incentives are presented most often through cash equivalent or premium differential:
- Health Risk Assessment
- Biometric testing
- Wellness programs
Condition management where incentives are presented most often through co-pay/coinsurance differential or cash equivalent:
- Adherence to evidence-based guidelines
- Adherence to chronic medications
- Participation in a disease management program
Provider Guidance
- Utilization of a retail clinic versus an emergency room
- Care through a “center of excellence”
- Tier one high quality physician
There is no silver bullet when it comes to VBD strategies. The first step is to assess your company’s health care utilization and compare it with other benchmarks in your industry or region. The ultimate goal is to provide benefits that meet employee needs and coincide with your company culture.
Strategy 3: Adopt Comprehensive Biometric Screenings
Think Health Risk Assessments (HRAs) and Biometric Screenings are one and the same? Think again. While HRAs include self-reported questions about medical history, health status, and lifestyle, biometric screenings measure objective risk factors, such as body weight, cholesterol, blood pressure, stress, and nutrition. This means that by adopting a comprehensive annual biometric screening, employees can review results with their physician, create an action plan, and see their personal progress year after year. For employers, being able to determine potentially catastrophic claims and quantitatively assess employee health on an aggregate level is gold. With such valuable metrics, its no surprise that nearly 51% of large companies offer biometric screenings to their employees.
Strategy 4: Open or Join an Employer-Sponsored Clinic
Despite a moderate health care cost trend of 4.1% after ACA changes in 2013, costs continue to rise above the rate of inflation, amplifying concerns about the long-term ability for employers to provide health care benefits. In spite of this climate, there are still high-performing companies managing costs by implementing the most effective tactics for improving health. One key tactic? Offer at least one onsite health service to your population.
I know what you’re thinking: employer-sponsored clinics are expensive and only make sense for large companies, right? Not anymore. There are a few innovative models out there tailored to small and mid-size businesses that are self-funded, including multi-employer, multi-site sponsored clinics. Typically a large company anchors the clinic and smaller employers can join or a group of small employers can launch their very own clinic. There are a number of advantages to employer-sponsored clinics and it is worthwhile to explore if this strategy is right for your company.
Strategy 5: Leverage Mobile Technology
With thousands health and wellness apps currently available through iOS and Android, consumers are presented with an array of digital tools to achieve personal goals. So how can self-insured companies possibly leverage this range of mobile technology? From health gamification and digital health coaching, to wearables and apps, employers are inundated with a wealth of digital means that delivering a variation of virtually the same thing: measurable data. A few start-ups, including JIFF and SocialWellth, have entered the field to help employers evaluate and streamline digital wellness offerings.
These companies curate available consumer health and wellness technology to empower employers by simplifying the process of selecting and managing various app and device partners, and even connecting with tools employees are already be using.
Conclusion:
Self-insured companies have a vested interest in improving employee health and understand that wellness is indeed a business strategy. High-performing companies are able to manage costs by implementing the most effective tactics for improving workforce health including an increased focus on Chronic Disease Management programs; strengthening value-based benefit design; adopting comprehensive biometric screening; exploring the option of opening or joining an employer-sponsored clinic; and leveraging mobile technology.
Which strategies or tactics are you considering to implement in 2017?






